- Make changes during general open enrollment (October 15 to December 7, with changes effective January 1).
- Switch to Original Medicare during the first year on the Medicare Advantage plan (trial period).
- Switch to Original Medicare during the annual Medicare Advantage open enrollment period (January 1 to March 31). ...
How to switch back to traditional Medicare?
in other exceptional circumstances. In most cases, all you need do to switch to traditional Medicare is disenroll from your health plan, which will check that you are entitled to a SEP. Once your plan coverage ends, traditional Medicare coverage automatically kicks in.
Does Medicare Advantage replace original Medicare?
Pitfalls of Medicare Advantage Plans
- Coverage Choices for Medicare. If you're older than 65 (or turning 65 in the next three months) and not already getting benefits from Social Security, you have to sign up ...
- Original Medicare. ...
- Medicare Advantage Plans. ...
- Disadvantages of Medicare Advantage Plans. ...
- Consider Premiums—and Your Other Costs. ...
- Switching Back to Original Medicare. ...
- The Bottom Line. ...
Can I go back to Original Medicare?
You can leave your Medicare Advantage plan to return to Original Medicare during two times each year: During Open Enrollment Period (Oct. 15 – Dec. 7) During the Medicare Advantage Disenrollment Period (Jan. 1 – Feb. 14) Browse Plans Online >>
When can I make changes to my Medicare coverage?
There are two opportunities outside of the Medicare Annual Enrollment Period when you may be able to make changes to your Medicare coverage: 1) the Medicare Advantage Open Enrollment Period and 2) the Special Enrollment Period for qualifying life events. The Medicare Advantage Open Enrollment Period runs from January 1 to March 31 each year.
How do I switch back to Original Medicare?
How to switchTo switch to a new Medicare Advantage Plan, simply join the plan you choose during one of the enrollment periods. You'll be disenrolled automatically from your old plan when your new plan's coverage begins.To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE.
Can you switch from Medicare Advantage to Original Medicare at any time?
You have many options to change coverage during this annual open enrollment period. You can switch to a different Medicare Advantage plan, change from a Medicare Advantage plan to original Medicare and vice versa, or switch from one Part D drug plan to another. Coverage in the new plan begins Jan. 1.
When can I change my original Medicare plan?
Fall Open Enrollment Period: You can make a number of changes to your Medicare coverage during Fall Open Enrollment (also known as the Annual Coordinated Election Period – ACEP). The Fall Open Enrollment Period occurs each year from October 15 through December 7, with your new coverage starting January 1.
Does getting a Medicare Advantage Plan make you lose original Medicare?
If you join a Medicare Advantage Plan, you'll still have Medicare but you'll get most of your Part A and Part B coverage from your Medicare Advantage Plan, not Original Medicare. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What happens when I disenroll from a Medicare Advantage plan?
Automatic disenrollment Disenrollment from the old plan will be automatic when the new policy begins, so there will be no break in coverage. People with a Medicare Advantage plan may also switch back to original Medicare. To do so, they may contact their plan provider to let them know or call Medicare directly.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Can I change Medicare plans during the year?
To switch to a new Medicare Advantage Plan, simply join the plan you choose during one of the enrollment periods. You'll be disenrolled automatically from your old plan when your new plan's coverage begins. To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE.
What are the top 3 Medicare Advantage plans?
The Best Medicare Advantage Provider by State Local plans can be high-quality and reasonably priced. Blue Cross Blue Shield, Humana and United Healthcare earn the highest rankings among the national carriers in many states.
Can I change my Medicare Supplement plan at any time?
As a Medicare beneficiary, you can change supplements at any time. As a result, there's no guarantee an application will be accepted if switched outside the designated Open Enrollment Period. An application may be “medically underwritten”.
Which two Medicare plans Cannot be enrolled together?
You generally cannot enroll in both a Medicare Advantage plan and a Medigap plan at the same time.
Can you switch back and forth between Medicare Advantage and Medigap?
Can I switch from Medicare Advantage to Medigap? A person can switch from Medicare Advantage to Medicare with a Medigap policy. However, the Centers for Medicare and Medicaid Services designate certain periods to do so. That said, some people can also switch at certain other times without incurring a penalty.
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.
Can I change Medicare Supplement plans anytime?
As a Medicare beneficiary, you can change supplements at any time. As a result, there's no guarantee an application will be accepted if switched outside the designated Open Enrollment Period. An application may be “medically underwritten”.
