What is the open enrollment period for Medicare Supplements?
six-monthUnder federal law, you have a six-month open enrollment period that begins the month you are 65 or older and enrolled in Medicare Part B. During your open enrollment period, Medigap companies must sell you a policy at the best available rate regardless of your health status, and they cannot deny you coverage.
How do I qualify for Medigap insurance?
Medicare Supplement Eligibility for Beneficiaries Aging in at 65Enroll in Medicare Part A and Medicare Part B.Be a citizen or legal resident of the United States for at least five years.Reside in the state offering the Medicare Supplement plan at time of application.More items...•Feb 25, 2022
Are Medigap premiums based on age?
Generally the same monthly premium is charged to everyone who has the Medigap policy, regardless of age. Your premium isn't based on your age. Premiums may go up because of inflation and other factors, but not because of your age.
Can I switch from Medicare Advantage to Medigap without underwriting?
For example, when you get a Medicare Advantage plan as soon as you're eligible for Medicare, and you're still within the first 12 months of having it, you can switch to Medigap without underwriting. The opportunity to change is the "trial right."Jun 3, 2020
Can I change Medicare supplement plans anytime?
You can change your Medicare Supplement Plan anytime, just be aware that you might have to answer medical questions if your outside your Open Enrollment Period.
Does Medigap cover pre-existing conditions?
Coverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded.
Can Medigap premiums increase mid year?
Medigap premium increases will occur nearly every year. Any agent who tells you otherwise is untrustworthy. Most Medigap policies have a rate increase once a year, usually on your policy anniversary. Some carriers increase on your birthday month instead.Dec 31, 2021
Do Medigap premiums go up each year?
Some insurance plans will have increases simply because you're getting older. Medicare Supplement Insurance (Medigap) companies try to limit premium increases to once a year, says Bill Gay, a licensed Medicare insurance agent and owner of Sun Coast Legacy Advisors.Sep 14, 2021
What is the average cost of a Medigap plan?
The average cost of a Medicare supplemental insurance plan, or Medigap, is about $150 a month, according to industry experts. These supplemental insurance plans help fill gaps in Original Medicare (Part A and Part B) coverage.Mar 21, 2022
What is the downside to Medigap plans?
Some disadvantages of Medigap plans include: Higher monthly premiums. Having to navigate the different types of plans. No prescription coverage (which you can purchase through Plan D)
Does Medigap have an out of pocket maximum?
Do Medigap Plans have an Out-of-Pocket Maximum? Medigap plans don't have a maximum out-of-pocket because they don't need one. The coverage is so good you'll never spend $5,000 a year on medical bills.Sep 22, 2021
Are you automatically disenrolled from Medicare Advantage to Medigap?
To switch to a new Medicare Advantage Plan, simply join the plan you choose during one of the enrollment periods. You'll be disenrolled automatically from your old plan when your new plan's coverage begins. To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE.
How Medicare works with other insurance
Learn how benefits are coordinated when you have Medicare and other health insurance.
Retiree insurance
Read 5 things you need to know about how retiree insurance works with Medicare. If you're retired, have Medicare and have group health plan coverage from a former employer, generally Medicare pays first. Your retiree coverage pays second.
What's Medicare Supplement Insurance (Medigap)?
Read about Medigap (Medicare Supplement Insurance), which helps pay some of the health care costs that Original Medicare doesn't cover.
When can I buy Medigap?
Get the facts about the specific times when you can sign up for a Medigap policy.
