
Does Medicare cover oxygen devices?
Oct 18, 2017 · Medicare and 02 Coverage. Return to previous page. 10/18/2017; 3065 Views; 6 Answers; Last Activity: 3 years ago, Whylene McCray Tags: Medicare Question: 0. Jastro 4 years ago I Care; Report; Comment; Unlike I Care; Report ...
What does Medicare Part A&Part B cover?
If you have Medicare and use oxygen, you’ll rent oxygen equipment from a supplier for 36 months. After 36 months, your supplier must continue to provide oxygen equipment and related supplies for an additional 24 months. Your supplier must provide equipment and supplies for up to a total of 5 years, as long as you have a medical need for oxygen.
When did Medicare become the secondary payer?
Mar 03, 2022 · Medicare provides coverage for items and services for over 55 million beneficiaries. The vast majority of coverage is provided on a local level and developed by clinicians at the contractors that pay Medicare claims. However, in certain cases, Medicare deems it appropriate to develop a National Coverage Determination (NCD) for an item or …
What does Medicare Part a cover?
Get the basics. When you first enroll in Medicare and during certain times of the year, you can choose how you get your Medicare coverage. There are 2 main ways to get Medicare: Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare ...
Are oximeters covered by Medicare?
What is the Medicare requirement for oxygen saturation?
Does Medicare cover oxygen for pulmonary hypertension?
Is oxygen a Part B drug?
Does Medicare pay for pulse oximeter 2021?
Which of the following conditions qualify a patient for Medicare reimbursement for oxygen therapy in the home?
Does Medicare cover oxygen for congestive heart failure?
Effective September 27, 2021, the Centers for Medicare & Medicaid Services will not cover oxygen therapy and oxygen equipment in the home in the following circumstances: Angina pectoris in the absence of hypoxemia.
Does Medicare cover oxygen for pneumonia?
What diagnosis qualifies for home oxygen?
Will Medicare pay for the purchase of a portable oxygen concentrator?
When should oxygen be administered?
Does AARP cover portable oxygen?
Does Medicare cover oxygen equipment?
If you meet the conditions above, Medicare oxygen equipment coverage includes: Systems that provide oxygen. Containers that store oxygen. Tubing and related oxygen accessories for the delivery of oxygen and oxygen contents. Medicare may also pay for a humidifier when it's used with your oxygen machine.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B deductible applies.
What is Part B insurance?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers the rental of oxygen equipment and accessories as durable medical equipment (DME) that your doctor prescribes for use in your home.
How long does an oxygen supply last?
After 36 months, your supplier must continue to provide oxygen equipment and related supplies for an additional 24 months. Your supplier must provide equipment and supplies for up to a total of 5 years, as long as you have a medical need for oxygen.
How many people does Medicare cover?
Medicare provides coverage for items and services for over 55 million beneficiaries. The vast majority of coverage is provided on a local level and developed by clinicians at the contractors that pay Medicare claims. However, in certain cases, Medicare deems it appropriate to develop a National Coverage Determination ...
Does Medicare have a national coverage determination?
However, in certain cases, Medicare deems it appropriate to develop a National Coverage Determination (NCD) for an item or service to be applied on a national basis for all Medicare beneficiaries meeting ...
How much does Medicare pay for Part B?
For Part B-covered services, you usually pay 20% of the Medicare-approved amount after you meet your deductible. This is called your coinsurance. You pay a premium (monthly payment) for Part B. If you choose to join a Medicare drug plan (Part D), you’ll pay that premium separately.
What is the original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). (Part A and Part B) or a.
What is Medicare Advantage Plan?