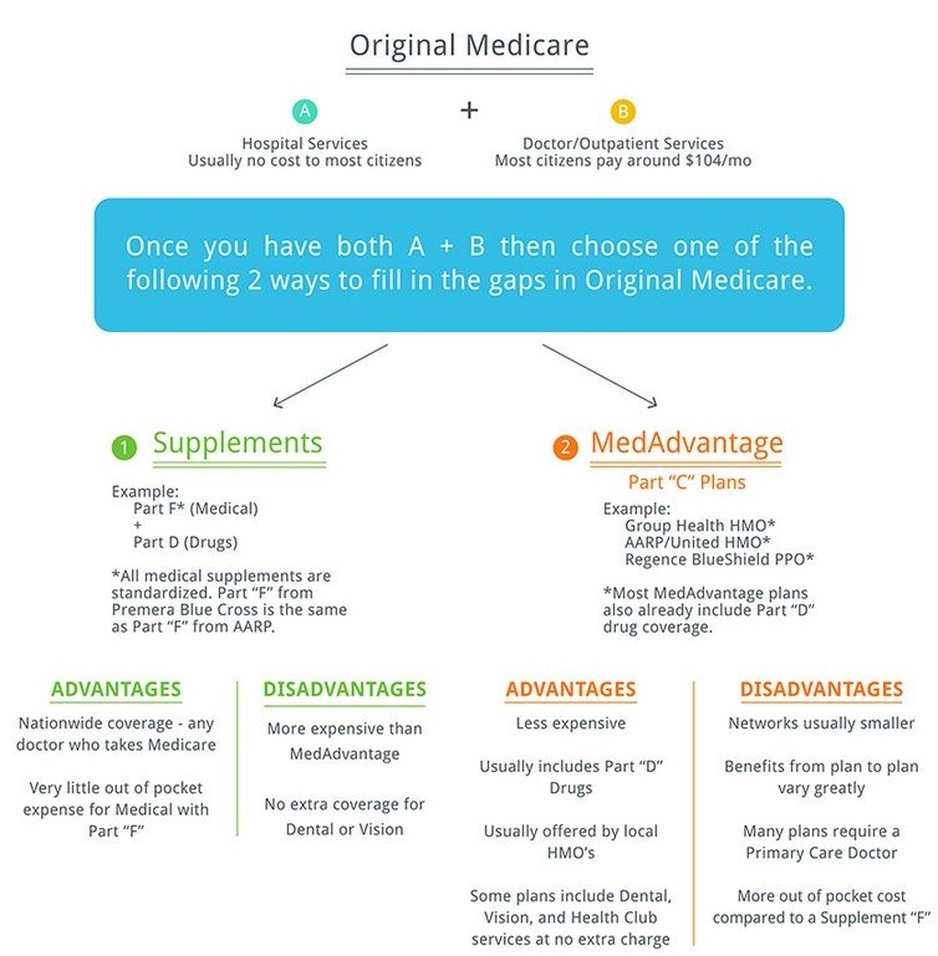
What is the difference between Original Medicare and Medicare Advantage?
Original Medicare covers inpatient hospital and skilled nursing services – Part A - and doctor visits, outpatient services and some preventative care – Part B. Medicare Advantage plans cover all the above (Part A and Part B), and most plans also cover prescription drugs (Part D).
What is the difference between Medicare Supplement and Medicare Advantage plans?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
What is the difference between Medicare Advantage and Medigap?
Medigap is supplemental and helps to fill gaps by paying out-of-pocket costs associated with Original Medicare while Medicare Advantage plans stand in place of Original Medicare and generally provide additional coverage.
When does a disenrollment become effective?
When you request to disenroll from your plan, your disenrollment likely won’t be effective immediately. In fact, it should become effective the first month after you request to disenroll from the plan. If you request to disenroll on February 1, you will officially leave your plan on March 1. Make sure you know exactly when you will be officially ...
How to join a Part D insurance plan?
You may be able to do this by doing any of the following: Joining online on the plan’s website. Requesting a paper enrollment form from the plan, filling it out and returning it. Calling the plan.
Can you switch from Advantage to Original?
The AEP and MAOEP may not be the only periods of time in which you can switch from Advantage to Original. You may have a Special Enrollment Period, or a special circumstance, which allows you to drop your MA plan at other times during the year. For example, you may be able to leave it and return to Original Medicare if you joined Advantage for the first time within the past 12 months after dropping your Medigap plan.
