
What is a Medicare/Medicaid provider number?
A Medicare/Medicaid Provider Number (MPN) verifies that a provider has been Medicare certified and establishes the type of care the provider can perform. This identifier is a six-digit number. The first two digits specify the state in which the provider is located, and the last four digits indicate the type of facility. For Ambulatory Surgery Centers, the MPN is 10 digits — with the …
What is a Medicare provider number (MPN)?
A Medicare/Medicaid Provider Number (MPN) verifies that a provider has been Medicare certified and establishes the type of care the provider can perform. This identifier is a six-digit number. The first two digits specify the state in which the provider is located, and the last four digits indicate the type of facility.
What are the billing responsibilities of a Medicare provider?
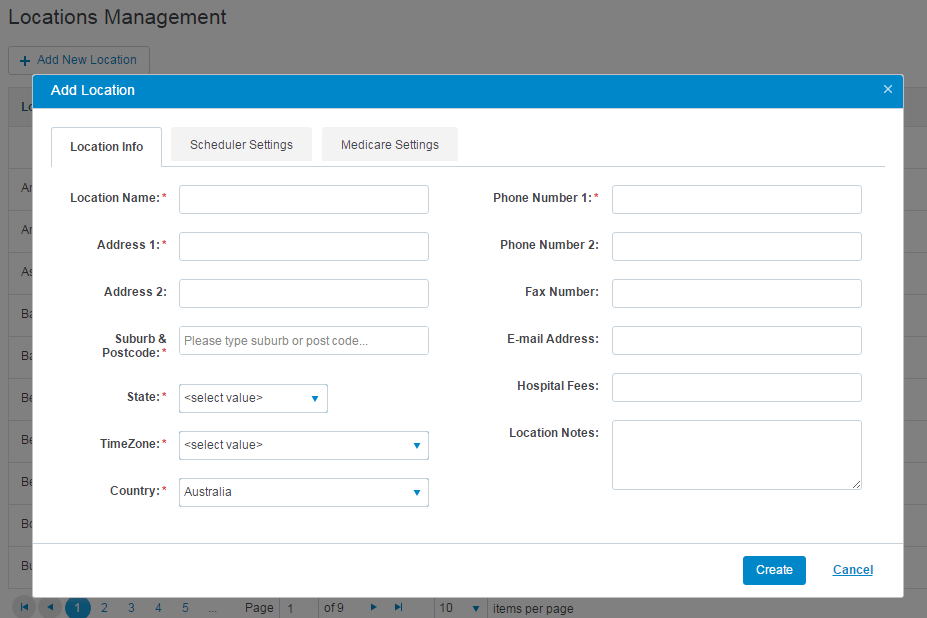
furnished the care must be identified in the billing provider loop. You must also report the name of the facility for whom the claim is being submitted, that facility’s address, and should report applicable NPI (when obtained prior to May 23, 2007), as well as the Medicare OSCAR number assigned to that provider in the 2010A/A (billing provider)
How do I contact Medicare about a medical bill?
Dec 01, 2021 · The NPI is a unique identification number for covered health care providers. Covered health care providers and all health plans and health care clearinghouses must use the NPIs in the administrative and financial transactions adopted under HIPAA. The NPI is a 10-position, intelligence-free numeric identifier (10-digit number).
What is required to bill Medicare?
In summary, a provider, whether participating or nonparticipating in Medicare, is required to bill Medicare for all covered services provided. If the provider has reason to believe that a covered service may be excluded because it may be found not to be reasonable and necessary the patient should be provided an ABN.
Is the Medicare provider number the same as NPI?
What are the NPI and CCN numbers? The NPI is the National Provider Identifier, and is a unique identification number provided to facilities and other medical entities. The Medicare Provider Number is also known as the CCN (CMS Certification Number). This is the six-digit Medicare certification number for a facility.
Does Medicare require a referring provider on claims?
Medicare requires the ordering/referring provider information for the following: Medicare covered services and items that are the result of a physician's order or referral.Dec 28, 2015
How does Medicare define a provider?
