When does Medicare start after disability?
Medicare coverage kicks in for most SSDI recipients two years after the first month they are eligible for their monthly disability benefits. However, this doesn’t automatically mean that every person approved for SSDI must wait two years to get their Medicare coverage. The two-year Medicare waiting period generally gets calculated from the date of your SSDI entitlement (the date you are eligible to receive your monthly award).
When can I go out on disability?
you're under 65 years old. you have a severe and prolonged mental or physical disability. your disability prevents you from working on a regular basis. The benefits include payments to children of a person with a disability. Apply as early as possible if you think you're eligible for CPP disability benefits.
Can someone on disability get Medicaid?
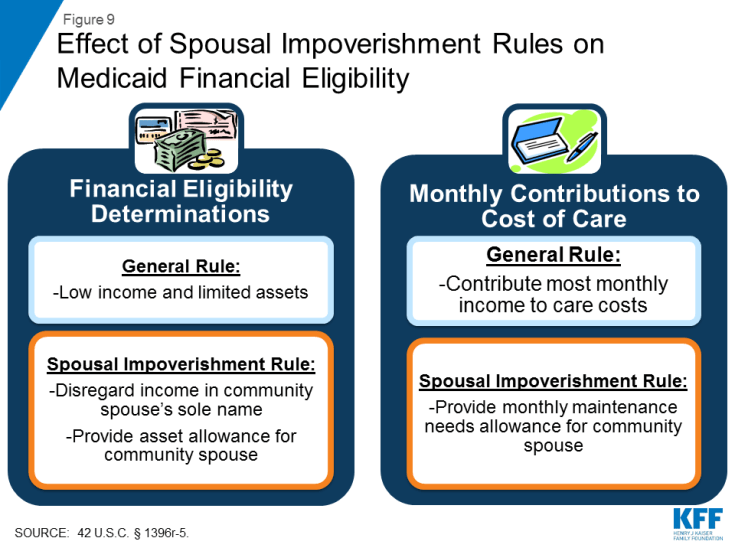
Medicaid disability coverage may be available if you have a qualifying disabling condition and if you meet certain other requirements such as having limited financial resources. Determining if you are able to get Medicaid can be complicated, so it is best to speak with an experienced attorney about what your rights and options are.
Can you get a job when you have a disability?
You can work as long as your countable income doesn't go above the SSI income limit. One of the basic requirements for getting approved for disability benefits is that your medical condition is so severe it prevents you from performing a substantial amount of work.
How long do you have to wait to get Medicare?
In most cases, you’ll need to wait 24 months before your Medicare coverage begins. There is a 2-year waiting period that begins the first month you receive a Social Security benefit check.
How long does a disability last?
Generally, this means you are unable to work and that your condition is expected to last for at least a year. Medicare doesn’t determine who is eligible for disability coverage.
How much is Medicare Part B 2021?
The standard Part B premium for 2021 is $148.50 per month. The deductible for Medicare Part B in 2021 is $203. After you meet the deductible, some services are covered in full. You’ll pay 20 percent of the Medicare-approved amount for other services.
How much is hospitalization for Medicare Part A 2021?
In 2021, hospitalization costs with Medicare Part A include: Deductible: $1,484 for each benefit period. Days 1–60: after the deductible has been met, inpatient stays will be completely covered until the 60th day the benefit period. Days 61–90: $371 per day coinsurance.
When does Medicare start covering ALS?
If you have amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s Disease, you’ll be enrolled in coverage in the first month you receive SSDI. If you have end stage renal disease (ESRD), your Medicare coverage normally begins after you’ve received 3 months of dialysis treatment.
Can I get Medicare Part B after 24 months?
The takeaway. Medicare coverage is available for people with a disability who receive SSDI. You’ll automatically be enrolled in parts A and B after your 24th month of SSDI benefits. You can choose to decline Medicare Part B coverage if you have other options that work better for your budget.
How long can you wait to get Medicare if you are disabled?
But, because Social Security only allows a maximum of 12 months of retroactive benefits, plus the 5-month waiting period for benefits, the earliest that you can become eligible for Medicare is one year ...
How long does it take to get Medicare after receiving SSDI?
Qualifying for Medicare When Receiving Disability Benefits. Medicare coverage kicks in for most SSDI recipients two years after the first month they are eligible for their monthly disability benefits. However, this doesn’t automatically mean that every person approved for SSDI must wait two years to get their Medicare coverage.
How long is the waiting period for Medicare?
The two-year Medicare waiting period generally gets calculated from the date of your SSDI entitlement (the date you are eligible to receive your monthly award). Normally, this is the date your disability began plus the five-month SSDI waiting period.
When will Medicare start?
Since it has been two years since your Date of Entitlement, you will start receiving Medicare benefits in December 2018. But, if you recently become disabled and were approved with an entitlement date of August 2018, you would not become eligible to receive Medicare benefits until August 2020.
Do you have to wait to receive medicaid if you are on SSI?
For SSI recipients, there is no waiting period to receive Medicaid.
Do you get Medicaid if you are approved for SSI?
In most states, if you are approved for SSI, you will receive benefits automatically through Medicaid as SSI’s income and asset limits mirror that of Medicaid’s .
