When can I Change my Medicare plan?
If you enroll during your Initial Enrollment Period, you can also make changes anytime in the first 3 months of your Medicare coverage. “After that, you can switch plans during open enrollment in the Fall or during Medicare Advantage open enrollment, which is at the beginning of each year,” Dworetsky says.
When can I enroll in a Medicare supplement plan?
When can I enroll in a Medicare Supplement Plan? When newly eligible for Medicare, you enter a seven-month Initial Enrollment Period (IEP) which begins three months before your 65th birthday and ends three months after the month of your birthday.
Can I change Medicare Advantage plans during special enrollment period?
The only way to change Medicare Advantage Plans outside of the standard annual enrollment periods is by qualifying for a Special Enrollment Period. SEPs when you can change Medicare Advantage Plans include, but are not limited to: Moving outside of your current plan’s service area.
Can I make changes to my Medicare plan during the AEP?
Medicare beneficiaries can make changes to parts of their Medicare coverage – including their Medicare Advantage (Part C) and Prescription Drug Plans (Part D) – during Medicare’s Annual Enrollment Period (AEP) which takes place every year from October 15th to December 7th.
Can I change my Medicare plan at any time?
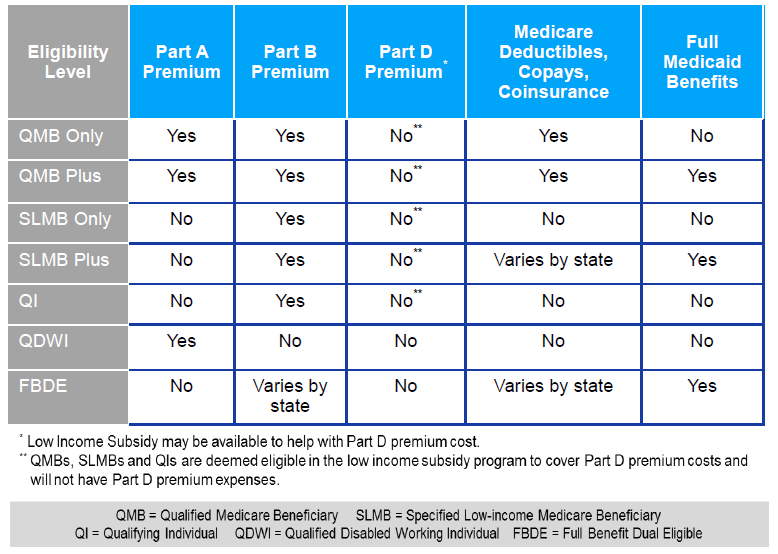
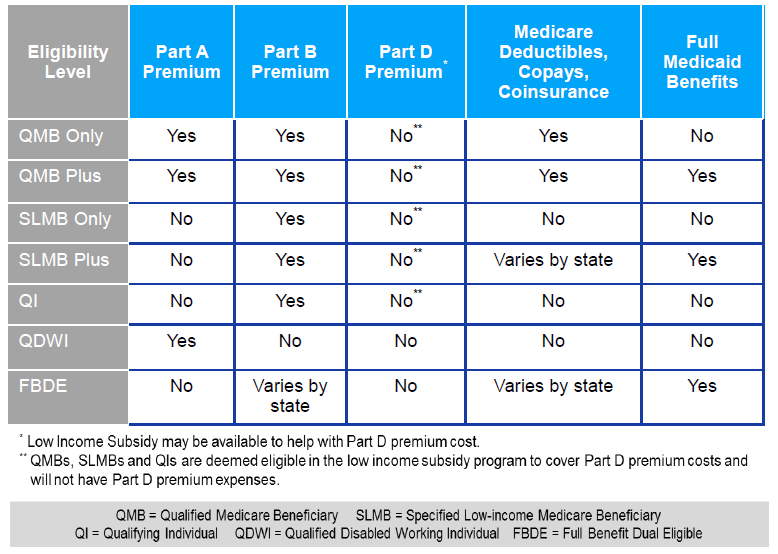
If you're covered by both Medicare and Medicaid, you can switch plans at any time during the year. This applies to Medicare Advantage as well as Medicare Part D.
When can I modify my Medicare plan?
Medicare provides certain time periods when you can change Medicare plans. The main one is the Medicare Annual Enrollment Period, which runs from October 15 to December 7 each year. Anyone on Medicare can make coverage changes during this time that then go into effect the following year.
When can a consumer enroll in a Medicare supplement plan?
