When can you join a Medicare Advantage plan?
Your first opportunity is during your initial enrollment period when you first become eligible for Medicare. After that, you can only join a Medicare Advantage Plan during the Medicare Open Enrollment Period from October 15 to December 7 each year.
How to join a Medicare Advantage plan?
When can I enroll in a Part C plan?
- Initial Enrollment Period (IEP)
- Annual Enrollment Period (AEP)
- Special Enrollment Period (SEP)
When is it too late to enroll in Medicare?
You may owe a late enrollment penalty if at any time after your Initial Enrollment Period is over, there's a period of 63 or more days in a row when you don't have Medicare drug coverage or other
When is the Medicare Advantage enrollment period?
The Medicare Advantage Open Enrollment Period starts January 1 and ends March 31 every year. During this period, you can switch Medicare Advantage plans or leave a Medicare Advantage plan and return to Original Medicare. Depending on your circumstances, you may also qualify for a Special Enrollment Period (SEP).

Can you add Medicare Advantage plans at any time?
If you're covered by both Medicare and Medicaid, you can switch plans at any time during the year. This applies to Medicare Advantage as well as Medicare Part D.
Can I switch to Medicare Advantage at any time?
You can make changes to your plan at any time during the Medicare Advantage open enrollment period from January 1 through March 31 every year. This is also the Medicare general enrollment period. The changes you make will take effect on the first day of the month following the month you make a change.
What is the Medicare Advantage initial enrollment period?
Initial Enrollment Period (IEP): Seven-month period, including the three months before, the month of, and the three months after the month you first become eligible for Medicare (either your 65th birth month or the 25th month you have collected disability benefits).
Can you enroll in Medicare Advantage with pre existing conditions?
Medicare defines a pre-existing condition as any health problem that you had prior to the coverage start date for a new insurance plan. If you have Original Medicare or a Medicare Advantage plan, you are generally covered for all Medicare benefits even if you have a pre-existing condition.
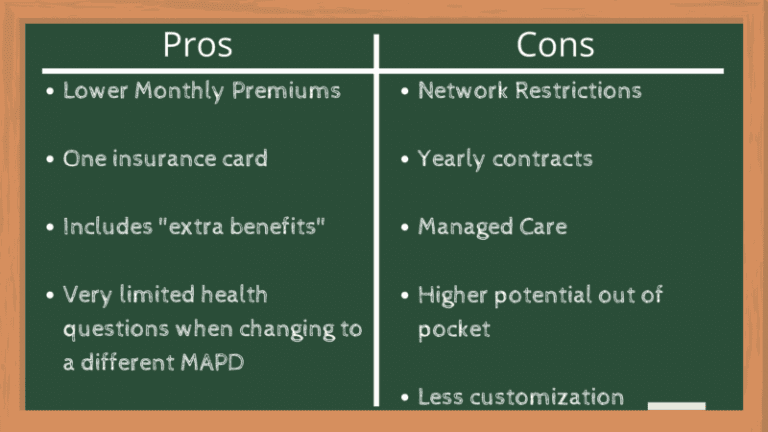
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Can I switch from Original Medicare to a Medicare Advantage plan?
You can switch from original Medicare to Medicare Advantage during one of the Medicare open enrollment periods. Medicare Advantage plans offer a popular substitute for Original Medicare (Parts A and B).
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.
What is initial enrollment period?
Initial Enrollment Period – a 7-month period when someone is first eligible for Medicare. For those eligible due to age, this period begins 3 months before they turn 65, includes the month they turn 65, and ends 3 months after they turn 65.
Do you need Medicare Part B if you have a Medicare Advantage plan?
Many Medicare Advantage plans offer extra benefits not available from Original Medicare. Therefore, to enroll in a Medicare Advantage plan, you must be enrolled in both Medicare Part A and Part B.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Can Medicare Advantage plans deny for pre-existing conditions?
As with Original Medicare, Medicare Advantage plans can't charge you more for preexisting conditions. Because they are offered by private insurance companies, basic costs for Medicare Advantage plans will vary by plan. In addition, you can't be denied coverage based on preexisting conditions.
What's considered a pre-existing condition?
As defined most simply, a pre-existing condition is any health condition that a person has prior to enrolling in health coverage. A pre-existing condition could be known to the person – for example, if she knows she is pregnant already.
How long does it take to enroll in Medicare Advantage?
Enrolling in a Medicare Advantage plan during your Initial Enrollment Period. When you first become eligible for Medicare, you have a 7-month Initial Enrollment Period (IEP) to enroll in Medicare. Then once enrolled in Part A and Part B, you can sign up for a Medicare Advantage plan (also known as Medicare Part C).
When is Medicare open enrollment?
The Medicare Open Enrollment Period, also known as the Annual Election Period (AEP), runs yearly from October 15 to December 7 , during which Medicare beneficiaries can apply for Medicare Advantage plan coverage.
How to change Medicare Advantage plan?