How long do you have to pay Medicare if you are on disability?
Once an individual goes back to work, they do not have to pay Part A premiums for the first 8 years and 6 months. After this time, however, they must pay the Part A premiums.
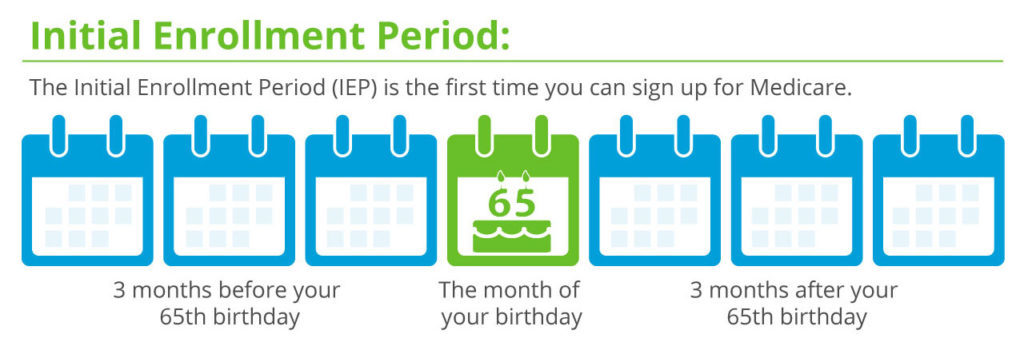
How long do you have to be on Medicare?
A person with a disability who wishes to enroll in either Medicare Part D or an Advantage plan may do so during: 1 the 7-month period that begins 3 months before the 25th month of Social Security disability benefits 2 the 7-month period that includes the 25th month of disability benefits 3 the 7-month period that stops after the 25th month of disability benefits
How long does Medicare Part D last?
A person with a disability who wishes to enroll in either Medicare Part D or an Advantage plan may do so during: the 7-month period that begins 3 months before the 25th month of Social Security disability benefits . the 7-month period that includes the 25th month of disability benefits.
What is the cost of Medicare Advantage Plan 2020?
The average premium for a Medicare Advantage plan that includes prescription drug coverage is $36 per month in 2020. A person with an Advantage plan must also pay the Part B monthly premium of $148.50.
Does Medicare cover nursing home stays?
Through Medicare, healthcare coverage for a person with a disability is identical to the coverage for an individual who qualifies because of their age . Areas of coverage include certain hospital and nursing home stays, along with doctor visits and community-based services.
Does Medicare Part D include prescriptions?
Part D and Medicare Advantage costs. The coverage from parts A and B does not include prescription drug costs. Coverage for prescribed medication is known as Medicare Part D. A person may wish to include Part D as part of their plan, or they may decide to explore available options through Medicare Advantage.
How long do you have to wait to get Medicare if you have Social Security Disability?
Social Security Disability Insurance (SSDI) & Medicare coverage. If you get Social Security Disability Income (SSDI), you probably have Medicare or are in a 24-month waiting period before it starts. You have options in either case.
What is SSI disability?
Supplemental Security Income (SSI) Disability & Medicaid coverage. Waiting for a disability status decision and don’t have health insurance. No disability benefits, no health coverage. The Marketplace application and disabilities. More information about health care for people with disabilities.
Can I enroll in a Medicare Marketplace plan if I have Social Security Disability?
You’re considered covered under the health care law and don’t have to pay the penalty that people without coverage must pay. You can’t enroll in a Marketplace plan to replace or supplement your Medicare coverage.
Can I keep my Medicare Marketplace plan?
One exception: If you enrolled in a Marketplace plan before getting Medicare, you can keep your Marketplace plan as supplemental insurance when you enroll in Medicare. But if you do this, you’ll lose any premium tax credits and other savings for your Marketplace plan. Learn about other Medicare supplement options.
Can I get medicaid if I have SSDI?
You may be able to get Medicaid coverage while you wait. You can apply 2 ways: Create an account or log in to complete an application. Answer “ yes” when asked if you have a disability.
Can I get medicaid if I'm turned down?
If you’re turned down for Medicaid, you may be able to enroll in a private health plan through the Marketplace while waiting for your Medicare coverage to start.
How long do you have to wait to receive medicare if you have SSDI?
For more information on calculating how this is calculated, see our article on when you'll receive Medicare benefits. There is no waiting period for SSI recipients to receive Medicaid.
Which states have a lower income limit for Medicaid?
There are a few states, including Illinois and Ohio, that are exceptions to this rule. These states may have a lower income or asset limit for the Medicaid program than the SSI program, so they make their own Medicaid determinations.
Do you get medicaid if you are approved for SSI?
Do you get Medicare coverage if you were approved for SSI? Claimants who are approved for SSI only typically receive Medicaid coverage in most states. And like SSI, Medicaid is subject to income and asset limitations. Medicaid is a needs-based, state- and county-administered program that provides for a number of doctor visits and prescriptions each month, as well as nursing home care under certain conditions.#N#Can you ever get Medicare if you get SSI? Medicare coverage for SSI recipients does not occur until an individual reaches the age of 65 if they were only entitled to receive monthly SSI disability benefits. At the age of 65, these individuals are able to file an "uninsured Medicare claim," which saves the state they reside in the cost of Medicaid coverage. Basically, the state pays the medical premiums for an uninsured individual to be in Medicare so that their costs in health coverage provided through Medicaid goes down.