Sign up for a Medicare Advantage Plan (with or without drug coverage) or a Medicare drug plan. During the 7‑month period that starts 3 months before the month you turn 65, includes the month you turn 65, and ends 3 months after the month you turn 65.
Can I change my Medicare supplement plan at any time during the year?
Changing Medicare supplement plans often requires you to go through medical underwriting. You can change Medicare supplement plans at any time of year – but in most states you will have to pass medical underwriting to do so.
How do you're enroll in Medicare?
If you're looking to reenroll in Medicare Part B, follow these steps:Go to the Social Security Administration website.Complete the application.Mail all required documents to the Social Security office. Include all required official or certified documents to allow for a seamless process.
When can you switch from Medicare Advantage to a Medicare supplement?
During the Medicare Advantage OEP From January 1 to March 31 each year, a person can switch from one Medicare Advantage plan to another or drop their Medicare Advantage plan altogether in favor of original Medicare. During this time, a person can also join a prescription drug plan and Medigap.
What are the Medicare enrollment periods?
You can sign up between January 1-March 31 each year. This is called the General Enrollment Period. Your coverage starts July 1. You might pay a monthly late enrollment penalty, if you don't qualify for a Special Enrollment Period.
What is the initial enrollment period for Medicare?
Initial Medicare Enrollment Period: Most people get Medicare Part A (Hospital Insurance) and Part B (Medical Insurance) during this period. It starts 3 months before you turn 65 and ends 3 months after you turn 65.
When can you enroll in Medicare Part D?
The first opportunity for Medicare Part D enrollment is when you're initially eligible for Medicare – during the seven-month period beginning three months before the month you turn 65. If you enroll prior to the month you turn 65, your prescription drug coverage will begin the first of the month you turn 65.
Can you switch from one Medigap plan to another?
. If you want to switch to a different Medigap policy, you'll have to check with your current or new insurance company to see if they'll offer you a different policy. If you decide to switch, you may have to pay more for your new Medigap policy.
Can I change Medicare supplement plans without underwriting?
During your Medigap Open Enrollment Period, you can sign up for or change Medigap plans without going through medical underwriting. This means that insurance companies cannot deny you coverage or charge you more for a policy based on your health or pre-existing conditions.
Can I switch from Plan N to Plan G?
You can switch from Plan N to Plan G any time during the year, but if you are outside your 6-month Open Enrollment window, then you may have to answer health questions to switch. Your approval is not guaranteed.
When Can I Sign Up For Medicare Part A and Part B?
If you’re already getting Social Security or Railroad Retirement Board benefits, usually you will be contacted a few months before you become eligi...
When Can I Sign Up For Prescription Drug Coverage?
You can sign up for stand-alone Medicare Part D Prescription Drug coverage during your Initial Enrollment Period.You must have Medicare Part A or P...
When Can I Enroll in A Medicare Advantage Plan?
You must have Medicare Part A and Medicare Part B to enroll in a Medicare Advantage plan. People can enroll in a Medicare Advantage plan for the fi...
When Can I Sign Up For A Medicare Supplement Insurance Plan?
There are no cost penalties for late enrollment, but your eligibility for some Medicare Supplement insurance plans can be impacted if you delay enr...
What Happens If I Miss My Medicare Supplement Open Enrollment period?
Your eligibility may be impacted if you miss the Medicare Supplement Open Enrollment Period: 1. Your application could be declined if you have a pr...
When Can You Change Your Medicare Advantage Or Medicare Part D Prescription Drug Coverage?
1. During your Initial Enrollment Period for Medicare, described above 2. During Medicare’s Annual Election Period 3. During a Special Election Per...
When Is Medicare’S Annual Election period?
1. The Medicare Advantage and Prescription Drug Plan Annual Election Period runs from October 15 to December 7 each year.
What Can You Do During The Annual Election Period (AEP)?
Plan benefits can change from year to year, so you have the option to change your Medicare coverage every year during Medicare’s Annual Election Pe...
How long is the free look period for Medigap?
If you’re within your six-month Medigap Open Enrollment Period and considering a different Medigap plan, you may try a new Medigap policy during a 30-day “free look period.”. During this period, you will have two Medigap plans, and pay the premium for both.
What is Medicare Supplement Insurance?
Medicare Supplement Insurance (Medigap or MedSup), sold by private companies, helps pay some health care costs that Original Medicare (Part A and Part B) doesn’t cover. Policies can include coverage for deductibles, coinsurance, hospital costs, skilled nursing facility costs, and sometimes health care costs when traveling outside the U.S.
What happens if a Medigap policy goes bankrupt?
