Which president signed Medicare into law?
In 1972, President Richard M. Nixon signed into the law the first major change to Medicare. The legislation expanded coverage to include individuals under the age of 65 with long-term disabilities and individuals with end-stage renal disease (ERSD).
Which president passed the GI Bill?
Feb 14, 2018 · Those making more than $500,000 a year ($750,000 for couples) will pay 85 percent of the actual costs of Part B and D in 2019, up from 80 percent this year. Most Medicare enrollees pay premiums ...
What president is responsible for Medicaid?
Feb 17, 2020 · Richard Nixon – By the 1970’s health care was a required part of any campaign for federal office, with all candidates having their own health reform proposal. However, it was Richard Nixon that...
What president started Medicare program?
May 22, 2020 · Trump Administration Announces Changes to Medicare Advantage and Part D to Provide Better Coverage and Increase Access for Medicare Beneficiaries May 22, …
Which president changed Medicare?
Medicare's history: Key takeaways President Lyndon B. Johnson signed Medicare into law in 1965.
Which president signed Medicare legislation?
President Lyndon B. JohnsonOn July 30, 1965, President Lyndon B. Johnson signed the Medicare and Medicaid Act, also known as the Social Security Amendments of 1965, into law. It established Medicare, a health insurance program for the elderly, and Medicaid, a health insurance program for people with limited income.Feb 8, 2022
Who was the first American president to make an appeal for national health insurance?
Harry Truman, who became President upon FDR's death in 1945, considered it his duty to perpetuate Roosevelt's legacy. In 1945, he became the first president to propose national health insurance legislation.
How did President Johnson reform the healthcare system?
Medicaid, a state and federally funded program that offers health coverage to certain low-income people, was also signed into law by President Johnson on July 30, 1965, as an amendment to the Social Security Act.
Which president started Medicare and Social Security?
President Johnson signing the Medicare program into law, July 30, 1965.
What President created Medicare and Medicaid?
President Lyndon B. JohnsonOn July 30, 1965, President Lyndon B. Johnson signed the Social Security Amendments of 1965 into law. With his signature he created Medicare and Medicaid, which became two of America's most enduring social programs. The signing ceremony took place in Independence, Missouri, in the presence of former President Harry S.
Which president first proposed Medicare?
On July 30, 1965, President Lyndon Johnson traveled to the Truman Library in Independence, Missouri, to sign Medicare into law. His gesture drew attention to the 20 years it had taken Congress to enact government health insurance for senior citizens after Harry Truman had proposed it.
What party was Harry Truman?
Democratic PartyHarry S. Truman / PartyThe Democratic Party is one of the two major contemporary political parties in the United States. It was founded in 1828 by supporters of Andrew Jackson, making it the world's oldest active political party. Since the 1860s, its main political rival has been the Republican Party. Wikipedia
Why did the American medical Association oppose Medicare in the 1950s and 1960s?
Said Edward Annis, MD, the AMA president who led the anti-Medicare fight in the early 1960s, "The AMA believed that anybody in this nation who needed medical care should have it when they need it for as long as they need it, whether they could pay for it or not." He and others of like mind predicted Medicare would be a ...Jul 30, 2015
What was the main reason that President Johnson and Congress added Medicare to the Great Society programs?
The special economic problem which stimulated the development of Medicare is that health costs increase greatly in old age when, at the same time, income almost always declines. The cost of adequate private health insurance, if paid for in old age, is more than most older persons can afford.
How did Medicare Part D expand Medicare services?
Part D was enacted as part of the Medicare Modernization Act of 2003 and went into effect on January 1, 2006. Under the program, drug benefits are provided by private insurance plans that receive premiums from both enrollees and the government.
What did Medicare do?
Medicare was enacted in July 1965 and implemented essentially nationwide in July 1966. It provided virtually universal public health insurance to individuals aged 65 and older (coverage for the disabled was added in 1973).
When will Medicare waive late enrollment penalties?
To help them with this transition, Medicare has waived late-enrollment penalties until the end of September.
How much is the penalty for Part D?
Right now, that’s roughly $30 a month, so the penalty would be 30 cents for each month you are late.
Who is Phil Moeller?