What to Know About the Annual Enrollment Period
Because your only opportunity to change from Medicare Advantage back to Original Medicare takes place during the AEP, you should know a bit more about it to better inform your switch. Prior to the AEP, you will receive an Annual Notice of Change (ANOC) and/or Evidence of Coverage (EOC).
What Is Medicare Advantage and How Does it Work?
Chances are, if you are already enrolled in an Advantage plan, you are already pretty familiar with it. However, before making the switch back to Original Medicare, you should know a few things about how it works.
Ready to Make Changes to Your Medicare Plan?
Our business is with people just like you—we help people get the Medicare coverage they need with free, high-quality, no-strings-attached insurance help. If you want to speak with one of our team members, call Trusted Senior Specialists today at (855) 952-1941.
How many months do you have to sign up for Medicare?
If you sign up for Medicare during the general enrollment period, you have three additional months (April – June) during which you can select a Part D plan or a Medicare Advantage plan.
When will Medicare open enrollment end?
A: For 2021 coverage, open enrollment (also known as the annual election period) for Medicare Advantage and Medicare Part D ended on December 7, 2020.
How many Medicare Advantage plans will be available in 2021?
For 2021, there are a total of 28 plans that have a five-star rating. Most are Medicare Advantage plans, but the list includes two stand-alone Part D plans and two Medicare cost plans.
When is the special enrollment period for Medicare?
The federal government allows a special enrollment period, after the end of the general enrollment period, for people who live in (or rely on enrollment help from someone who lives in) an area that’s experienced a FEMA-declared major disaster or emergency. For 2021 coverage, there are several states and several partial states where this special enrollment period is available. Eligible enrollees who make a Medicare Advantage or Part D plan selection during this special enrollment period will have coverage effective January 1, 2021.
When will Medicare Advantage coverage start in 2021?
Eligible enrollees who make a Medicare Advantage or Part D plan selection during this special enrollment period will have coverage effective January 1, 2021.
When is Medicare Part B coverage guaranteed?
If you’re within the six-month open enrollment window that begins as soon as you’re at least 65 and enrolled in Medicare Part B, the coverage is guaranteed issue. That is also the case if you’re in a special enrollment period triggered by a qualifying event.
Does Medicare Advantage last longer than the disenrollment period?
As of 2019, this window replaced the Medicare Advantage Disenrollment Period that was available in prior years. It lasts twice as long and provides more flexibility than the disenrollment period did, as it also allows Medicare Advantage enrollees the option to switch to a different Medicare Advantage plan.
You have multiple options if you want to leave an Advantage plan and return to Original Medicare
Medicare provides health insurance to American seniors as well as adults who have a qualifying disability or medical condition. Beneficiaries can choose between Original Medicare and a Medicare Advantage (MA) plan. But can you go back to Original Medicare from an Advantage plan? The short answer is, Yes.
What Is Original Medicare?
Medicare Part A is also known as hospital insurance. It covers inpatient care received in a hospital or skilled nursing facility. It also helps pay for hospice care.
What Is Medicare Advantage?
Medicare Part C, more commonly known as Medicare Advantage, is similar to the group health insurance plans that many people have through an employer. At a minimum, every Medicare Advantage plan must provide the same coverage as Original Medicare. However, they are not limited to this coverage.
Can You Return to Original Medicare After Joining an Advantage Plan?
Yes, you may return to Original Medicare after you join an Advantage plan. But you may only do so during specific enrollment periods.
Can You Join a Medigap Plan After Leaving Medicare Advantage?
Medicare Supplement Insurance, more commonly known as Medigap, helps pay some of your out-of-pocket costs under Original Medicare. You cannot have both Medigap and a Medicare Advantage plan.
How to Choose Between Original Medicare and Medicare Advantage
There are pros and cons to both Original Medicare and Medicare Advantage. The right choice depends on your unique situation. Consider the following:
How to switch Medicare Part D?
The process for switching depends on your plan. Start by contacting your plan provider or 1-800-MEDICARE for specific information. Make sure that you’re getting the coverage you want before dropping your MA plan.
When to drop MA insurance?
If the plan isn’t working, it may be worth waiting until the open enrollment period – October 15 to December 7 – to find a new MA plan that better fits your needs.
Is Medicare Advantage for everyone?
Perhaps you signed up because you thought it was a great deal, only to realize later that you don’t need comprehensive benefits and prescription drug coverage. Medicare Advantage isn’t for everyone. If you need to drop your plan and move to original Medicare, here are some things to keep in mind.
Does Medicare Advantage cover nursing home care?