Your Medigap insurance company goes bankrupt and you lose your coverage , or your Medigap policy coverage otherwise ends through no fault of your own. You leave a Medicare Advantage plan or drop a Medigap policy because the company hasn’t followed the rules, or it misled you.
What to Do if You Missed Medicare Annual Enrollment Period
If you miss the Medicare Annual Enrollment Period, there are a few circumstances in which you are allowed to change your coverage. Each year, there are five set times you can enroll in Medicare or change existing Medicare plans:
When can I change my Medicare Supplement Insurance plan?
There are limited circumstances in which you can change your Medicare Supplement plan, also known as Medigap. If you’re still within your Initial Enrollment Period (three months before and three months after your birth month), you have the option to switch your coverage.
When can I change my Medicare Part D plan?
In most cases, you can only make changes to your Medicare Part D coverage during the Annual Enrollment Period. If you have a Medicare Advantage plan, however, you can make changes to your Part D coverage during the Medicare Advantage Open Enrollment Period, which runs from January 1 to March 31 each year.
How to Change Medicare Plans During a Medicare Enrollment Period
If you are eligible to change your Medicare plan during one of the Medicare enrollment periods, SelectQuote can help you do so. We can help you understand your options for coverage and find a plan that includes the benefits you need at a price that fits your budget.
Want to switch Medicare plans? Let SelectQuote compare Medicare plans for you
If you need help understanding your enrollment and coverage options, save yourself time and the hassle of navigating the Medicare maze on your own. In just minutes, we can compare Medicare plans available to you from some of the most trusted insurance companies in the nation.
When can I join a health or drug plan?
Find out when you can sign up for or change your Medicare coverage. This includes your Medicare Advantage Plan (Part C) or Medicare drug coverage (Part D).
Types of Medicare health plans
Medicare Advantage, Medicare Savings Accounts, Cost Plans, demonstration/pilot programs, and Programs of All-inclusive Care for the Elderly (PACE).
When does Medicare open enrollment end?
Any changes that you make will take effect on January 1 of the following year. Medicare Advantage Open Enrollment Period. This open enrollment period applies to recipients who are currently using a Medicare Advantage plan. This period lasts from January 1 to March 31 each year, and during this time, you can make one change to your healthcare ...
When does Medicare kick in?
If you make a change during the Medicare Advantage Open Enrollment Period, your new Medicare benefits will kick in on the first day of the month following your enrollment. For example, if you make a change to your Medicare Advantage plan at any point during the month of January, your new coverage will take effect on February 1.
When is the Medicare election period?
Annual Election Period. From October 15 to December 7 each year is the Annual Election Period. This period is also referred to as the Annual Enrollment Period. During this time, you can elect to make changes to your Medicare coverage.
When is the Medicare Advantage open enrollment period?
The Medicare Advantage Open Enrollment Period, January 1 – March 31 every year, starting in 2019. The 5-Star Special Enrollment Period. You can switch to a Medicare Advantage plan with a 5-star rating between December 8 one year and November 30 the next year.
Does Medicare cover prescription drugs?
Here are just a few. Many – but not all – Medicare Advantage plans cover prescription drugs. Some Medicare Advantage plans give you extra benefits, like routine dental or hearing care. Some plans may require you to use doctors in the plan’s provider network, or pay more if you go outside the network. Premiums vary among plans.
How to switch to Medicare Advantage?
To switch to a new Medicare Advantage Plan, simply join the plan you choose during one of the enrollment periods. You'll be disenrolled automatically from your old plan when your new plan's coverage begins. To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE. Unless you have other drug coverage, you should ...
What happens if you lose Medicare coverage?
In other cases, you may still be able to use your employer or union coverage along with the Medicare Advantage plan you join.
When can I change my insurance plan in 2021?
Changing plans in 2021 — what you need to know. You can change plans through August 15 due to the coronavirus disease 2019 (COVID-19) emergency. If you’re currently enrolled in Marketplace coverage, you may qualify for more tax credits. Learn more about new, lower costs.
Can you add a new dependent to your current plan?
New household members. If your household size increases due to marriage, birth, adoption, foster care, or court order, you can choose to add the new dependent to your current plan or add them to their own group and enroll them in any plan for the remainder of the year.
Can a dependent pick a health insurance plan?
Enrollees and their dependents (including newly added household members) who qualify for the most common Special Enrollment Period types — like a loss of health insurance, moving to a new home, or a change in household size — will only be able to pick a plan from their current plan category .
Can you change your health insurance plan at any time?
