Covered Services Under Medicare Part B
| Ambulance services | If you need transportation for a medical ... |
| Cardiac rehabilitation | Medicare Part B covers approved exercise ... |
| Chiropractic services (limited) | These services can help correct a sublux ... |
| Diabetes self-management training | This class shows you how to manage your ... |
| Diabetes supplies | Covered supplies can include: Blood suga ... |
Full Answer
What is the maximum premium for Medicare Part B?
Sep 11, 2014 · The basic medically-necessary services covered include: Abdominal Aortic Aneurysm Screening Ambulance Services Blood Bone Mass Measurement (Bone Density) Cardiac Rehabilitation Cardiovascular Screenings Chiropractic Services (limited) Clinical Laboratory Services Clinical Research Studies Colorectal ...
What are the rules for Medicare Part B?
25 rows · Medicare Part B covers approved exercise, education, and counseling programs for patients ...
What is the difference between Medicare Part an and Part B?
Learn about what Medicare Part B (Medical Insurance) covers, including doctor and other health care providers' services and outpatient care. Part B also covers durable medical equipment, home health care, and some preventive services. What Medicare health plans cover. Medicare health plans include Medicare Advantage, Medical Savings Account (MSA), Medicare Cost …
What services are covered under Medicare Part?
Services Covered by Medicare Part A & Part B. Eyeglasses (Limited) Medicare covers one pair of eyeglasses with standard frames (or one set of contact lenses) after cataract surgery that implants ... Diabetes Supplies. Diabetes screenings. Diabetes Self-Management Training. Blood. If the provider ...
What services are covered by Medicare Part B?
Part B covers things like:Clinical research.Ambulance services.Durable medical equipment (DME)Mental health. Inpatient. Outpatient. Partial hospitalization.Limited outpatient prescription drugs.
Which service would not be covered under Medicare Part B?
Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing. Long-term supports and services can be provided at home, in the community, in assisted living, or in nursing homes.
What does Medicare Part B entitle you to?
Medicare Part B (Medical Insurance) Part B helps cover medically necessary services like doctors' services, outpatient care, and other medical services that Part A doesn't cover. Part B also covers many preventive services.
What does Medicare Part B reimburse for?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. premium deducted automatically from their Social Security benefit payment (or Railroad Retirement Board benefit payment).
What services does Medicare not cover?
Medicare does not cover: medical exams required when applying for a job, life insurance, superannuation, memberships, or government bodies. most dental examinations and treatment. most physiotherapy, occupational therapy, speech therapy, eye therapy, chiropractic services, podiatry, acupuncture and psychology services.Jun 24, 2021
Does Medicare Part B include dental coverage?
Yes, but Medicare Part B only covers dental expenses that are a medically necessary part of another covered service. It does not cover routine dental services, such as cleanings, or other standard procedures like dentures, crowns, or fillings.
What part of Medicare covers prescriptions?
Part DMedicare offers prescription drug coverage for everyone with Medicare. This coverage is called “Part D.” There are 2 ways to get Medicare prescription drug coverage: 1. Join a Medicare Prescription Drug Plan (PDP).
What is the Medicare Part B deductible for 2021?