Phil Moeller is the author of “Get What’s Yours for Medicare: Maximize Your Coverage, Minimize Your Costs” and the co-author of the updated edition of The New York Times bestseller “How to Get What’s Yours: The Revised Secrets to Maxing Out Your Social Security,” with Making Sen$e’s Paul Solman and Larry Kotlikoff.
Will Medicare be repealed?
It’s a more significant if largely invisible change. Medicare’s caps on covered expenses for outpatient therapy have been officially repealed.
When did Medicare expand?
Over the years, Congress has made changes to Medicare: More people have become eligible. For example, in 1972 , Medicare was expanded to cover the disabled, people with end-stage renal disease (ESRD) requiring dialysis or kidney transplant, and people 65 or older that select Medicare coverage.
When did Medicare and Medicaid start?
On July 30, 1965 , President Lyndon B. Johnson signed into law legislation that established the Medicare and Medicaid programs. For 50 years, these programs have been protecting the health and well-being of millions of American families, saving lives, and improving the economic security of our nation.
What is Medicare Part D?
Medicare Part D Prescription Drug benefit. The Medicare Prescription Drug Improvement and Modernization Act of 2003 (MMA) made the biggest changes to the Medicare in the program in 38 years. Under the MMA, private health plans approved by Medicare became known as Medicare Advantage Plans.
When was the Children's Health Insurance Program created?
The Children’s Health Insurance Program (CHIP) was created in 1997 to give health insurance and preventive care to nearly 11 million, or 1 in 7, uninsured American children. Many of these children came from uninsured working families that earned too much to be eligible for Medicaid.
What is the Affordable Care Act?
The 2010 Affordable Care Act (ACA) brought the Health Insurance Marketplace, a single place where consumers can apply for and enroll in private health insurance plans. It also made new ways for us to design and test how to pay for and deliver health care.
Who signed Medicare and Medicaid into law?
It took only six months before he was able to travel to Independence, Missouri and sign Medicare and Medicaid into law next to former President Harry Truman. 4. Richard Nixon – By the 1970’s health care was a required part of any campaign for federal office, with all candidates having their own health reform proposal.
Who was the 32nd president of the United States?
But it wasn’t until his distant cousin, Franklin Delano Roosevelt (F.D.R.), the 32 nd President of the United States, that national health insurance was again at the forefront of a president’s mind – and campaign. F.D.R. was an advocate for mandatory health insurance in both the Social Security Act of 1935 and the Wagner National Health Act of 1939.
When did Medicare+Choice become Medicare Advantage?
These Part C plans were initially known in 1997 as "Medicare+Choice". As of the Medicare Modernization Act of 2003, most "Medicare+Choice" plans were re-branded as " Medicare Advantage " (MA) plans (though MA is a government term and might not even be "visible" to the Part C health plan beneficiary).
When did Medicare Part D start?
Medicare Part D went into effect on January 1, 2006. Anyone with Part A or B is eligible for Part D, which covers mostly self-administered drugs. It was made possible by the passage of the Medicare Modernization Act of 2003. To receive this benefit, a person with Medicare must enroll in a stand-alone Prescription Drug Plan (PDP) or public Part C health plan with integrated prescription drug coverage (MA-PD). These plans are approved and regulated by the Medicare program, but are actually designed and administered by various sponsors including charities, integrated health delivery systems, unions and health insurance companies; almost all these sponsors in turn use pharmacy benefit managers in the same way as they are used by sponsors of health insurance for those not on Medicare. Unlike Original Medicare (Part A and B), Part D coverage is not standardized (though it is highly regulated by the Centers for Medicare and Medicaid Services). Plans choose which drugs they wish to cover (but must cover at least two drugs in 148 different categories and cover all or "substantially all" drugs in the following protected classes of drugs: anti-cancer; anti-psychotic; anti-convulsant, anti-depressants, immuno-suppressant, and HIV and AIDS drugs). The plans can also specify with CMS approval at what level (or tier) they wish to cover it, and are encouraged to use step therapy. Some drugs are excluded from coverage altogether and Part D plans that cover excluded drugs are not allowed to pass those costs on to Medicare, and plans are required to repay CMS if they are found to have billed Medicare in these cases.
What is Medicare and Medicaid?
Medicare is a national health insurance program in the United States, begun in 1965 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, ...
