This section contains five-character HCPCS Level II (national), interim codes, and three or four-character Health Insurance Portability and Accountability Act (HIPAA)-compliant revenue codes used for billing. This list is arranged in alphabetical order by service “description.” Although interim codes are not used to bill Medicare, they are included to assist providers in determining the “type of service” not covered by Medicare.
Do Medicare payers accept s codes?
Dental Medicare denial not necessary. Explanation of Medicare benefits (EOMB) not necessary for ambulatory surgery centers for ICD-10-CM codes G50.0 thru G51.9 or K00.0 thru K08.99. H0033 Directly Observed Therapy (DOT) Always A9273, A9274, A9279, A9281, E0240 thru E0248, E0273, E0625 DME Always
What do providers need to know about CPT code descriptors?
Version 1.0 – July 30, 2015 MEDICARE PROVIDER ENROLLMENT ELIGIBILITY REFERENCE TABLE. 1. Physicians and Non Physicians Permitted to Enroll in Medicare Non Physicians NOT Permitted to Enroll in Medicare
Why are the digits of the Category III codes missing from CPT?
Medicare does not cover items and services that are not reasonable and necessary for the diagnosis or treatment of an illness or injury or to improve the functioning of a malformed body member. Section 1862(a)(1) of the Social Security Act is the basis for denying payment for types of care, or specific items, services or procedures that are not ...
Are S codes accepted by private payers?
Medicare and other federal payers do not recognize "S" codes; however, "S" codes may be useful for claims to what type of insurers? G, K, Q List the temporary code letters for procedures or services that are not established by private payers or Medicaid. Administration of the drug HCPCS codes J9000-J9999 cover the cost of the chemotherapy drug.

What types of codes are not recognized by Medicare and other federal payers?
Medicare and other federal payers do not recognize "S" codes; however, "S" codes may be useful for claims to what type of insurers? List the temporary code letters for procedures or services that are not established by private payers or Medicaid.
What modifiers are not accepted by Medicare?
Medicare will automatically reject claims that have the –GX modifier applied to any covered charges. Modifier –GX can be combined with modifiers –GY and –TS (follow up service) but will be rejected if submitted with the following modifiers: EY, GA, GL, GZ, KB, QL, TQ.
Are H codes covered by Medicare?
Medicare pays for some Level II codes, including A, G, J codes; Medicare does NOT pay for H (State mental health codes), S, or T codes. H codes are for Medicaid only.
Are C codes only for Medicare?
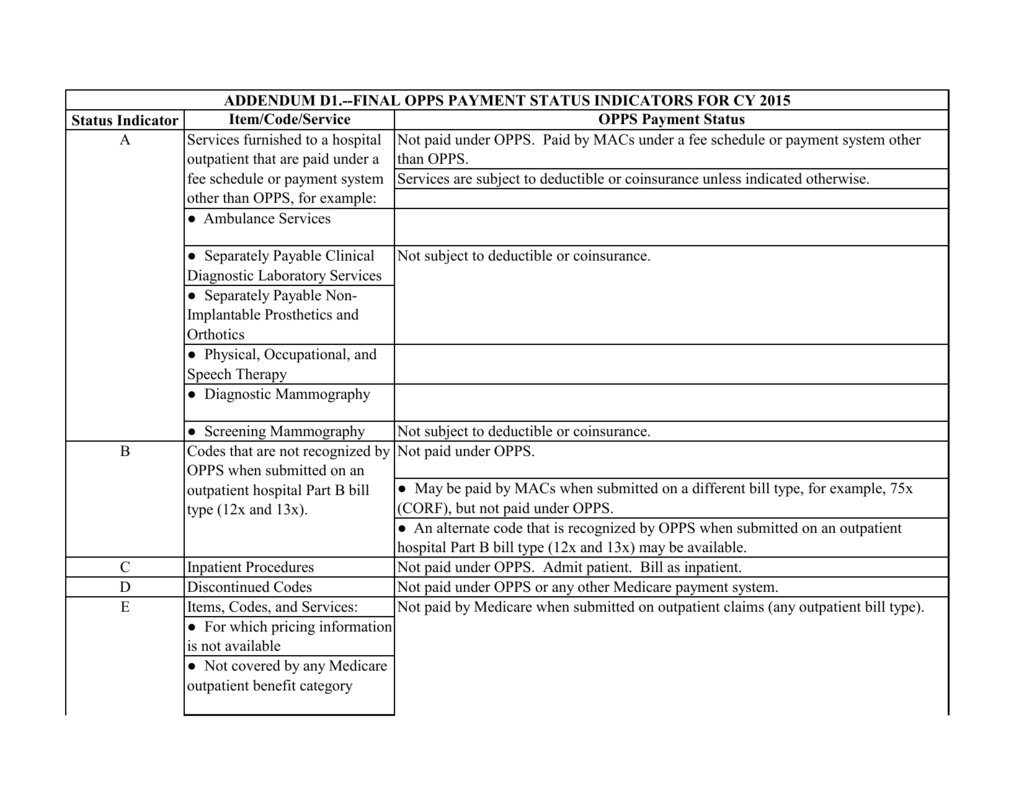
C-codes are unique temporary pricing codes established for the Prospective Payment System and are only valid for Medicare on claims for hospital outpatient department services and procedures.Jun 26, 2006
Which of the following is not covered by Medicare?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Which of the following is not covered with Medicare Part A?
Part A does not cover the following: A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care.
What are the 3 categories of CPT codes?