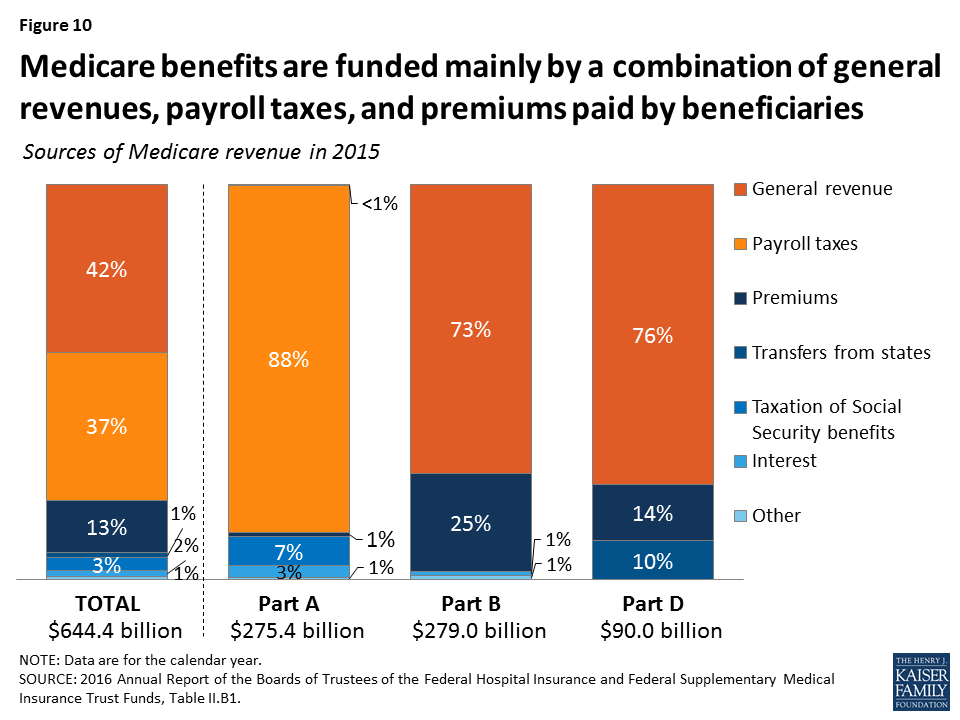
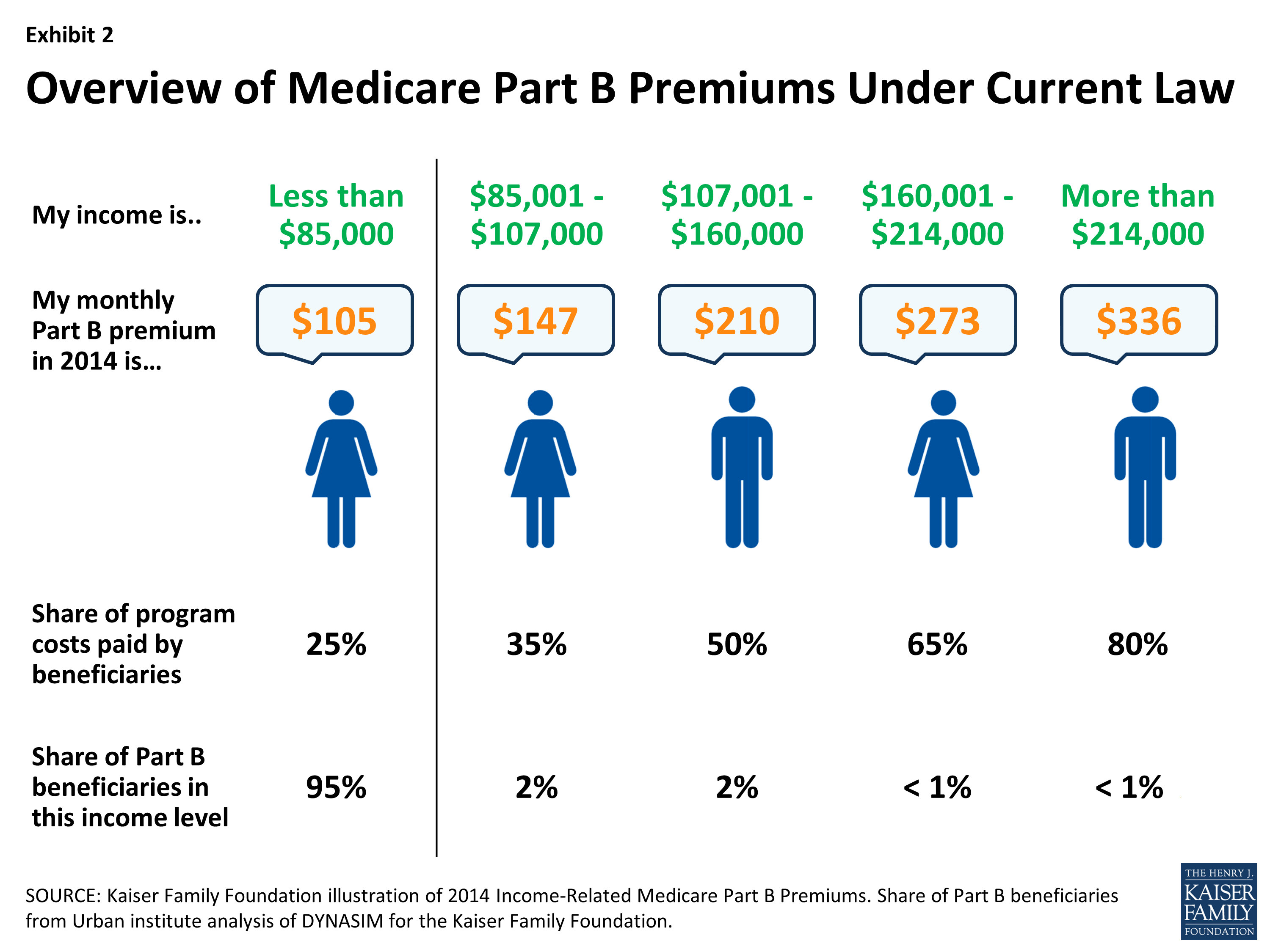
$203 inMedicare Part B Premiums/Deductibles The standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.Nov 6, 2020
Does Medicare affect Social Security?