How many people have Medicare?
In 2018, according to the 2019 Medicare Trustees Report, Medicare provided health insurance for over 59.9 million individuals —more than 52 million people aged 65 and older and about 8 million younger people.
When will Medicare cards be mailed out?
A sample of the new Medicare cards mailed out in 2018 and 2019 depending on state of residence on a Social Security database.
Who is Bruce Vladeck?
Bruce Vladeck, director of the Health Care Financing Administration in the Clinton administration, has argued that lobbyists have changed the Medicare program "from one that provides a legal entitlement to beneficiaries to one that provides a de facto political entitlement to providers."
What is CMS in healthcare?
The Centers for Medicare and Medicaid Services (CMS), a component of the U.S. Department of Health and Human Services (HHS), administers Medicare, Medicaid, the Children's Health Insurance Program (CHIP), the Clinical Laboratory Improvement Amendments (CLIA), and parts of the Affordable Care Act (ACA) ("Obamacare").
When will CMS change the star rating?
Additionally, CMS adopted a series of changes in the March 31, 2020, Interim Final Rule with Comment Period (CMS-1744-IFC) for the 2021 and 2022 Star Ratings to accommodate challenges arising from the COVID-19 public health emergency.
What is star rating?
The Star Ratings system helps people with Medicare, their families, and their caregivers compare the quality of health and drug plans being offered. One of the best indicators of a plan’s quality is how its enrollees feel about their coverage experience.
Does Medicare have telehealth?
The Centers for Medicare & Medicaid Services today finalized requirements that will increase access to telehealth for seniors in Medicare Advantage (MA) plans , expand the types of supplemental benefits available for beneficiaries with an MA plan who have chronic diseases, provide support for more MA options for beneficiaries in rural communities, and expand access to MA for patients with End Stage Renal Disease (ESRD). Together, the changes advance President Trump’s Executive Orders on Protecting and Improving Medicare for Our Nation’s Seniors and Advancing American Kidney Health as well as several of the CMS strategic initiatives.
Who signed Medicare into law?
President Johnson signs Medicare into law. On July 30, 1965, President Lyndon B. Johnson signs Medicare, a health insurance program for elderly Americans, into law. At the bill-signing ceremony, which took place at the Truman Library in Independence, Missouri, former President Harry Truman was enrolled as Medicare’s first beneficiary ...
When did Medicare become a federal program?
Medicaid, a state and federally funded program that offers health coverage to certain low-income people, was also signed into law by President Johnson on July 30 , 1965, ...
How many people were on Medicare in 1966?
Some 19 million people enrolled in Medicare when it went into effect in 1966. In 1972, eligibility for the program was extended to Americans under 65 with certain disabilities and people of all ages with permanent kidney disease requiring dialysis or transplant.
What would happen if the Trump administration changed Medicaid?
These changes would dramatically affect state budgets and could lead to significant cuts to benefits, coverage, and provider payments.
What is Medicaid waiver?
The Trump Administration issued guidance in January 2020 inviting states to seek demonstration projects — known as waivers — that would radically overhaul Medicaid coverage for adults. Under the guidance, states could apply for waivers that would convert their Medicaid programs for adults into a form of block grant, with capped federal funding and new authorities to cut coverage and benefits.
What are the new immigration rules?
The Department of Homeland Security (DHS) and the Department of State (DoS) issued immigration rules in 2019 that will make it much more difficult for people with low or modest means to immigrate to the United States or for people already here to gain permanent resident status or extend or modify their temporary status. These complicated rules, along with other Trump Administration policies, have led many families that include immigrants to forgo Medicaid and other assistance programs for which they’re eligible despite the fact that most people who qualify for the programs identified in the rules will not undergo the “public charge” assessment that the rules radically changed. Beginning February 24, 2020, DHS immigration officials will be able to reject immigration applicants if they have received, or are judged likely to receive in the future, any of an array of benefits, including Medicaid. Timing for the DoS implementation of the policy has not yet been announced.
What would happen if the poverty line was lowered?
