What does Medicare Part cover in skilled nursing facilities?
Yes, Medicare Part A insurance will cover skilled nursing facilities (SNF) and inpatient hospital stays, hospice care, and some home health care. The SNF will cover any DME equipment needed for patients for up to 100 days. An SNF is a facility with skilled nursing care staff, rehabilitative services, and other related health services.
Does Medicare cover SNF care?
Skilled care provided in a skilled nursing facility (SNF) is covered by Medicare. Custodial care may also be covered is a Medicare, but only if the beneficiary is also receiving skilled nursing care.
What in-home care will Medicare cover?
In Home Care Medicare will cover skilled nursing care in the home for a limited time period, but not non-medical care. Care must be prescribed by a doctor and needed part-time only. The senior must be "confined", meaning they are unable to leave the home without the assistance of another person. This is formally referred to as " homebound ".
Does Medicare cover skilled nursing facilities?
Yes, Medicare covers skilled nursing care, but only under certain conditions and only for a limited time. Medicare Part A covers inpatient hospital care, and it also covers home health care and hospice care. It covers skilled nursing care, too, but it only covers short-term stays at skilled nursing facilities if you meet the following conditions:
What part of Medicare does SNF fall under?
Part APart A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Care like intravenous injections that can only be given by a registered nurse or doctor. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services.
What does SNF mean in Medicare?
SKILLED NURSING FACILITY201.2. Definitions. 201. SKILLED NURSING FACILITY (SNF) DEFINED. An SNF is an institution or a distinct part of an institution (see §201.1), such as a skilled nursing.
What services are included in Medicare Part A?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
What are the four parts of Medicare and what is included in each?
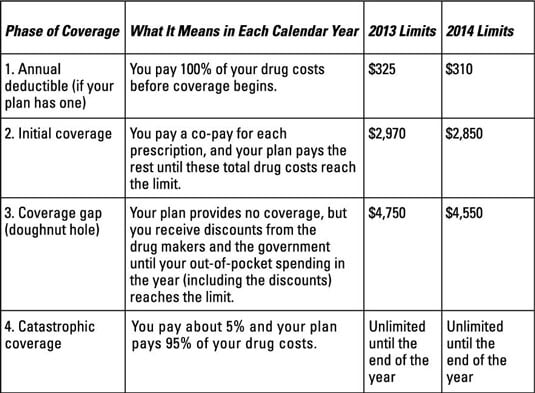
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Which part of Medicare covers SNF services quizlet?
Medicare Part A provides coverage for skilled nursing facilities (SNF) care after a three-day inpatient hospital stay for an illness or injury requiring SNF care. Covered SNF expenses include: semi-private room, meals, skilled nursing services, and rehabilitation.
What is the difference between SNF and NF?
A nursing home or long-term care facility is normally dual certified with designated SNF (Skilled Nursing Facility) or rehabilitation beds and NF (Nursing Facility) or long-term care beds. In other words, the same health center can be both a SNF and an NF.
What is covered by Medicare Part C?
Medicare Part C outpatient coveragedoctor's appointments, including specialists.emergency ambulance transportation.durable medical equipment like wheelchairs and home oxygen equipment.emergency room care.laboratory testing, such as blood tests and urinalysis.occupational, physical, and speech therapy.More items...
What is Medicare Part C called?
A Medicare Advantage is another way to get your Medicare Part A and Part B coverage. Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are offered by Medicare-approved private companies that must follow rules set by Medicare.
Whats the difference between Medicare Part A and B?
Part A is hospital coverage, while Part B is more for doctor's visits and other aspects of outpatient medical care. These plans aren't competitors, but instead are intended to complement each other to provide health coverage at a doctor's office and hospital.
What is the difference between Part C and Part D Medicare?
Medicare Part C is an alternative to original Medicare. It must offer the same basic benefits as original Medicare, but some plans also offer additional benefits, such as vision and dental care. Medicare Part D, on the other hand, is a plan that people can enroll in to receive prescription drug coverage.
What is Medicare Part F?
Medigap Plan F is a Medicare Supplement Insurance plan that's offered by private companies. It covers "gaps" in Original Medicare coverage, such as copayments, coinsurance and deductibles. Plan F offers the most coverage of any Medigap plan, but unless you were eligible for Medicare by Dec.
What is Medicare Part B mean?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services. Part B also covers some preventive services. Look at your Medicare card to find out if you have Part B.
What happens if you leave SNF?
If you stop getting skilled care in the SNF, or leave the SNF altogether, your SNF coverage may be affected depending on how long your break in SNF care lasts.
How long does a break in skilled care last?
If your break in skilled care lasts for at least 60 days in a row, this ends your current benefit period and renews your SNF benefits. This means that the maximum coverage available would be up to 100 days of SNF benefits.
Does Medicare cover skilled nursing?
Medicare covers skilled nursing facility (SNF) care. There are some situations that may impact your coverage and costs.
Can you be readmitted to the hospital if you are in a SNF?
If you're in a SNF, there may be situations where you need to be readmitted to the hospital. If this happens, there's no guarantee that a bed will be available for you at the same SNF if you need more skilled care after your hospital stay. Ask the SNF if it will hold a bed for you if you must go back to the hospital.