Does Social Security pay for Medicare? Social Security does not pay for Medicare, but if you receive Social Security payments, your Part B premiums can be deducted from your check. This means that instead of $1,500, for example, you'll receive $1,386.40 and your Part B premium will be paid.May 13, 2020
Which service is covered by Medicare Part B quizlet?
Part B helps cover medically-necessary services like doctors' services, outpatient care, durable medical equipment, home health services, and other medical services.
How do you qualify to get $144 back from Medicare?
How do I qualify for the giveback?Be a Medicare beneficiary enrolled in Part A and Part B,Be responsible for paying the Part B premium, and.Live in a service area of a plan that has chosen to participate in this program.Nov 24, 2020
What month is Medicare deducted from Social Security?
Hi RCK. The Medicare premium that will be withheld from your Social Security check that's paid in August (for July) covers your Part B premium for August. So, if you already have Part B coverage you'll need to pay your Medicare premiums out of pocket through July.Mar 5, 2021
What does Medicare Part B cover?
Medicare Part B covers ground ambulance transportation when you need to be taken to a hospital or skilled nursing facility for medically necessary services , and when transportation in any other vehicle could endanger your health.
How many visits does Medicare cover?
Medicare Part B benefits cover up to eight face-to-face visits with a Medicare-recognized practitioner in a 12-month period. Speech therapy. Also known as speech-language pathology services, these benefits involve evaluation and treatment to regain and strengthen speech and language skills.
How often is a wellness visit covered by Medicare?
Wellness Visit: This is covered once a year, after your first year of Medicare Part B coverage. At this visit, the doctor works with you to develop or update a personalized prevention plan based on your current health and risk factors. You pay nothing for the Wellness exam if the doctor accepts Medicare assignment.
What is a DME in medical terms?
Durable medical equipment (such as walkers) Durable medical equipment (DME) refers to items such as oxygen equipment and supplies, wheelchairs, walkers, and hospital beds ordered by a Medicare doctor for use in the home. You might need to rent some items.
Does Medicare cover exercise?
Medicare will only cover services to the nearest appropriate medical facility that is able to give you the care you need. Medicare Part B covers approved exercise, education, and counseling programs for patients who meet certain conditions.
Does Medicare cover chiropractic care?
Medicare Part B also covers intensive cardiac rehabilitation programs that are more rigorous than regular cardiac rehabilitation programs. Chiropractic services (limited) These services can help correct a subluxation (when one or more of the bones of your spine move out of position) using manipulation of the spine.
Does Medicare cover eyeglasses after cataract surgery?
Medicare Part B does cover one pair of eyeglasses with standard frames (or one set of contact lenses) after cataract surgery. Hearing and balance exams. These exams are covered if your doctor orders hearing and balance tests to see if you need medical treatment.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is Medicare Part B?
Medicare Part B covers medically necessary services and preventative services. The partial-list of Medicare covered services below will help you learn about some of the services covered by Medicare and basic information about each. You can find out if your test, item, or service is covered by visiting Medicare.gov here.
How much does Medicare pay for ambulatory surgery?
Except for certain preventive services (for which you pay nothing if the doctor or other health care provider accepts assignment), you pay 20% of the Medicare-approved amount to both the ambulatory surgical center and the doctor who treats you, and the Part B deductible applies.