By lowering the poverty line, that proposal would ultimately cut billions of dollars from federal health programs and cause millions of people to lose their eligibility for, or receive less help from, these programs. Many programs, including Medicaid and CHIP, use the poverty line to determine eligibility and benefits, and the cuts to these programs — and the numbers of people losing assistance altogether or receiving less help — would increase with each passing year. After ten years, more than 300,000 children would lose comprehensive coverage through Medicaid and CHIP, as would more than 250,000 adults covered through the ACA Medicaid expansion. Some pregnant women, low-income parents in non-expansion states, and people receiving family planning services through Medicaid would also lose coverage.
Will Trump repeal the Affordable Care Act?
President Trump has made clear that his goal remains to repeal the Affordable Care Act (ACA), including its expansion of Medicaid to low-income adults, and to impose rigid caps on the federal government’s Medicaid spending. While Congress considered and rejected a series of proposals to cut Medicaid and repeal the ACA in 2017, ...
When will Medicare Part D change to Advantage?
Some of them apply to Medicare Advantage and Medicare Part D, which are the plans that beneficiaries can change during the annual fall enrollment period that runs from October 15 to December 7.
How much will Medicare copay be in 2021?
The copay amounts for people who reach the catastrophic coverage level in 2021 will increase slightly, to $3.70 for generics and $9.20 for brand-name drugs. Medicare beneficiaries with Part D coverage (stand-alone or as part of a Medicare Advantage plan) will have access to insulin with a copay of $35/month in 2021.
What is the Medicare premium for 2021?
The standard premium for Medicare Part B is $148.50/month in 2021. This is an increase of less than $4/month over the standard 2020 premium of $144.60/month. It had been projected to increase more significantly, but in October 2020, the federal government enacted a short-term spending bill that included a provision to limit ...
Is Medicare Advantage available for ESRD?
Under longstanding rules, Medicare Advantage plans have been unavailable to people with end-stage renal disease (ESRD) unless there was an ESRD Special Needs Plan available in their area. But starting in 2021, Medicare Advantage plans are guaranteed issue for all Medicare beneficiaries, including those with ESRD. This is a result of the 21st Century Cures Act, which gives people with ESRD access to any Medicare Advantage plan in their area as of 2021.
Is there a donut hole in Medicare?
The Affordable Care Act has closed the donut hole in Medicare Part D. As of 2020, there is no longer a “hole” for brand-name or generic drugs: Enrollees in standard Part D plans pay 25 percent of the cost (after meeting their deductible) until they reach the catastrophic coverage threshold.
What is the maximum deductible for Part D?
For stand-alone Part D prescription drug plans, the maximum allowable deductible for standard Part D plans will be $445 in 2021, up from $435 in 2020. And the out-of-pocket threshold (where catastrophic coverage begins) will increase to $6,550 in 2021, up from $6,350 in 2020.