Do you get medicaid if you are on SSDI?
If you're approved for disability benefits, you'll also get Medicare or Medicaid, depending on whether you receive SSDI or SSI benefits. Disabled people who are approved for Social Security disability insurance (SSDI) benefits will receive Medicare, and those who are approved for Supplemental Security Income (SSI) will receive Medicaid.
Can I get concurrent disability from both SSI and SSDI?
Some disability recipients will be approved for concurrent benefits; that is, they will draw disability money from both SSDI and SSI. In such instances, the issue of whether a claimant will get Medicare or Medicaid is not so cut and dry. Claimants who are approved for concurrent disability benefits should consult their local Social Security office ...
How long does a child have to be disabled to qualify for Medicare?
Disability benefits through SSA can be granted at any age. Once a disability beneficiary is at least 20 years old and has been declared disabled for 24 continuous months, they can qualify for Medicare. Only a child diagnosed with End-Stage Renal Disease (ESRD) ...
How old do you have to be to qualify for Medicare?
If you're age 65 or older, you will typically qualify for Medicare automatically. But you can also qualify for Medicare if you have a disability as determined by the Social Security Administration (SSA) if you're at least 20 years old.
What are the different types of disability?
The SSA determines disability eligibility through the examination of medical records, expert consults and a claimant's self-report of activity limitations. The scope and severity of health issues that lead to disability determinations are different for each individual. The SSA categorizes disabilities into the following groups : 1 Sensory and speech disorders 2 Musculoskeletal conditions 3 Cardiovascular and respiratory illnesses 4 Neurological disorders 5 Cancer and immune system disorders 6 Mental health conditions 7 Congenital disorders 8 Endocrine and digestive conditions 9 Skin disorders
How long can you be on Medicare if you have both SSI and SSDI?
Regardless of which disability benefit you receive, you will not become eligible for Medicare until you've been disabled for 24 months.
How does the SSA determine disability eligibility?
The SSA determines disability eligibility through the examination of medical records, expert consults and a claimant's self-report of activity limitations. The scope and severity of health issues that lead to disability determinations are different for each individual.
What is the difference between SSDI and SSI?
Types of Social Security Disability Benefits: SSI vs. SSDI. Most people are awarded either Supplemental Security Income (SSI) or Social Security Disability Insurance (SSDI) benefits. SSI is based on financial need, and SSDI is awarded if you have a minimum work history. Individuals with SSI may qualify for Medicaid in their home state.
Does Medicare cover special needs?
Medicare plans for individuals with special needs offer coverage for services typically covered by traditional Medicare with the addition of enhanced benefits, such as vision, dental, transportation assistance and meal delivery. Furthermore, you can transition to a special needs plan as soon as you meet the criteria.
How long is a person eligible for Medicare?
Everyone eligible for Social Security Disability Insurance (SSDI) benefits is also eligible for Medicare after a 24-month qualifying period. The first 24 months of disability benefit entitlement is the waiting period for Medicare coverage. During this qualifying period for Medicare, the beneficiary may be eligible for health insurance ...
How long can you keep Medicare after you return to work?
Answer: As long as your disabling condition still meets our rules, you can keep your Medicare coverage for at least 8 ½ years after you return to work. (The 8 ½ years includes your nine month trial work period.) Question: I have Medicare hospital Insurance (Part A) and medical insurance (Part B) coverage.
Why does Bill have Medicare?
Example: Bill has Medicare coverage because of permanent kidney failure. He also has group health plan coverage through the company he works for. His group health coverage will be his primary payer for the first 30 months after Bill becomes eligible for Medicare. After 30 months, Medicare becomes the primary payer.
How to order a publication from Medicare?
Answer: You can view, print, or order publications online or by calling 1-800-MEDICARE (1-800-633-4227). The fastest way to get a publication is to use our search tool and then view and print it. If you order online or through 1-800-MEDICARE, you will receive your order within 3 weeks. The link to search publications is at: http://www.medicare.gov/Publications/home.asp
Is Medicare a secondary payer?
Answer: Medicare may be the "secondary payer" when you have health care coverage through your work. See the information under "Coordination of Medicare and Other Coverage for Working Beneficiaries with Disabilities" about when Medicare is a "secondary payer or primary payer".
Does Medicare pay for non-VA hospital?
If the VA authorizes services in a non-VA hospital, but doesn't pay for all of the services you get during your hospital stay, then Medicare may pay for the Medicare-covered part of the services that the VA does not pay for. Example: John, a veteran, goes to a non-VA hospital for a service that is authorized by the VA.
Does Medicare pay for the same service?
Medicare cannot pay for the same service that was covered by Veterans benefits, and your Veterans benefits cannot pay for the same service that was covered by Medicare. You do not have to go to a Department of Veterans Affairs (VA) hospital or to a doctor who works with the VA for Medicare to pay for the service.