Provider is defined at 42 CFR 400.202 and generally means a hospital, critical access hospital, skilled nursing facility, comprehensive outpatient rehabilitation facility (CORF), home health agency or hospice, that has in effect an agreement to participate in Medicare; or a clinic, rehabilitation agency, or public ...
How many digits is a Medicare ID number?
11 charactersThe MBI has 11 characters, like the Health Insurance Claim Number (HICN), which can have up to 11. Will the MBI's characters have any meaning? Each MBI is randomly generated. This makes MBIs different than HICNs, which are based on the Social Security Numbers (SSNs) of people with Medicare.
What is a CNN number?
Call CNN at 1 (404) 827-1500.
Who is the billing provider?
The billing provider is the individual or organization that furnishes and bills Medicare for the ordered/referred service provided to the beneficiary.Feb 1, 2022
Is rendering and referring provider be the same?
The Referring Provider is the individual who directed the patient for care to the provider rendering the services being reported.
Is ordering provider and referring provider is same?
Referring physician - is a physician who requests an item or service for the beneficiary for which payment may be made under the Medicare program. Ordering physician - is a physician or, when appropriate, a non-physician practitioner who orders non-physician services for the patient.Jan 29, 2018
What is a provider type code?
Provider types include individuals, facilities, and vendors. The provider's specialty is a value indicating what field of medicine a provider has additional education in to make him/her a specialist in a certain field. NOTE: Provider type codes may not be unique to one provider type.
What is a Medicare Part B provider?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers. medically necessary.
What is an example of a healthcare provider?
Healthcare providers include hospitals, doctors, nursing staff, clinics, nursing homes, medical practitioners, nutritionists and dieticians, and many more. Hospitals, clinics, and nursing homes are the places where patients come for getting diagnosis for any injury or disease.
What is Medicare provider number?
A Medicare/Medicaid Provider Number (MPN) verifies that a provider has been Medicare certified and establishes the type of care the provider can perform. This identifier is a six-digit number. The first two digits specify the state in which the provider is located, and the last four digits indicate the type of facility.
What is an MPN number?
MPN is also known as an OSCAR (Online Survey, Certification and Reporting) Number, Medicare Identification Number, and Provider Number . Though no longer the primary identification method, the MPN was once the primary identifier for Medicare and Medicaid providers.
What is an MPN?
An MPN is issued by CMS and used by Medicare for surveys, certification, and patient assessments. A facility must pass a Medicare survey/inspection to obtain an MPN. Providers that do not participate in the Medicare program will not have an MPN.
What is a CCN in healthcare?
The MPN (or CCN), however, continues to be issued to providers to confirm Medicare/Medicaid certification for certifications, surveys, and patient assessments.
What is MLN CMS?
The Medicare Learning Network (MLN) is a CMS initiative to ensure Medicare physicians, providers and supplies have immediate access to Medicare coverage and reimbursement rules in a brief, accurate, and easy to understand format. To access MLN Matters articles, click on the MLN Matters link.
What is secondary payer Medicare?
Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare. For example, information submitted on a medical claim or from other sources may result in an MSP claims investigation that involves the collection of data on other health insurance. In such situations, the other health plan may have the legal obligation to meet the beneficiary's health care expenses first before Medicare. For more information about Medicare Secondary Payer and the providers’ role in collecting data to ensure they are billing the correct primary payer, please see the Medicare Secondary Payer Fact Sheet (PDF).
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken Medicare payment. The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
What is the BCRC? What is its role?
The BCRC is the sole authority to ensure the accuracy and integrity of the MSP information contained in CMS's database (i.e., Common Working File (CWF)). Information received because of MSP data gathering and investigation is stored on the CWF. MSP data may be updated, as necessary, based on additional information received from external parties (e.g., beneficiaries, providers, attorneys, third party payers). Beneficiary, spouse and/or family member changes in employment, reporting of an accident, illness, or injury, Federal program coverage changes, or any other insurance coverage information should be reported directly to the BCRC. CMS also relies on providers and suppliers to ask their Medicare patients about the presence of other primary health care coverage, and to report this information when filing claims with the Medicare program.
What is a coba?