How much is the Part A deductible for 2021?
If the person needs additional inpatient coverage during that same benefit period, there’s a daily coinsurance charge. For 2021, it’s $371 per day for the 61st through 90th day of inpatient care (up from $352 per day in 2020).
Overview
Legislation and reform
• 1960: PL 86-778 Social Security Amendments of 1960 (Kerr-Mills aid)
• 1965: PL 89-97 Social Security Act of 1965, Establishing Medicare Benefits
• 1980: Medicare Secondary Payer Act of 1980, prescription drugs coverage added
History
Originally, the name "Medicare" in the United States referred to a program providing medical care for families of people serving in the military as part of the Dependents' Medical Care Act, which was passed in 1956. President Dwight D. Eisenhowerheld the first White House Conference on Aging in January 1961, in which creating a health care program for social security beneficiaries was p…
Administration
The Centers for Medicare and Medicaid Services (CMS), a component of the U.S. Department of Health and Human Services (HHS), administers Medicare, Medicaid, the Children's Health Insurance Program (CHIP), the Clinical Laboratory Improvement Amendments (CLIA), and parts of the Affordable Care Act (ACA) ("Obamacare"). Along with the Departments of Labor and Treasury, the CMS also implements the insurance reform provisions of the Health Insurance Portability an…
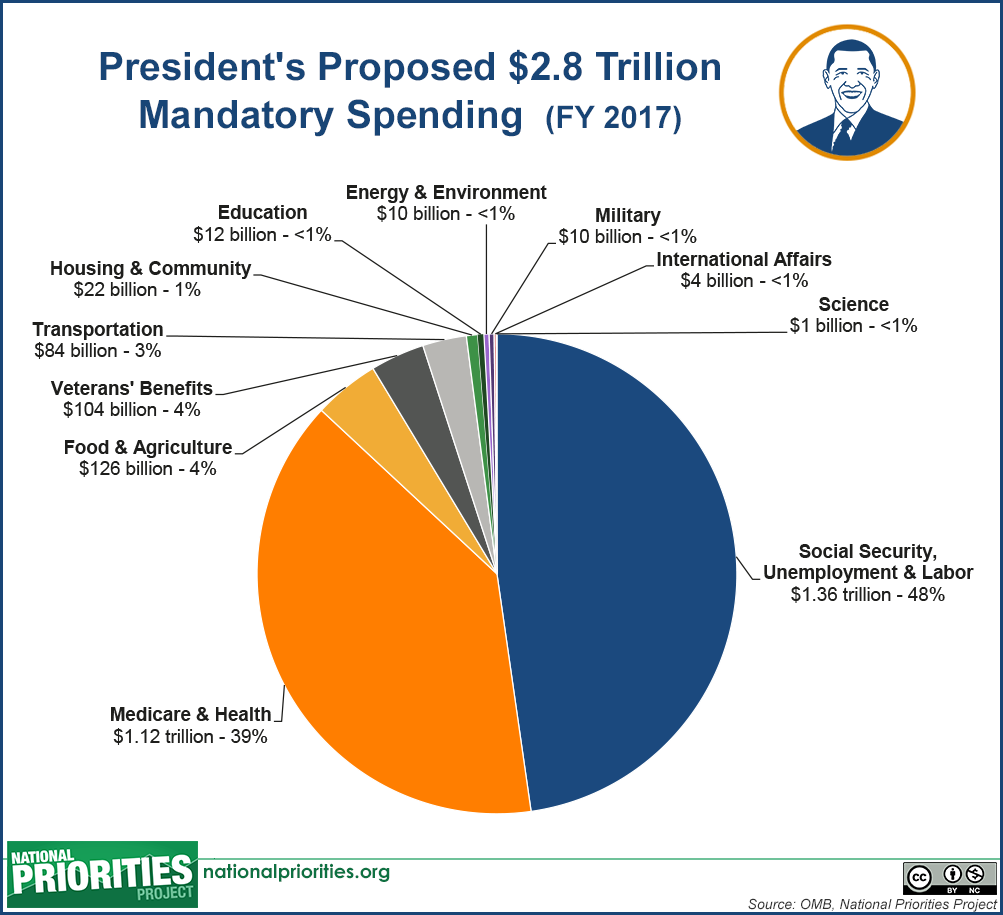
Financing
Medicare has several sources of financing.
Part A's inpatient admitted hospital and skilled nursing coverage is largely funded by revenue from a 2.9% payroll taxlevied on employers and workers (each pay 1.45%). Until December 31, 1993, the law provided a maximum amount of compensation on which the Medicare tax could be imposed annually, in the same way that the Social Security payroll tax operates. Beginning on January 1, …
Eligibility
In general, all persons 65 years of age or older who have been legal residents of the United States for at least five years are eligible for Medicare. People with disabilities under 65 may also be eligible if they receive Social Security Disability Insurance (SSDI) benefits. Specific medical conditions may also help people become eligible to enroll in Medicare.
People qualify for Medicare coverage, and Medicare Part A premiums are entirely waived, if the f…
Benefits and parts
Medicare has four parts: loosely speaking Part A is Hospital Insurance. Part B is Medical Services Insurance. Medicare Part D covers many prescription drugs, though some are covered by Part B. In general, the distinction is based on whether or not the drugs are self-administered but even this distinction is not total. Public Part C Medicare health plans, the most popular of which are bran…
Out-of-pocket costs
No part of Medicare pays for all of a beneficiary's covered medical costs and many costs and services are not covered at all. The program contains premiums, deductibles and coinsurance, which the covered individual must pay out-of-pocket. A study published by the Kaiser Family Foundation in 2008 found the Fee-for-Service Medicare benefit package was less generous than either the typical large employer preferred provider organization plan or the Federal Employees He…