Is Medicare considered insurance?
Medicare is an insurance program. Medical bills are paid from trust funds which those covered have paid into. It serves people over 65 primarily, whatever their income; and serves younger disabled people and dialysis patients.
Is Medicare primary or secondary?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
Is Medicare considered a Social Security benefit?
Are Social Security and Medicare the same thing? A: They're not the same thing, but they do have many similarities, and most older Americans receive benefits simultaneously from both programs.
Is Medicare always the primary insurance?
If you don't have any other insurance, Medicare will always be your primary insurance. In most cases, when you have multiple forms of insurance, Medicare will still be your primary insurance.
Is Medicare a 3rd party insurance?
Federal statutes also assign responsibility when an individual is covered by more than one public program. Generally, Medicare and other state and federal programs can be liable third parties unless specifically excluded by federal statute.
When Medicare is the secondary payer?
The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the remaining costs. If your group health plan or retiree coverage is the secondary payer, you may need to enroll in Medicare Part B before they'll pay.
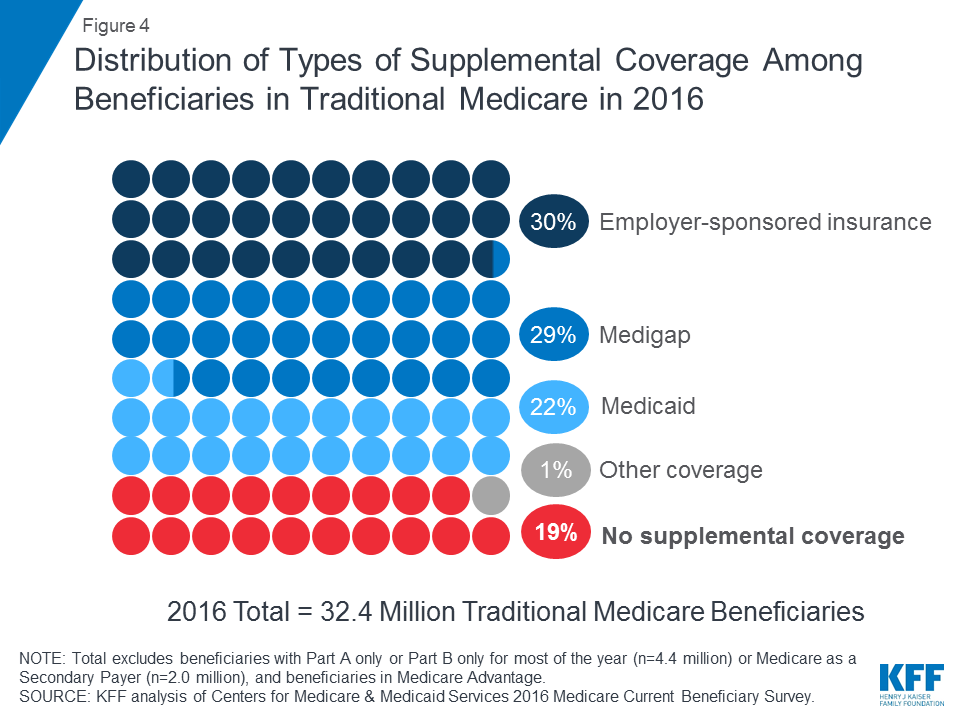
What is the difference between Medicare and Medicaid?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
Is SSI and Medicare the same?
People with SSI benefits are covered by Medi-Cal (California's Medicaid Program), not Medicare. Note: Some SSDI beneficiaries who had a short work history are eligible for a small SSDI income benefit and a supplementary SSI income benefit. For more information on SSI, see our Medi-Cal section.
Is Medicaid the same as Social Security?
Medicaid only provides medical benefits. Social Security provides a direct cash payment. 3. For both programs, your disability must substantially harm your ability to work.
What insurance is primary or secondary?
Primary insurance pays first for your medical bills. Secondary insurance pays after your primary insurance. Usually, secondary insurance pays some or all of the costs left after the primary insurer has paid (e.g., deductibles, copayments, coinsurances).
What is the primary insurance?
Primary insurance is health insurance that pays first on a claim for medical and hospital care. In most cases, Medicare is your primary insurer.
Can I have Medicare and private insurance at the same time?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
What is the benefit of Medicare?
One of the primary benefits of Medicare as a social program is that the financial risk is distributed across the working population. This means that the nation as a whole assumes financial risk for factors that might raise someone’s premiums substantially.
How is Medicare funded?
While Medicare is funded primarily through taxes, there are actually several sources of funding. It’s important to understand the financing behind Medicare because the future of the program largely depends on continued funding from individual taxes and other sources. Social programs only succeed in light of their perceived benefit versus the amount of money it takes to sustain them. These programs fail when they lose financial and moral support. In this section, we’ll give you a basic overview of how Medicare is funded so that you’re familiar with its impact on the economy and the healthcare industry as a whole.
What is HMO in healthcare?
Lawmakers approved the cooperation between Medicare and health maintenance organizations (HMOs). HMOs act as liaisons between healthcare providers and beneficiaries. People who subscribe to HMO plans usually have to go to a select list of providers that has been approved by the HMO administrators.
How long did it take for Medicare to become law?
However, the path to Medicare wasn’t always smooth sailing. A bill for socialized healthcare was first introduced in 1957, and it took eight years for Medicare to become law. The Johnson administration and lawmakers at the time debated extensively on the concept.
What changes have affected Medicare?
One of the changes that had the biggest impact on Medicare was the decision to include people with certain disabilities as beneficiaries of the program. People with end-stage renal disease (ESRD) or Lou Gehrig’s disease can receive Medicare benefits if they also receive Social Security Disability Insurance.
How much does an employer pay for Medicare?
