What is not typically covered by Medicare?
What diagnosis codes are not covered by Medicare?
- Biomarkers in Cardiovascular Risk Assessment.
- Blood Transfusions (NCD 110.7)
- Blood Product Molecular Antigen Typing.
- BRCA1 and BRCA2 Genetic Testing.
- Clinical Diagnostic Laboratory Services.
- Computed Tomography (NCD 220.1)
- Genetic Testing for Lynch Syndrome.
Does Medicare cover routine bloodwork?
Does Medicare Part B cover lab tests?
What is considered not medically necessary?
What modifiers are not accepted by Medicare?
Is vitamin D blood test covered by Medicare?
What lab can I use with Medicare?
How often will Medicare cover a lipid panel?
Does Medicare cover EMG test?
Is Quest Diagnostics covered by Medicare?
Is Holter monitor covered by Medicare?
What Medicare Doesn’T Cover
Original Medicare, Part A and Part B, doesn’t generally cover the following services and supplies. This may not be a complete list.Alternative medi...
Can I Get Benefits That Pay For Services Medicare Does Not Cover?
Medicare Advantage plans may be an option to consider since they are required to have at least the same level of coverage as Original Medicare, but...
What Medicare Part D Doesn’T Cover
Medicare Part D is optional prescription drug coverage. You can enroll in this coverage through a stand-alone Medicare Part D Prescription Drug Pla...
What services does Medicare cover?
Dentures. Cosmetic surgery. Acupuncture. Hearing aids and exams for fitting them. Routine foot care. Find out if Medicare covers a test, item, or service you need. If you need services Medicare doesn't cover, you'll have to pay for them yourself unless you have other insurance or a Medicare health plan that covers them.
Does Medicare cover everything?
Medicare doesn't cover everything. Some of the items and services Medicare doesn't cover include: Long-Term Care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
Does Medicare pay for long term care?
Medicare and most health insurance plans don’t pay for long-term care. (also called. custodial care. Non-skilled personal care, like help with activities of daily living like bathing, dressing, eating, getting in or out of a bed or chair, moving around, and using the bathroom.
What happens if you take a medication that is not covered by Medicare?
If you are taking a medication that is not covered by Medicare Part D, you may try asking your plan for an exception. As a beneficiary, you have a guaranteed right to appeal a Medicare coverage or payment decision.
What are the requirements for Medicare Part D?
Generally, Medicare Part D will cover certain prescription drugs that meet all of the following conditions: 1 Only available by prescription 2 Approved by the Food and Drug Administration (FDA) 3 Sold and used in the United States 4 Used for a medically accepted purpose 5 Not already covered under Medicare Part A or Part B
What is Medicare Part D?
Medicare Part D is optional prescription drug coverage. You can enroll in this coverage through a stand-alone Medicare Part D Prescription Drug Plan, or through a Medicare Advantage Prescription Drug plan.
What is Medicare services?
Medicare considers services needed for the diagnosis, care, and treatment of a patient’s condition to be medically necessary. These supplies and services cannot be primarily for the convenience of the provider or beneficiary. Always ask your doctor to clarify if you’re not sure whether a specific service or item is covered by Medicare.
Does Medicare cover homemaker services?
You must be taking the most direct route and traveling “without unreasonable delay.”. Homemaker services : Medicare won’t cover homemaker services, such as cooking and cleaning. An exception is if the beneficiary is in hospice care, and the homemaker services are included in the care plan. Long-term care : Medicare doesn’t cover long-term ...
Does Medicare cover hearing aids?
Hearing care : Medicare won’t cover routine hearing exams, hearing aids, and exams to get fitted for hearing aids. However, you may be covered if your doctor orders a diagnostic hearing exam to see if you need further treatment.
Does Medicare cover short term nursing?
However, Medicare does cover short-term skilled nursing care when it follows a qualifying inpatient hospital stay. Medicare Part A may cover nursing care in a skilled nursing facility (SNF) for a limited time if it’s medically necessary for you to receive skilled care.
Medicare Advantage Plans May Cover COVID-19 Tests
Medicare will pay for COVID-19 PCR or rapid tests when they are ordered by a healthcare professional and performed by a laboratory. Currently, a Medicare beneficiary can get one free test performed by a laboratory per year without an order. 2
How to Get Free At-Home Test Kits
If you’re showing symptoms of COVID-19 or you’ve come in contact with someone who has COVID-19, you should get tested three to five days after the exposure.
What This Means For You
Medicare beneficiaries, unlike people with private insurance or Medicaid, cannot be reimbursed for at-home COVID-19 tests because the program is barred from covering self-administered diagnostic tests.
How often does Medicare cover mammograms?
once a year if you meet criteria. *Medicare covers diagnostic mammograms more often if your doctor orders them. You are responsible for the 20 percent coinsurance cost. Other nonlaboratory diagnostic screenings Medicare covers include X-rays, PET scans, MRI, EKG, and CT scans.
What is Medicare Part A?
Medicare Part A offers coverage for medically necessary blood tests. Tests can be ordered by a physician for inpatient hospital, skilled nursing, hospice, home health, and other related covered services. Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines.