What are the benefits of Medicare?
Medicare covers comprehensive programs that include exercise, education, and counseling for patients who meet at least one of these conditions: 1 A heart attack in the last 12 months 2 Coronary artery bypass surgery 3 Current stable angina pectoris (chest pain) 4 A heart valve repair or replacement 5 A coronary angioplasty (a medical procedure used to open a blocked artery) or coronary stenting (a procedure used to keep an artery open) 6 A heart or heart-lung transplant Medicare also covers intensive cardiac rehabilitation programs that are typically more rigorous or more intense than regular cardiac rehabilitation programs. Services are covered in a doctor’s office or hospital outpatient setting. You pay 20% of the Medicare-approved amount if you get the services in a doctor’s office. In a hospital outpatient setting, you also pay the hospital a copayment. The Part B deductible applies.
What is clinical research?
Clinical research studies test how well different types of medical care work and if they’re safe. Medicare covers some costs, like office visits and tests, in qualifying clinical research studies.
How many depression screenings does Medicare cover?
Medicare covers one depression screening per year . The screening must be done in a primary care setting (like a doctor’s office) that can provide follow-up treatment and referrals. You pay nothing for this screening if the doctor or other qualified health care provider accepts assignment.
Does Medicare cover diabetes screenings?
Diabetes screenings. Medicare covers these screenings if your doctor determines you’re at risk for diabetes . You may be eligible for up to 2 diabetes screenings each year. You pay nothing for the test if your doctor or other qualified health care provider accepts assignment.
How many visits does Medicare cover?
Medicare will cover one visit per year with a primary care doctor in a primary care setting (like a doctor’s office) to help lower your risk for cardiovascular disease. During this visit, the doctor may discuss aspirin use (if appropriate), check your blood pressure, and give you tips to make sure you eat well.
What is Medicare intern?
For Medicare purposes, the terms “interns” and “residents” include physicians participating in approved postgraduate training programs and physicians who are not in approved programs but who are authorized to practice only in a hospital setting, e.g., individuals with temporary or restricted licenses, or unlicensed graduates of foreign medical schools. Where a senior resident has a staff or faculty appointment or is designated, for example, a “fellow,” it does not change the resident’s status for the purposes of Medicare coverage and reimbursement. As a general rule, services of interns and residents are paid as provider services by the A/B MAC (A).
What is the purpose of psychiatric services?
Services must be for the purpose of diagnostic study or reasonably be expected to improve the patient's condition. The treatment must, at a minimum, be designed to reduce or control the patient's psychiatric symptoms so as to prevent relapse or hospitalization, and improve or maintain the patient's level of functioning.
What is the purpose of observation?
The purpose of observation is to determine the need for further treatment or for inpatient admission. Thus, a patient receiving observation services may improve and be released, or be admitted as an inpatient (see Pub. 100-02, Medicare Benefit Policy Manual, Chapter 1, Section 10 “Covered Inpatient Hospital Services Covered Under Part A” at https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c01.pdf). For more information on correct reporting of observation services, see Pub. 100-04, Medicare Claims Processing Manual, chapter 4, section 290.2.2.)
What is observation care?
Observation care is a well-defined set of specific, clinically appropriate services, which include ongoing short term treatment, assessment, and reassessment before a decision can be made regarding whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital. Observation services are commonly ordered for patients who present to the emergency department and who then require a significant period of treatment or monitoring in order to make a decision concerning their admission or discharge.
What is a partial program admission?
A particular individual covered service (described above) as intervention, expected to maintain or improve the individual’s condition and prevent relapse, may also be included within the plan of care, but the overall intent of the partial program admission is to treat the serious presenting psychiatric symptoms. Continued treatment in order to maintain a stable psychiatric condition or functional level requires evidence that less intensive treatment options (e.g., intensive outpatient, psychosocial, day treatment, and/or other community supports) cannot provide the level of support necessary to maintain the patient and to prevent hospitalization.
Is a denial of a benefit category appealable?
Benefit category denials made under §1861(ff) or §1835(a)(2)(F) are not appealable by the provider and the limitation on liability provision does not apply (HCFA Ruling 97-1). Examples of benefit category based in §1861(ff) or §1835(a)(2)(F) of the Act, for partial hospitalization services generally include the following:
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
What is intermittent skilled nursing?