For people who work for an employer, the employer pays half of the Medicare tax while the worker pays the other half. The Medicare tax rate is 2.9 percent, which means that an employer pays 1.45 percent while the remaining 1.45 percent is deducted from the employee’s wages.
What is Medicare's coverage for speech therapy?
These forms of care help seniors, particularly those with disabilities, to achieve alternate forms of medical treatments.
What is the goal of Medicare?
The overall goal of Medicare is to provide senior citizens and other individuals suffering from disease or disability with reliable and affordable medical coverage. The most well known portions of Medicare are the original Part A and Part B. Medicare Part A provides individuals with beneficial coverage related to inpatient hospital stays, ...
What is Medicare Advantage Plan?
Medicare Part C, or the Medicare Advantage Plan, allows individuals to get their Part A, B, and D coverage all in one plan from a private insurance company that is working under contract with Medicare.
What is Medicare Part B?
Medicare Part B provides coverage and benefits related to general medical care from doctors such as checkups, exams, and necessary durable medical equipment. In addition to the full coverage Medicare Part A and B provide, individuals can enroll in Medicare Part D and take advantage of the programs prescription drug benefits.
Is Medicare a perfect system?
Medicare may not be a perfect system, but it was designed with honest intentions. To date, the program still provides senior citizens the benefit of health insurance at rates that most can afford while private insurance programs continue to experience skyrocketing prices.
Does Medicare Part D cover all prescriptions?
Medicare Part D provides prescription drug coverage for those individuals with Medicare, however it comes in roughly 1,800 different forms and plans may not cover all the drugs an individual has been prescribed. A Medicare Advantage Plan has its benefits as well.
Does Medicare cover mental health?
There are of course other Medicare benefits outside of the traditional items covered under Part A, B, and D. Medicare covers a wide range of “wellness” services as well as mental health, home health care, hospice, and long term care. Medicare now covers inpatient and outpatient mental health services provided by psychiatrists, psychologists, ...
Is Medicare a basic premise?
Most Americans, adults in particular, are familiar with the basic premise of the Medicare program operating in this country. However, those who are not taking advantage of the coverage Medicare offers may not be familiar with all the Medicare benefits that can be provided.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is Medicare Advantage?
Medicare Advantage, also known as Medicare Part C, is a type of health plan offered by private insurance companies that provides the benefits of Parts A and Part B and often Part D (prescription drug coverage) as well. These bundled plans may have additional coverage, such as vision, hearing and dental care.
What is not covered by Medicare?
The biggest potential expense that’s not covered is long-term care, also known as custodial care. Medicaid, the federal health program for the poor, pays custodial costs but typically only for low-income people with little savings. Other common expenses that Medicare doesn’t cover include:
How long do you have to sign up for Medicare Part B?
You can avoid the penalty if you had health insurance through your job or your spouse’s job when you first became eligible. You must sign up within eight months of when that coverage ends.
What are the most common medical expenses that are not covered by Medicaid?
The biggest potential expense that’s not covered is long-term care, also known as custodial care . Medicaid, the federal health program for the poor, pays custodial costs but typically only for low-income people with little savings. Hearing aids and exams for fitting them. Eye exams and eyeglasses.
Does Medicare Part A cover hospice?
Part A also helps pay for hospice care and some home health care. Medicare Part A has a deductible ($1,484 in 2021) and coinsurance, which means patients pay a portion of the bill. There is no coinsurance for the first 60 days of inpatient hospital care, for example, but patients typically pay $371 per day for the 61st through 90th day ...
Is Medicare the same as Medicaid?
No. Medicare is an insurance program, primarily serving people over 65 no matter their income level. Medicare is a federal program, and it’s the same everywhere in the United States. Medicaid is an assistance program, serving low-income people of all ages, and patient financial responsibility is typically small or nonexistent.
Does Medicare cover eye exams?
Medicare also doesn’t cover eye exams for eyeglasses or contact lenses. Some Medicare Advantage Plans (Medicare Part C) offer additional benefits such as vision, dental and hearing coverage. To find plans with coverage in your area, visit Medicare’s Plan Finder.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
Do you pay more for outpatient services in a hospital?
For services that can also be provided in a doctor’s office, you may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office . However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What does Medicare Part A cover?
Medicare Part A covers the care you receive when you’re admitted to a facility like a hospital or hospice center. Part A will pick up all the costs while you’re there, including costs normally covered by parts B or D.
What is Medicare for seniors?
Medicare is a health insurance program for people ages 65 and older, as well as those with certain health conditions and disabilities. Medicare is a federal program that’s funded by taxpayer contributions to the Social Security Administration.
What is the maximum amount you can pay for Medicare in 2021?
In 2021, the out-of-pocket maximum for plans is $7,550. Note.
What are the parts of Medicare?
Each part covers different healthcare services you might need. Currently, the four parts of Medicare are: Medicare Part A. Medicare Part A is hospital insurance. It covers you during short-term inpatient stays in hospitals and for services like hospice.
How many people are on medicare in 2018?
Medicare is a widely used program. In 2018, nearly 60,000 Americans were enrolled in Medicare. This number is projected to continue growing each year. Despite its popularity, Medicare can be a source of confusion for many people. Each part of Medicare covers different services and has different costs.
How old do you have to be to get Medicare?
You can enroll in Medicare when you meet one of these conditions: you’re turning 65 years old. you’ve been receiving Social Security Disability Insurance (SSDI) for 24 months at any age. you have a diagnosis of end-stage renal disease (ESRD) or amyotrophic lateral sclerosis (ALS) at any age.
When does Medicare enrollment start?
It begins 3 months before your birth month, includes the month of your birthday, and extends 3 months after your birthday. During this time, you can enroll for all parts of Medicare without a penalty. General enrollment period (January 1–March 31).