• If a Medicare beneficiary also has Medicaid then Medicare always pays first. Medicaid is second payer, or the payer of last resort if there’s another insurance (i.e. an employer or retiree health plan). • Once on Medicare, claims are processed FIRST by Medicare A or B or their MA plan (Part C).
Who is eligible for Medicare?
Importantly, Medicare coverage always takes precedence over Medicaid. Consider that you see a specialist and need a prescription drug. The bill is first paid with Medicare Parts B and D. When all Medicare payments have been made, Medicaid will pick up the remainder of eligible costs. Do Medicare and Medicaid Cover Long-Term Care?
Who pays first Medicare or Medicaid?
Nov 16, 2017 · Medicare is the earned-benefit program for Americans aged 65 or older or disabled. Workers pay into Medicare throughout their working years. The Centers for Medicare & Medicaid Services is the agency in charge of both Medicare and Medicaid, but you sign up for Medicare A (Hospital) and Medicare B (Medical) through Social Security.
How can I see if I qualify for Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for …
How do I get Medicaid if I have too much income?
Dec 01, 2019 · The main points to know are these. A state-imposed, post-death lien on a house occupied by the loved ones of a deceased recipient of Medicaid will get money back to the government, but not while a spouse or dependent/disabled child is still living—anywhere. And the spouse may sell the home, overriding the Medicaid lien.
How do you determine which insurance is primary and which is secondary?
How do you determine which insurance is primary?
Is Medicare always primary or secondary?
Is Medicare always the primary payer?
Is it better to have two health insurances?
Can you have two health insurances at the same time?
Does Medicare automatically forward claims to secondary insurance?
Does Medicare pay first or second?
Will Medicaid pay for my Medicare Part B premium?
Do retirees pay Medicare premiums?
You'll need to pay monthly premiums, copayments, coinsurance, and deductibles. You can pay for premiums and other Medicare costs in several ways. While you could budget and save for healthcare throughout your life, other programs can help: Paying with Social Security.
Can you have Medicare and Humana at the same time?
Why do doctors not like Medicare Advantage plans?
What Is Medicaid?
Instead of age, eligibility for Medicaid is based on income. It is a health care program designed to provide coverage for low-income Americans.
What Does Medicaid Cover?
Medicaid covers most medical services that an individual or family would need. It covers hospitalizations, X-rays, and other laboratory services.
What Is Medicare?
Let’s start off by defining Medicare and explaining the different parts of the program. Medicare is a federal entitlement program that you pay into while working.
Can You Have Access to Both Programs?
It is possible for low-income seniors to be eligible for both programs. This scenario is referred to as dual eligibility.
Do Medicare and Medicaid Cover Long-Term Care?
Many disabled and elderly Americans deplete their savings to pay for long-term care. Unfortunately, Medicare and many private health insurance plans do not cover long-term care.
The Difference between Medicare and Medicaid – A Recap
Both programs are invaluable for providing health care to Americans in need. The primary difference between the two programs is that Medicare largely depends on age. On the other hand, Medicaid eligibility is based on income.
What is Medicare and Medicaid?
Medicare and Medicaid are two of the major insurance programs that provide healthcare to the American public. Understanding each program, as well as how the two programs differ, can help you and those you care about find the right healthcare program. Tags: Disability, Medicaid, Medicare. See Comments.
What is Medicare A?
Medicare is the earned-benefit program for Americans aged 65 or older or disabled. Workers pay into Medicare throughout their working years. The Centers for Medicare & Medicaid Services is the agency in charge of both Medicare and Medicaid, but you sign up for Medicare A (Hospital) and Medicare B (Medical) through Social Security.
Does medicaid require taxes?
Medicaid offers care for the most vulnerable among us. While it does not require paying taxes while working, it does have guidelines about how much income and resources you can have to qualify. Medicaid provides coverage for older people, people with disabilities, and some families with children.
What is Medicaid coverage?
Medicaid provides coverage for older people, people with disabilities, and some families with children. Each state has its own eligibility rules and decides which services to cover. The names of the Medicaid program may vary from state to state.
What does the letter M mean in Medicare?
Both programs begin with the letter “M.”. They’re both health insurance programs run by the government. People often ask questions about what Medicare and Medicaid are, what services they cover, and who administers the programs. Let’s start with Medicare. Medicare is the earned-benefit program for Americans aged 65 or older or disabled.
Is Medicare part of Medicaid?
Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance).
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
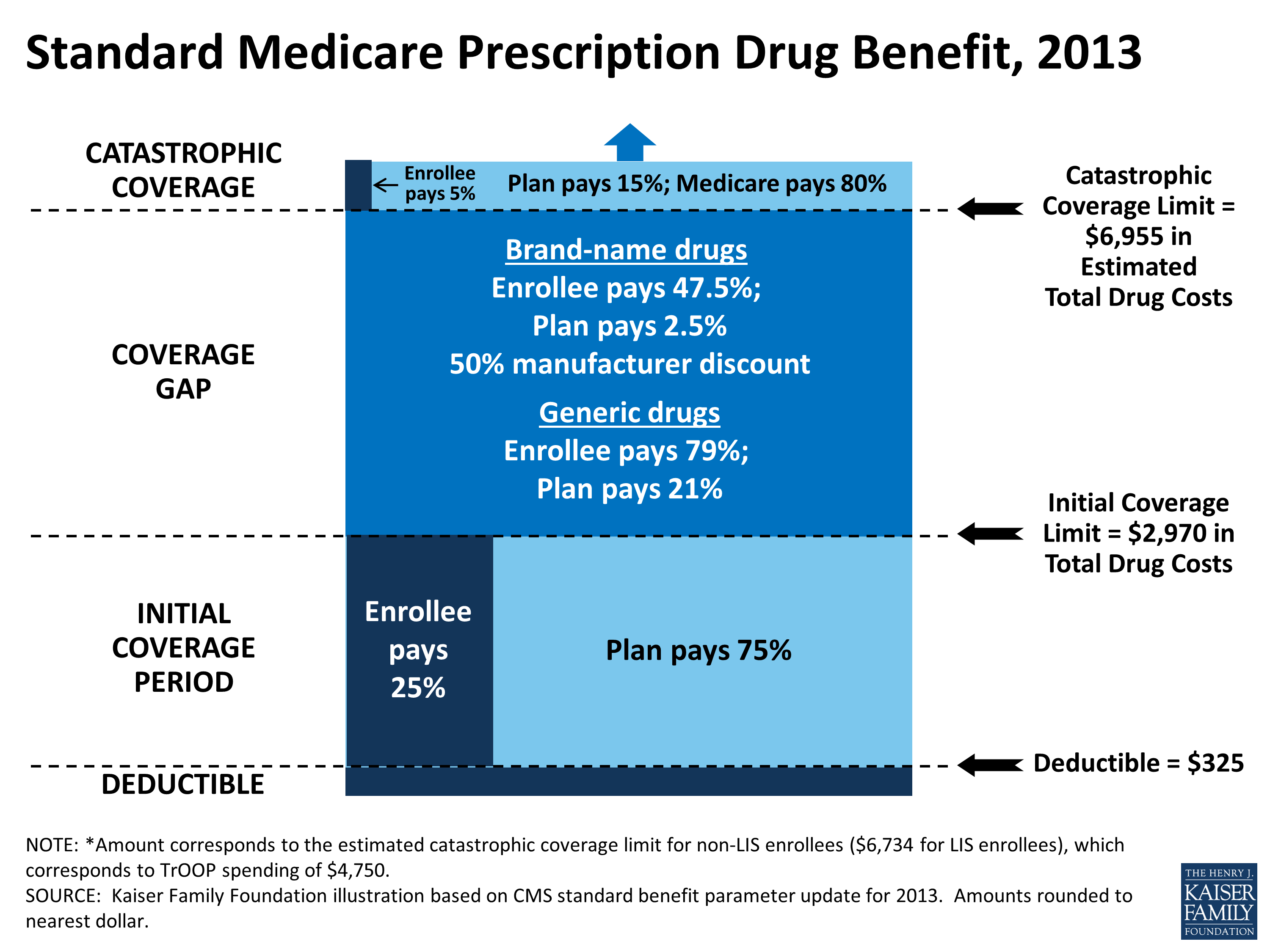
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
Can you take Medicaid home?
If you are likely to return home after a period of care, or your spouse or dependents live in the home, the state generally cannot take your home in order to recover payments.
Does Medicaid get first dibs?
And Medicaid gets first dibs —even over a mortgage lender. Should the homeowner die with the lien in place, Medicaid recovery becomes a part of probate. In many cases, an adult child of the deceased is forced to pay the Medicaid claim when taking title to a parent’s property.