Advantage may also cover assisted living facilities and nursing home care, other benefits that original does not .
Is Medicare accepted for travel?
It also means that for those who travel, getting medical care can be less stressful since Medicare is widely accepted. And if you don’t need a lot of prescription drugs, there’s no point in paying for that coverage. Keep in mind, though, that original Medicare comes with some pretty big limitations.
Does Medicare Advantage come with a network?
Medicare Advantage comes with networks. It’s partly how these plans keep costs low. With original Medicare, you’re free to use any provider nationwide that accepts Medicare, which means that you can see a specialist when needed without having to get a referral or stay inside a network.
Does Medicare cover hospital care?
For starters, it covers basic medical and hospital care with Parts B and A, respectively, but it doesn’t cover much else. You’ll also have to cover about 20 percent of your medical bills all year without a cap.
When does Medicare kick in?
If you make a change during the Medicare Advantage Open Enrollment Period, your new Medicare benefits will kick in on the first day of the month following your enrollment. For example, if you make a change to your Medicare Advantage plan at any point during the month of January, your new coverage will take effect on February 1.
When does Medicare open enrollment end?
Any changes that you make will take effect on January 1 of the following year. Medicare Advantage Open Enrollment Period. This open enrollment period applies to recipients who are currently using a Medicare Advantage plan. This period lasts from January 1 to March 31 each year, and during this time, you can make one change to your healthcare ...
When is the Medicare election period?
Annual Election Period. From October 15 to December 7 each year is the Annual Election Period. This period is also referred to as the Annual Enrollment Period. During this time, you can elect to make changes to your Medicare coverage.
When does Medicare revert to original?
Once you contact your Medicare Advantage plan during Annual Enrollment to dis-enroll, your coverage will automatically revert to Original Medicare. You don’t have to contact Medicare yourself. Your new coverage will begin on January 1.
How to switch from Medicare Advantage to Original Medicare?
To switch from a Medicare Advantage plan to Original Medicare, you will need to contact your plan provider or Medicare directly. You can contact Medicare via the Medicare helpline 24 hours a day, seven days a week at 1-800-MEDICARE (1-800-633-4227), TTY 1-877-486-2048.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What is Medicare Advantage?
Most Medicare Advantage plans are all-in-one plans. They cover your Medicare Part A and Part B benefits plus prescription drugs (Part D) and other health services and items not included with Original Medicare. Examples of these other items include coverage for dental health, vision, hearing and gym memberships.
What happens if you drop your Medicare Advantage plan?
When you drop your Medicare Advantage plan, you will lose coverage for other health services and items such as for prescription drugs and vision or dental. You will also lose built-in financial protection on out-of-pocket costs.
When does Medicare start covering you?
You don’t have to contact Medicare yourself. Your new plan will begin covering you on January 1. If you have a stand-alone Part D prescription drug plan or other private Medicare plan, ...
Does Medicare have an annual out-of-pocket limit?
It does not provide some of the benefits you may have with your Medicare Advantage plan, like drug coverage, dental, vision or fitness. Original Medicare also doesn’t have an annual out-of-pocket limit, so there’s no built-in financial protection.
How to switch Medigap insurance?
How to switch Medigap policies. Call the new insurance company and arrange to apply for your new Medigap policy. If your application is accepted, call your current insurance company, and ask for your coverage to end. The insurance company can tell you how to submit a request to end your coverage.
What happens if you buy a Medigap policy before 2010?
If you bought your policy before 2010, it may offer coverage that isn't available in a newer policy. If you bought your policy before 1992, your policy: Might not be a Guaranteed renewable policy. May have a bigger Premium increase than newer, standardized Medigap policies currently being sold. expand.
How long do you have to have a Medigap policy?
If you've had your Medicare SELECT policy for more than 6 months, you won't have to answer any medical questions.
How long is the free look period for Medigap?
Medigap free-look period. You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period.". The 30- day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
Can you exclude pre-existing conditions from a new insurance policy?
The new insurance company can't exclude your Pre-existing condition. If you've had your Medigap policy less than 6 months: The number of months you've had your current Medigap policy must be subtracted from the time you must wait before your new Medigap policy covers your pre-existing condition.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
Can I keep my Medigap policy if I move out of state?
I'm moving out of state. You can keep your current Medigap policy no matter where you live as long as you still have Original Medicare. If you want to switch to a different Medigap policy, you'll have to check with your current or new insurance company to see if they'll offer you a different policy. If you decide to switch, you may have ...