If you have a life event that qualifies you for a Special Enrollment Period, you can change any time. Most people who qualify for a Special Enrollment Period and want to change plans may have a limited number of health plan “metal” categories to choose from (instead of all 4) during their Special Enrollment Period.
Can you enroll in a different plan with the same plan?
If your plan’s rules don’t allow you to add new members to your plan, your family can enroll together in a different plan in the same category. If no other plans are available in your current plan category, your family can enroll together in a category that’s one level up or one level down.
Does an employer offer to help with the cost of coverage?
An employer offer to help with the cost of coverage. Gaining access to an individual coverage HRA or a QSEHRA from your employer to help with coverage costs doesn’t limit your ability to choose a new plan during a Special Enrollment Period.
How long can you change your Medicare plan?
During these 7 months, you can make any changes you need to your plan elections, says Matt Dworetsky, founder of Dworetsky Financial in Manalapan, New Jersey. If you enroll during your Initial Enrollment Period, you can also make changes anytime in the first 3 months of your Medicare coverage. “After that, you can switch plans during open ...
How long does Medicare open enrollment last?
Medicare Advantage Open Enrollment lasts from January 1 through March 31 each year. If you qualify for a SEP, you generally have 2 months to make a change to your Medicare Advantage Plan. There are 3,550 Medicare Advantage Plans available nationwide in 2021, according to the Kaiser Family Foundation. The average Medicare beneficiary has access ...
How long do you have to switch insurance plans after moving?
You have from one month before your move until 2 months after your move to switch plans.
How long does Medicare Advantage last?
Your first opportunity is after you first enroll in a MA Plan during your Initial Enrollment Period. Your Initial Enrollment Period generally lasts for 7 months from 3 months before the month you turn 65 to 3 months after the month you turn 65, ...
Can I sell my Medicare Part A?
No. The prohibition, set forth in Section 1882(d) of the Social Security Act, applies to selling or issuing coverage to someone who has Medicare Part A or Part B . However, the regulations at 26 CFR §1.36B-2(c)(i) state that an individual who is eligible to receive benefits under government-sponsored minimum essential coverage (e.g. Medicare Part
Can you sell QHP to Medicare?
Yes. The prohibition on selling or issuing duplicative coverage set forth in Section 1882(d) of the Social Security Act applies to the sale or issuance of a (QHP) or other individual market coverage to a Medicare beneficiary. It does not require an individual who was not a Medicare beneficiary when the QHP was purchased to drop coverage when he or she becomes a Medicare beneficiary.
Does Medicare cover a person with employer health insurance?
Medicare beneficiaries whose employer purchases SHOP coverage are treated the same as any other person with employer coverage. If the employer has 20 or more employees, the employer-provided health coverage generally will be primary for a Medicare beneficiary who is covered through active employment.
Is Medicare Part B considered essential?
If you have only Medicare Part B, you are not considered to have minimum essential coverage. This means you may have to pay the penalty that people who don't have coverage may have to pay. If you have Medicare Part A only, you are considered covered. If you have both Medicare Part A and Part B, you are also considered covered.
Can you sell Medicare coverage to a beneficiary?
Consistent with the longstanding prohibitions on the sale and issuance of duplicate coverage to Medicare beneficiaries (section 1882(d) of the Social Security Act), it is illegal to knowingly sell or issue an Individual Marketplace Qualified Health Plan (or an individual market policy outside the Marketplace) to a Medicare beneficiary. The issuer should cancel an enrollment prior to the policy being issued if the issuer learns that the enrollment is for someone who has Medicare coverage. That is, the start date for the individual’s Part A and/or Part B was before the effective date of the individual market coverage. However, if the applicant’s Medicare coverage has not started yet, then the issuer issue the coverage on a guaranteed available basis.
Can a dialysis facility apply for Medicare?
dialysis facility or attending physician may not complete an application for Medicare entitlement on behalf of the beneficiary. While these providers may submit the medical evidence form for an individual applying for Medicare based on ESRD, the individual must also contact the Social Security Administration (SSA) to complete the Medicare application.
Can I withdraw from Medicare after kidney transplant?
Generally, no. Following the application for Medicare, the law provides that Medicare coverage ends one year after the termination of regular dialysis or 36 months after a successful kidney transplant. However, a beneficiary may withdraw their original Medicare application. The individual is required to repay all costs covered by Medicare, pay any outstanding balances, and refund any benefits received from the SSA or RRB. Once all repayments have been made, the withdrawal can be processed as though the individual was never enrolled in Medicare at all (i.e., retroactively).