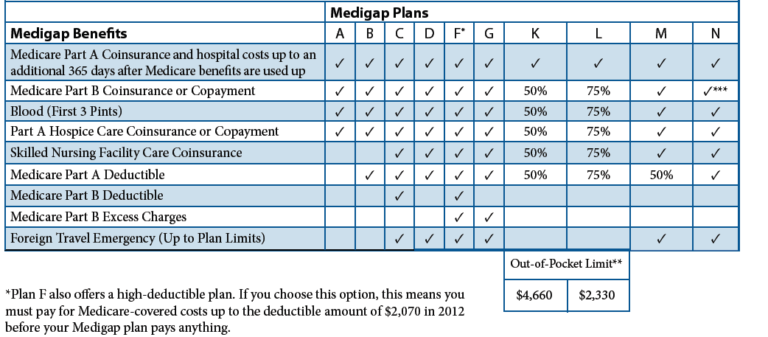
How to compare Medigap policies
Read about different types of Medigap policies, what they cover, and which insurance companies sell Medigap policies in your area.
Medigap & travel
Read about which Medigap policies offer coverage when you travel outside the United States (U.S.).
How long does it take to apply for Medicare Supplement?
When to apply for a Medicare Supplement plan. Here's the quick answer: Most people should apply for a Medigap plan within six months of signing up for Part B. Medigap open enrollment begins when you sign up for Medicare Part B (at age 65) and lasts for six months. If you defer Part B coverage past age 65 because of health coverage ...
Does Medicare cover medical expenses?
December 12, 2019. Medicare can cover a wide range of medical costs, but like anything else, it’s not perfect. We would all like a bit more coverage than Original Medicare can offer, especially when we know we'll be in more need of the benefits later in life. Luckily, Medicare Supplement (also called Medigap) plans provide a solution, ...
Is eligibility.com a Medicare provider?
Eligibility.com is a DBA of Clear Link Technologies, LLC and is not affiliated with any Medicare System Providers.
Do I need to have Original Medicare to apply for Medigap?
The short answer is yes. To have a Medigap policy, you must first have Medicare Part A and Part B. Your Medigap Open Enrollment Period begins on the first day of the month that you’re both 65 or older and enrolled in Medicare Part B.
Can I have a Medicare Supplement insurance plan with Medicare Advantage?
If you have a Medicare Advantage plan but are planning to drop it and sign up for Original Medicare, you can apply for a Medigap policy before your Medicare Advantage coverage ends. The insurer can sell you a Medigap policy if you verify that you are leaving the Medicare Advantage plan and will sign up for Medicare Part A and B.
What types of Medicare Supplement insurance plans are available?
Different Medigap policies may be available to you depending on your state. Insurance companies that sell Medigap don’t have to sell every plan. However, the insurance company must offer Medigap Plan A (which is not the same as Medicare Part A) if it offers any Medigap policy.
How long does Medicare Supplement open enrollment last?
How can enrollment periods affect my eligibility for Medicare Supplement plans? The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period —for most people, this period starts the month that you turn 65 and have Medicare Part B, and goes for six months.
Does Medicare Supplement cover out-of-pocket expenses?
Medicare Supplement plans aren’t meant to provide stand-alone health coverage; these plans just help with certain out-of-pocket costs that Original Medicare doesn’t cover. If you’re under 65 and have Medicare because of disability, end-stage renal disease, or amyotrophic lateral sclerosis, your eligibility for Medicare Supplement coverage may ...
How long do you have to wait to get Medicare Supplement?
Keep in mind that even though a Medicare Supplement insurance company cannot reject your enrollment for health reasons, the company is allowed to make you wait up to six months before covering your pre-existing conditions.
Does Medigap cover prescriptions?
Since Medigap plans don’t include prescription drug benefits, if you’re enrolled in Original Medicare and want help with prescription drug costs, you can get this coverage by enrolling in a stand-alone Medicare Prescription Drug Plan.
Does Medigap cover coinsurance?
Medigap plans cover some of your out of pocket expenses like copayments, coinsurances, and some deductibles not included in Original Medicare benefits. There are currently several types of Medigap policies available to purchase in most states.
What happens if you cancel your insurance?
When you terminate your policy, in most cases it continues through the month that you have already paid. Some insurance companies offer a refund of unused funds if applicable.