The Medicare Open Enrollment Period, also known as the Annual Election Period (AEP), runs yearly from October 15 to December 7, during which Medicare beneficiaries can apply for Medicare Advantage plan coverage. Beneficiaries can make the following changes to their coverage during this two-month period: 1 Switch from Original Medicare to Medicare Advantage 2 Switch from a Medicare Advantage plan back to Original Medicare 3 Switch from a Medicare Advantage plan to a different Medicare Advantage plan in their service area 4 Switch from a Medicare Advantage plan that doesn’t include drug coverage to one that does, and vice versa
What is Medicare Advantage?
Medicare Advantage plans are provided through private insurance companies and offer the same benefits as Original Medicare, with some also offering prescription drug coverage and vision, dental or hearing care.
What happens if you miss the enrollment period?
If you missed the other enrollment periods, you generally have to wait for the next Annual Election Period. However, there are certain special circumstances that could qualify you for a Special Enrollment Period, such as: You moved out of your current Medicare Advantage plan’s service area. You are eligible for Medicaid.
When does IEP end?
If you are aging into Medicare, then your IEP begins 3 months before the month that you turn 65 and ends 3 months after the month you turn 65. For example, if you age into Medicare in May, then your Initial Enrollment Period begins February 1st and ends August 31st. People with End-Stage Renal Disease generally cannot enroll in a Medicare Advantage ...
How long does it take to get Medicare Advantage?
This is the period that begins three months before your birth month and ends three months after it. While there is no cost penalty for signing up at any time during this period, it is highly desirable to sign up as early in the period as possible. This is because any plan with a Part D component takes approximately three months to kick in, which means you could see a temporary gap in your drug coverage if you sign up any time after your birthday. This gap could last as long as three months after the time you lose the coverage you had before switching to Medicare, so it’s helpful to start your research before the ICEP and get the forms submitted prior to the first day of the month you turn 65.
What is Medicare Part A?
Medicare Part A is the basic coverage Medicare provides for its beneficiaries. This is a no-cost plan that covers the cost of inpatient hospitalization for eligible seniors. All U.S. citizens are automatically enrolled in Part A when they become eligible, since there is no out-of-pocket cost or monthly premium for this coverage. Services covered under Part A generally revolve around admissions to the hospital and treatments provided as part of regular inpatient care. Providers bill the Original Medicare program directly, which then pays for services according to a fixed or negotiated schedule. All Medicare-qualified providers are part of the Part A network, and they are required to bill only Medicare for covered services, unless the patient has a Medicare Advantage plan that provides the same coverage.
Is Medicare Supplement Part C?
Medicare supplements are not strictly part of the Medicare system, but they are a consequence of it. Whether you have Original Medicare or Medicare Advantage, there could easily be some gaps in coverage that leave certain services out. Many seniors also face high copayments and extra out-of-pocket expenses for services not covered by their Part C plan. Medicare supplement plans plug these gaps with various coverage options. These are highly variable, and each plan has to be discussed with an insurance agent to make sure the coverage is adequate for your situation.
Can you enroll in Medicare Advantage outside of the normal enrollment period?
Sometimes circumstances force beneficiaries to enroll in Medicare Advantage outside of the normal enrollment periods. This can be tricky to do without incurring a penalty rate, but there are special circumstances you can invoke to justify an out-of-period enrollment. Examples of special circumstances include:
Enrolling in a Medicare Advantage Plan
Medicare requires that you enroll, disenroll, or make changes to your Medicare Advantage plan only during pre-determined enrollment periods.
Learn More About Medicare
Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage.
When is the Medicare Advantage enrollment period?
There are now three main Medicare Advantage enrollment periods, although what you can do during each period may be slightly different.
Medicare Advantage enrollment: what if I have a pre-existing condition?
In most cases, you can switch from Original Medicare to a Medicare Advantage plan regardless of health status or pre-existing conditions. If you have end-stage renal disease, you may not be eligible for most Medicare Advantage plans. You may be able to sign up for a special type of Medicare Advantage plan called a Special Needs Plan.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
How many enrollment periods are there for Medicare Advantage?
There are 2 separate enrollment periods each year. See the chart below for specific dates.
What is the late enrollment penalty for Medicare?
The late enrollment penalty is an amount that’s permanently added to your Medicare drug coverage (Part D) premium. You may owe a late enrollment penalty if at any time after your Initial Enrollment Period is over, there’s a period of 63 or more days in a row when you don’t have Medicare drug coverage or other creditable prescription drug coverage. Creditable prescription drug coverage is coverage (for example, from an employer or union) that’s expected to pay, on average, at least as much as Medicare’s standard prescription drug coverage. If you have a penalty, you’ll generally have to pay it for as long as you have Medicare drug coverage. For more information about the late enrollment penalty, visit Medicare.gov, or call 1‑800‑MEDICARE (1‑800‑633‑4227). TTY users can call 1‑877‑486‑2048.
What are the special enrollment periods?
When certain events happen in your life, like if you move or lose other insurance coverage, you may be able to make changes to your Medicare health and drug coverage. These chances to make changes are called Special Enrollment Periods. Rules about when you can make changes and the type of changes you can make are different for each Special Enrollment Period.