The Coordination of Benefits Agreement (COBA) Program establishes a nationally standard contract between CMS and other health insurance organizations that defines the criteria for transmitting enrollee eligibility data and Medicare adjudicated claim data. CMS has provided a COBA Trading Partners customer service contact list as an avenue for providers to contact the trading partners. The COBA Trading Partners document in the Download section below provides a list of automatic crossover trading partners in production, their identification number, and customer contact name and number. For additional information, click the COBA Trading Partners link.
What is a provider NPI?
The National Provider Identifier (NPI) is a Health Insurance Portability and Accountability Act (HIPAA) Administrative Simplification Standard. The NPI is a unique identification number for covered health care providers. Covered health care providers and all health plans and health care clearinghouses must use the NPIs in the administrative and financial transactions adopted under HIPAA. The NPI is a 10-position, intelligence-free numeric identifier (10-digit number). This means that the numbers do not carry other information about healthcare providers, such as the state in which they live or their medical specialty. The NPI must be used in lieu of legacy provider identifiers in the HIPAA standards transactions.
What is NPI in HIPAA?
The NPI must be used in lieu of legacy provider identifiers in the HIPAA standards transactions. As outlined in the Federal Regulation, The Health Insurance Portability and Accountability Act of 1996 (HIPAA), covered providers must also share their NPI with other providers, health plans, clearinghouses, and any entity that may need it ...
What is secondary payer?
Medicare is the Secondary Payer when Beneficiaries are: 1 Treated for a work-related injury or illness. Medicare may pay conditionally for services received for a work-related illness or injury in cases where payment from the state workers’ compensation (WC) insurance is not expected within 120 days. This conditional payment is subject to recovery by Medicare after a WC settlement has been reached. If WC denies a claim or a portion of a claim, the claim can be filed with Medicare for consideration of payment. 2 Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer. 3 Covered under their own employer’s or a spouse’s employer’s group health plan (GHP). 4 Disabled with coverage under a large group health plan (LGHP). 5 Afflicted with permanent kidney failure (End-Stage Renal Disease) and are within the 30-month coordination period. See ESRD link in the Related Links section below for more information. Note: For more information on when Medicare is the Secondary Payer, click the Medicare Secondary Payer link in the Related Links section below.
Is Medicare a primary or secondary payer?
Providers must determine if Medicare is the primary or secondary payer; therefore, the beneficiary must be queried about other possible coverage that may be primary to Medicare. Failure to maintain a system of identifying other payers is viewed as a violation of the provider agreement with Medicare.
What is a medical biller?
In general, the medical biller creates claims like they would for Part A or B of Medicare or for a private, third-party payer. The claim must contain the proper information about the place of service, the NPI, the procedures performed and the diagnoses listed. The claim must also, of course, list the price of the procedures.
What is 3.06 Medicare?
3.06: Medicare, Medicaid and Billing. Like billing to a private third-party payer, billers must send claims to Medicare and Medicaid. These claims are very similar to the claims you’d send to a private third-party payer, with a few notable exceptions.
How long does it take for Medicare to process a claim?
The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days .
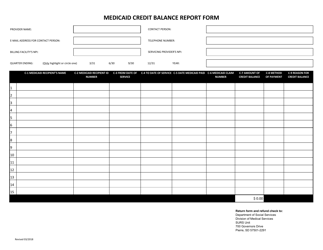
Is it harder to make a claim for medicaid or Medicare?
Creating claims for Medicaid can be even more difficult than creating claims for Medicare. Because Medicaid varies state-by-state, so do its regulations and billing requirements. As such, the claim forms and formats the biller must use will change by state. It’s up to the biller to check with their state’s Medicaid program to learn what forms ...
Coordination of Benefits Overview
Information Gathering
Provider Requests and Questions Regarding Claims Payment
Medicare Secondary Payer Records in CMS's Database
Termination and Deletion of MSP Records in CMS's Database
Contacting The BCRC
Contacting The Medicare Claims Office
- Contact your local Medicare Claims Office to: 1. Answer your questions regarding Medicare claim or service denials and adjustments. 2. Answer your questions concerning how to bill for payment. 3. Process claims for primary or secondary payment. 4. Accept the return of inappropriate Medicare payment.
Coba Trading Partner Contact Information
mln Matters Articles - Provider Education