Intermittent skilled nursing care (other than drawing blood) Physical therapy, speech-language pathology, or continued occupational therapy services. These services are covered only when the services are specific, safe and an effective treatment for your condition.
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
Do you have to be homebound to get home health insurance?
You must be homebound, and a doctor must certify that you're homebound. You're not eligible for the home health benefit if you need more than part-time or "intermittent" skilled nursing care. You may leave home for medical treatment or short, infrequent absences for non-medical reasons, like attending religious services.
What is Medicare HIT?
144-255), established a new Medicare HIT benefit under Medicare Part B. The Medicare HIT benefit is for coverage of HIT services for certain drugs and biologicals administered intravenously, or subcutaneously for an administration period of 15 minutes or more, in the home of an individual, through a pump that is a DME item. This benefit is effective January 1, 2021.
What is a HIT benefit?
The HIT benefit is intended to be a separate payment from the amount paid under the DME benefit, explicitly covering the professional services that occur in the patient’s home (and that are not for the set-up and training on the routine use of the external infusion pump), as well as monitoring and remote monitoring services for the provision of home infusion drugs. Home infusion drugs are defined as parenteral drugs and biologicals administered intravenously, or subcutaneously for an administration period of 15 minutes or more, in the home of an individual through a pump that is an item of DME covered under the Medicare Part B DME benefit. The HIT benefit covers services distinct from those under the DME benefit (as discussed above) and could conceivably include, for example:
What services does Medicare cover?
Dentures. Cosmetic surgery. Acupuncture. Hearing aids and exams for fitting them. Routine foot care. Find out if Medicare covers a test, item, or service you need. If you need services Medicare doesn't cover, you'll have to pay for them yourself unless you have other insurance or a Medicare health plan that covers them.
What does Medicare not cover?
Medicare doesn't cover everything. Some of the items and services Medicare doesn't cover include: 1 Long-Term Care#N#Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing. Long-term supports and services can be provided at home, in the community, in assisted living, or in nursing homes. Individuals may need long-term supports and services at any age. Medicare and most health insurance plans don’t pay for long-term care.#N#(also called#N#custodial care#N#Non-skilled personal care, like help with activities of daily living like bathing, dressing, eating, getting in or out of a bed or chair, moving around, and using the bathroom. It may also include the kind of health-related care that most people do themselves, like using eye drops. In most cases, Medicare doesn't pay for custodial care.#N#) 2 Most dental care 3 Eye exams related to prescribing glasses 4 Dentures 5 Cosmetic surgery 6 Acupuncture 7 Hearing aids and exams for fitting them 8 Routine foot care
Does Medicare pay for long term care?
Medicare and most health insurance plans don’t pay for long-term care. (also called. custodial care. Non-skilled personal care, like help with activities of daily living like bathing, dressing, eating, getting in or out of a bed or chair, moving around, and using the bathroom.
Does Medicare cover everything?
Medicare doesn't cover everything. Some of the items and services Medicare doesn't cover include: Long-Term Care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
Can you transfer financial liability to a patient?
To transfer potential financial liability to the patient, you must give written notice to a Fee-for-Service Medicare patient before furnishing items or services Medicare usually covers but you don’ t expect them to pay in a specific instance for certain reasons, such as no medical necessity .
Does Medicare cover non-physician services?
Medicare normally excludes coverage for non-physician services to Part A or Part B hospital inpatients unless those services are provided either directly by the hospital/SNF or under an arrangement that the hospital/SNF makes with an outside source.
Does Medicare cover personal comfort items?
Medicare doesn’t cover personal comfort items because these items don’t meaningfully contribute to treating a patient’s illness or injury or the functioning of a malformed body member. Some examples of personal comfort items include:
Does Medicare cover dental care?
Medicare doesn’t cover items and services for the care, treatment, filling, removal, or replacement of teeth or the structures directly supporting the teeth, such as preparing the mouth for dentures, or removing diseased teeth in an infected jaw. The structures directly supporting the teeth are the periodontium, including:
Does Medicare cover exceptions?
This booklet outlines the 4 categories of items and services Medicare doesn’t cover and exceptions (items and services Medicare may cover). This material isn’t an all-inclusive list of items and services Medicare may or may not cover.