What happens after day 100 of SNF?
After day 100, there is no Medicare coverage for a SNF and you would be responsible for all costs. If you have a break in SNF care that lasts 60 days or more, your benefit period would reset. This means that Medicare coverage for SNF benefits is reset, and the maximum coverage available would be 100 days for a new stay in a SNF.
Is skilled nursing covered by Medicare?
Your reason for needing skilled care in a SNF must be related to the qualifying hospital stay or be the result of a condition that started while you were hospitalized or getting care in a SNF. If you meet the above criteria, your stay in a SNF would be Medicare-covered.
Does Medicare cover nursing home stays?
Medicare Part A provides coverage for a Medicare-covered skilled nursing facility stay. However, this does not mean that you are covered at 100% for all costs indefinitely. As with other parts of Medicare and other services, there are some out-of-pocket costs.
Does Medicare cover SNF?
We follow strict editorial standards to give you the most accurate and unbiased information. Coverage for skilled nursing facilities (also known as SNFs for short) is provided by Medicare Part A. Medicare includes coverage in a SNF under certain situations for limited time periods. It is crucial that you understand what those conditions ...
How long do you have to stay in a skilled nursing facility to get a break?
If you leave the SNF for less than 30 days and then return, you don’t need another qualifying hospital visit.
How long does a skilled nursing stay in a hospital last?
Your hospital visit must last for at least three days of inpatient care.
Does Medicare cover skilled nursing?
Your Medicare insurance doesn’t provide unlimited coverage for skilled nursing facilities. The first 20 days of treatment in a given benefit period receive full coverage. For any days falling between 21 and 100 days of treatment in the facility, you’re responsible for a $170.50 co-payment per day. You’re responsible for the full cost for any days of treatment beyond 100 days. If you are enrolled in a Medicare Advantage plan, you will have at least the same Part A and Part B benefits as Original Medicare, but many include additional benefits.
Is a three day visit to the hospital considered inpatient?
Not every visit to the hospital, even one where you stay for three days, is a qualifying visit. Doctors frequently admit patients for a day of observation, rather than treatment. The day of observation doesn’t qualify as inpatient care. The three-day clock only begins when your doctor formally admits you for inpatient treatment.
Can you receive treatment for a condition you develop during your stay at a skilled nursing facility?
The medical condition that you get treatment for must also be a condition treated during your hospital stay. You can also receive treatment for a condition you develop during your stay at a skilled nursing facility that’s related to your original condition. A post-operation infection, for example, would likely qualify.
How long is a SNF stay?
A person has a 60 day benefit period that applies to both hospital and SNF stays. Once a person has been discharged from the hospital or SNF for 60 days, a new admission will result in a new benefit period. This means they are eligible for another 100 days of SNF care covered by Medicare after a qualifying hospital stay.
What happens if you don't meet the SNF requirement?
If the person does not meet Medicare’s requirement for the SNF or the person has reached their 100-day limit, Medicaid may be able to offer help if the person is eligible.
Does Medicare cover outpatient therapy?
Post-100 days, Medicare may continue to cover some medically necessary skilled therapy services while the person is in an SNF, but the person will still have to pay out of pocket for the room & board costs . Some individuals can see if they qualify for at-home therapy through Medicare’s home health benefit. Also, when a patient can receive outpatient therapy safely, different coverage options will apply.
What is the SNF?
The SNF must provide you with a written description of your legal rights. Keep the information you get about your rights, admission and transfer policies, and any other information you get from the SNF in case you need to look at them later. As a person with Medicare, you have certain guaranteed rights and protections.
What are the rights of SNF?
You have the right to privacy, and to keep and use your personal belongings and property as long as they don't interfere with the rights, health, or safety of others. SNF staff should never open your mail unless you allow it. You have the right to use a phone and talk privately. The SNF must protect your property from theft. This may include a safe in the facility or cabinets with locked doors in resident rooms. If you and your spouse live in the same SNF, you're entitled to share a room (if you both agree to do so).
How does SNF work?
However, the SNF must allow you access to your bank accounts, cash, and other financial records. The SNF must place your money (over $50) in an account that provides interest, and they must give you quarterly statements. The SNF must protect your funds from any loss by buying a bond or providing other similar protections.
What are the rights of a person in a nursing home?
You have the right to be treated with dignity and respect. You have the right to choose the activities you want to go to. As long as it fits your care plan, you have the right to make your own schedule, including when you: Go to bed. Rise in the morning. Eat your meals.
Do SNFs have to develop a care plan?
By law, SNFs must develop a plan of care (care plan) for each resident. You have the right to take part in this process and family members can help with your care plan with your permission. If your relative is your legal guardian, he or she has the right to look at all medical records about you.
Do SNFs have to accept all applicants?
Freedom from discrimination. SNFs don't have to accept all applicants, but they must comply with Civil Rights laws that don't allow discrimination based on these: If you believe you've been discriminated against, contact the Department of Health and Human Services, Office for Civil Rights.
Can you be sent to another SNF?
You can't be sent to another SNF or made to leave the SNF, except in these situations: It's necessary for the welfare, health, or safety of you or others. Your health has declined to the point that the SNF can't meet your care needs. Your health has improved to the point that SNF care is no longer necessary.