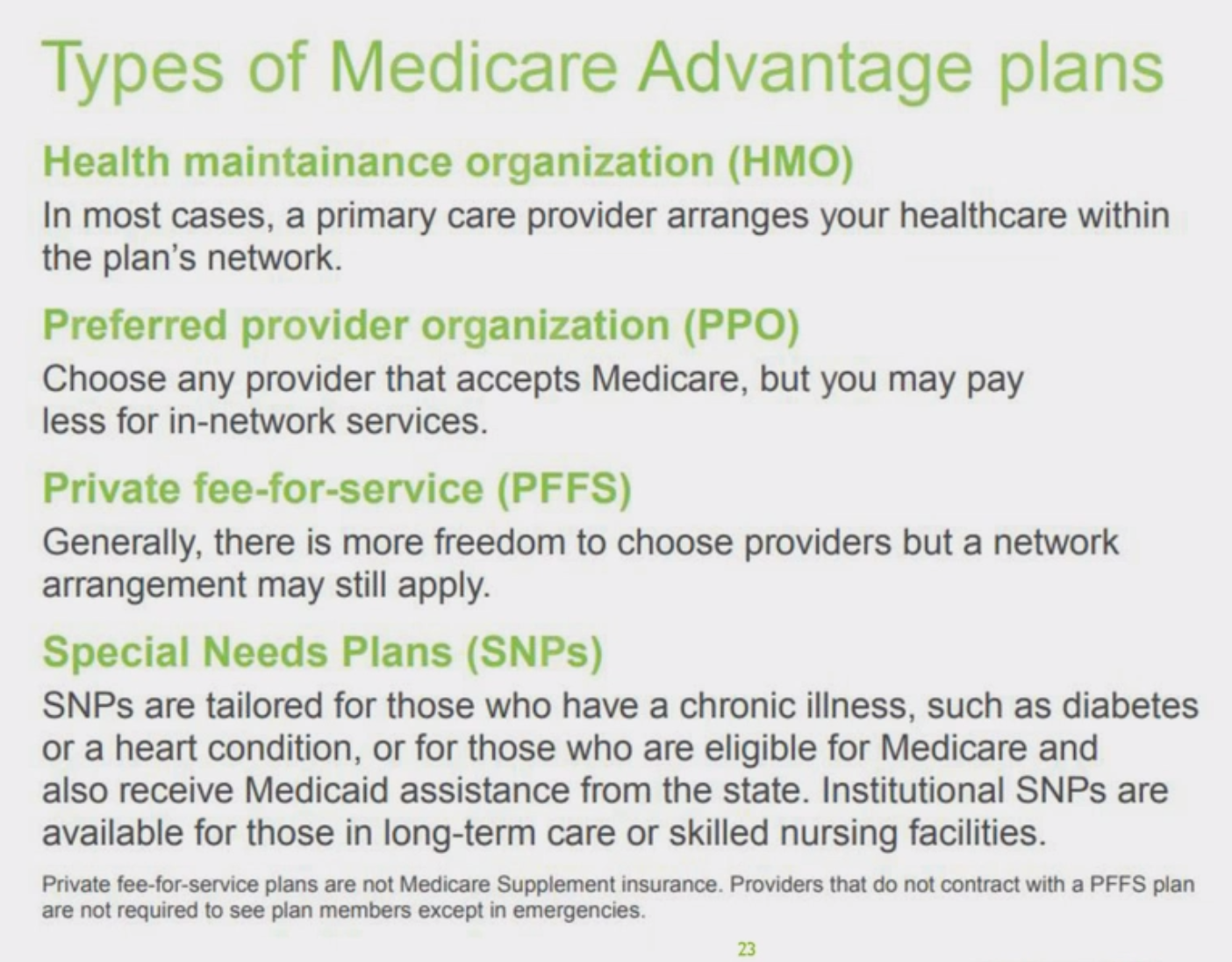
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
Does Medicare Advantage cover prescriptions?
Most Medicare Advantage Plans offer prescription drug coverage. . Some people need to get additional coverage , like Medicare drug coverage or Medicare Supplement Insurance (Medigap). Use this information to help you compare your coverage options and decide what coverage is right for you.
What are the benefits of Medicare Advantage?
Medicare Advantage (also known as Part C) 1 Medicare Advantage is an “all in one” alternative to Original Medicare. These “bundled” plans include Part A, Part B, and usually Part D. 2 Plans may have lower out-of-pocket costs than Original Medicare. 3 In many cases, you’ll need to use doctors and other providers who are in the plan’s network and service area for the lowest costs. 4 Most plans offer extra benefits that Original Medicare doesn’t cover—like vision, hearing, dental, and more.
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is Part B?
Part B covers 2 types of services. Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
What is preventive care?
Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best. You pay nothing for most preventive services if you get the services from a health care provider who accepts. assignment.
What is medically necessary?
Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
Does Medicare cover tests?
Medicare coverage for many tests, items and services depends on where you live. This list only includes tests, items and services (both covered and non-covered) if coverage is the same no matter where you live. If your test, item or service isn’t listed, talk to your doctor or other health care provider about why you need certain tests, ...
What to do if your test isn't listed on Medicare?
If your test, item or service isn’t listed, talk to your doctor or other health care provider about why you need certain tests, items or services. Ask if Medicare will cover them.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
What is ESRD in Medicare?
End-Stage Renal Disease (ESRD): Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD. Individual has ESRD, is covered by a Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA plan) ...
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
Is Medicare the primary payer?
Medicare remains the primary payer for beneficiaries who are not covered by other types of health insurance or coverage. Medicare is also the primary payer in certain instances, provided several conditions are met.
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
What is conditional payment?
A conditional payment is a payment Medicare makes for services another payer may be responsible for.
Does Medicare cover oxygen?
Medicare recipients may have coverage for oxygen devices they need. Medicare Part B (Medical Insurance) includes coverage for medically necessary services and supplies, including benefits for durable medical equipment (DME).
What is Medicare Part B?
Medicare Part B (Medical Insurance) includes coverage for medically necessary services and supplies, including benefits for durable medical equipment (DME). DME includes a wide range of medical equipment, including oxygen supplies, such as the systems, storage containers, tubing and associated accessories needed to transport the oxygen.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
NON-MEDICAL NECESSITY COVERAGE AND PAYMENT RULES#N#For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements.
ICD-10-CM Codes that Support Medical Necessity
The presence of an ICD-10 code listed in this section is not sufficient by itself to assure coverage. Refer to the section on “ Coverage Indications, Limitations and/or Medical Necessity ” for other coverage criteria and payment information.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