Can you recover Medicaid if your spouse has an equity interest in your home?
Your home is also shielded from recovery if a spouse or sibling has an equity interest in it, and has lived in it for the legally specified time, or if it’s the home of a child who is under 21 or lives with a disability. But Medicaid may try to recover funds at a future date, before your home is conveyed to a new owner.
Does Medicare cover long term care?
Medicare, as a rule, does not cover long-term care settings. So, Medicare in general presents no challenge to your clear home title. Most people in care settings pay for care themselves. After a while, some deplete their liquid assets and qualify for Medicaid assistance. Check your state website to learn about qualifications for Medicaid.
Can Medicare challenge a clear title?
So, Medicare in general presents no challenge to your clear home title. Most people in care settings pay for care themselves. After a while, some deplete their liquid assets and qualify for Medicaid assistance. Check your state website to learn about qualifications for Medicaid. If you are likely to return home after a period of care, ...
When did Medicaid lien on homes become common?
The Federal Government Has Pressed People to Rely on Private Funds. Medicaid liens on homes have become common since the federal Omnibus Budget Reconciliation Act (OBRA) of 1993, which forces estate recovery if the homeowner: Relied on Medicaid at age 55+. Left the home, at any age, for a permanent care setting.
What are the two types of liens for Medicaid?
Medicaid uses two lien types: TEFRA, and estate recovery liens. Under the Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982, states may prevent Medicaid recipients from giving away the home that they leave when they go into a long-term care setting.
Can you recover Medicaid money after a deceased person dies?
States may not recover from the estate of a deceased Medicaid enrollee who is survived by a spouse, child under age 21, or blind or disabled child of any age.
Can you recover Medicaid from a deceased spouse?
States may not recover from the estate of a deceased Medicaid enrollee who is survived by a spouse, child under age 21, or blind or disabled child of any age. States are also required to establish procedures for waiving estate recovery when recovery would cause an undue hardship.
Can Medicaid liens be placed on a home?
States may also impose liens on real property during the lifetime of a Medicaid enrollee who is permanently institutionalized, except when one of the following individuals resides in the home: the spouse, child under age 21, blind or disabled child of any age, or sibling who has an equity interest in the home.
Can states impose liens on Medicaid?
States are also required to establish procedures for waiving estate recovery when recovery would cause an undue hardship. States may impose liens for Medicaid benefits incorrectly paid pursuant to a court judgment.
Is Medicare primary or secondary?
Option 1: Original Medicare. Medicare is primary and Medi-Cal is secondary. In Original Medicare, also known as fee-for-service, it is important to present providers with both Medicare and Medi-Cal cards. With Original Medicare you can choose any medical provider that accepts Medicare and Medi-Cal, no referrals to a specialist is needed.
What is a medicaid program?
What is Medi-Cal? Medicaid, called Medi-Cal in California, is a joint federal and state program that helps pay medical costs for people with limited income and/or resources (assets). Some people qualify for both Medicare and Medi-Cal.
What is the difference between Medicare and Medi-Cal?
When you have Medicare Parts A and B, Medicare is your primary insurance and pays for most of your medical care. Medi-Cal is your secondary insurance. It pays for costs not covered by Medicare and provides additional benefits not covered by Medicare.
What is Medicare for people over 65?
Medicare is health insurance for: People 65 or older. People under 65 with certain disabilities. People of any age with End-Stage Renal Disease (ESRD) – permanent kidney failure requiring dialysis or a kidney transplant. People of any age with Amyotrophic Lateral Sclerosis (ALS), also known as Lou Gehrig’s disease.
Does Medicare cover medical expenses?
If you have Medicare and full Medi-Cal coverage, most of your health care costs are covered. People with Medi-Cal may get coverage for services that Medicare may not or may partially cover, like basic vision and hearing, dental, non-emergency transportation, incontinence supplies, personal care, and home-and community-based services.
Is Medicare a secondary insurance?
Medicare is primary and Medi-Cal is secondary. In Original Medicare, also known as fee-for-service, it is important to present providers with both Medicare and Medi-Cal cards. With Original Medicare you can choose any medical provider that accepts Medicare and Medi-Cal, no referrals to a specialist is needed.
Can you use Medicare and Medi-Cal?
With Original Medicare you can choose any medical provider that accepts Medicare and Medi-Cal, no referrals to a specialist is needed. In addition to the Medicare and Medi-Cal card, beneficiaries also have ...