What is the purpose of blood test?
Blood tests are an important diagnostic tool doctors use to screen for risk factors and monitor health conditions. A blood test is generally a simple procedure to measure how your body is functioning and find any early warning signs. Medicare covers many types of blood tests. Trusted Source.
How much is Medicare Part B 2021?
You have to meet your annual deductible for this coverage as well. In 2021, the deductible is $203 for most people. Remember, you also have to pay your monthly Part B premium, which is $148.50 in 2021 for most beneficiaries.
How much does a blood test cost?
The costs are based on the particular test, your location, and the lab used. Tests can run from a few dollars to thousands of dollars. That’s why it’s important to check that your test is covered before you have it done.
What to do if your service is not covered?
If a service is not covered, check around to find the lowest-cost provider.
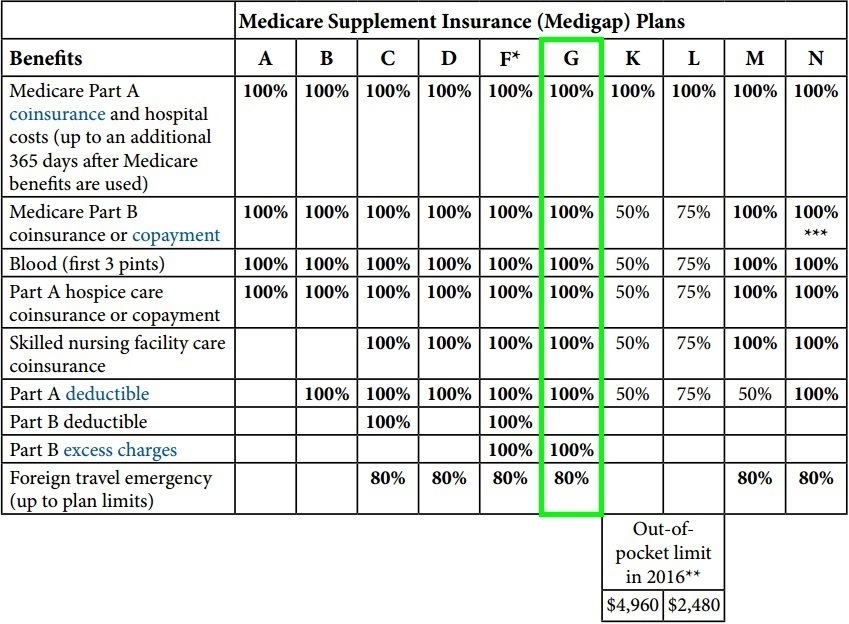
Does Medigap cover out of pocket costs?
Medigap (Medicare supplemental insurance) plans can help pay for some out-of-pocket costs like coinsurance, deductibles, or copayments of covered screenings and other diagnostic tests.
How many Medicare beneficiaries received wellness visits in 2014?
In fact, research published in JAMA found that only about 16% of Medicare beneficiaries received a wellness visit in 2014. While this figure increased significantly since 2011, it's still quite low. One contributing factor has likely been beneficiary confusion about the differences between a Medicare annual wellness exam vs. an annual physical exam.
When did Medicare start offering wellness visits?
The differences between traditional physicals and how Medicare approaches annual exams have created headaches for providers and beneficiaries since the Medicare annual wellness visit debuted in 2011.
How long does a physical exam last?
In defining the term, Dignity Health states, "A thorough physical examination covers head to toe and usually lasts about 30 minutes. It measures important vital signs — temperature, blood pressure, and heart rate — and evaluates your body using ...
Does Medicare cover annual physicals?
While Medicare does not cover annual physical exams, it does cover a single "initial preventive physical examination," followed by exams called "annual wellness visits.
Does Medicare cover Beverly Dunn?
A Kaiser Health News ( KHN) article tells the story of Medicare beneficiary Beverly Dunn. She scheduled her annual physical exam, believing that Medicare would cover the checkup. Then Dunn received the bill and quickly learned the shocking piece of information many patients discover: Medicare does not cover ...
Can Medicare beneficiaries get a physical?
Medicare beneficiaries can still receive an annual physical from their primary care providers, but charges, as discussed earlier, will typically apply to this service. For those patients with a Medicare Advantage plan, an annual physical may be an included benefit.
Is a routine physical exam covered by Medicare?
The Centers for Medicare & Medicaid Services (CMS) notes that a "routine physical examination" is not covered by Medicare.
How often does Medicare cover PSA?
When does Medicare cover the PSA test? All men over 50 are eligible to receive a free PSA test once every 12 months under the preventive services benefits included in Medicare Part B. If your doctor accepts Medicare assignment, you pay nothing. If your doctor does not accept Medicare assignment, you may pay a fee for the doctor services, ...
What is a PSA test?
A PSA test is a simple blood test that measures substances in the blood that may indicate the presence of prostate cancer. In a man with a healthy prostate, these substances, prostate-specific antigens, are present in the blood in very tiny amounts, usually less than 4 ng/mL. In a person with prostate cancer or other prostate abnormalities, ...