These codes are utilized to communicate with: other physicians, hospitals, and insurers for claims processing. There are three categories of CPT Codes: Category I, Category II, and Category III.Aug 16, 2017
What are HCPCS S codes?
Q. What is an S code? A.S codes are a set of Healthcare Common Procedure Coding System (HCPCS) codes that were originally requested by Blue Cross/Blue Shield. The codes are listed by the Centers for Medicaid & Medicare Services (CMS), but they are never for use on claims filed to Medicare.Dec 16, 2006
What are the four types of HCPCS codes?
5.20: CPC Exam: HCPCS Level IIA-codes: Transportation, Medical and Surgical Supplies, Miscellaneous and Experimental.B-codes: Enteral and Parenteral Therapy.C-codes: Temporary Hospital Outpatient Prospective Payment System.D-codes: Dental codes.E-codes: Durable Medical Equipment.More items...
What are T codes in medical billing?
CPT Category III codes are a set of temporary (T) codes assigned to emerging technologies, services, and procedures. These codes are intended to be used for data collection to substantiate more widespread usage or to provide documentation for the Food and Drug Administration (FDA) approval process.
What are HCPCS G codes used for?
G-codes are used to report a beneficiary's functional limitation being treated and note whether the report is on the beneficiary's current status, projected goal status, or discharge status.Dec 1, 2021
Are there ICD 10 procedure codes?
ICD-10-PCS will be the official system of assigning codes to procedures associated with hospital utilization in the United States. ICD-10-PCS codes will support data collection, payment and electronic health records. ICD-10-PCS is a medical classification coding system for procedural codes.
When will Medicare pay for a test?
Medicare will make payment only when a service is accepted as effective and proven. Some tests or services are obsolete and have been replaced by more advanced procedures. The tests or procedures may be paid only if the physician who performs them satisfactorily justifies the medical need for the procedure (s).
Why do contractors specify bill types?
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service . Absence of a Bill Type does not guarantee that the policy does not apply to that Bill Type.
Is FDA approved CPT code medically reasonable?
It is important to note that the fact that a new service or procedure has been issued a CPT code or is FDA-approved does not, in itself, make the procedure medically reasonable and necessary.
Is Trailblazer a non-covered service?
A service or procedure on the “Local Non-Coverage Decisions” list is always denied on the basis that TrailBlazer does not believe it is ever medically reasonable and necessary. The TrailBlazer list of LCD exclusions contains procedures that, for example, are: Experimental. Not proven safe and effective.
Can I get paid for medical procedures that have not been approved by the FDA?
Program payment, therefore, may not be made for medical procedures and services performed using devices that have not been approved for marketing by the FDA or for those not included in an FDA-approved Investigational Device Exemption (IDE) trial.
