What is the Medicare Secondary Payer Act (MSP)?
The Medicare Secondary Payer (MSP) provisions protect the Medicare Trust Fund from making ... National program savings: CMS MSP provisions enforcement saved the Medicare Program about $8.5 billion in FY 2018. Increased provider, physician, and other supplier revenue: Billing a primary plan before ... Social Security Act §1862. Title 42 The ...
When can Medicare make payment to a secondary payer?
The Medicare Secondary Payer Act (the “MSP Act”) was first enacted in 1980; however, it is the recent Section 111 reporting requirements (that become effective January 1, 2011 for settlements entered into on or after October 1, 2010) that have brought that statute to the forefront of personal injury and insurance defense litigation.
When did Medicare become the primary payer for claims?
B. The Medicare Secondary Payer Act (“MSP”) In 1980, Congress amended the Social Security Act to include the MSP, which became effective on December 5, 1980. 42 U.S.C. § 1395y(b)(2) (Regulations are promulgated under 42 C.F.R. 411.20, et seq). The MSP sets forth Medicare’s status as a secondary, rather than primary
Does the Medicare Secondary Payer Act apply to claims adjusters?

Under which circumstance is Medicare the secondary payer?
Medicare may be the secondary payer when: a person has a GHP through their own or a spouse's employment, and the employer has more than 20 employees. a person is disabled and covered by a GHP through an employer with more than 100 employees.Oct 29, 2020
What is the purpose of Medicare Secondary Payer MSP )?
The Medicare Secondary Payer (MSP) provisions protect the Medicare Trust Fund from making payments when another entity has the responsibility of paying first. Any entity providing items and services to Medicare patients must determine if Medicare is the primary payer.
Is Medicare administered by CMS?
The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, and the Children's Health Insurance Program (CHIP).
Is MSP required for Medicare Advantage plans?
The Medicare Advantage program was created under Part C of the Medicare statutes to serve as an alternative delivery vehicle for Medicare benefits, but as far as the MSP regulations and CMS are concerned, Medicare Advantage plans have the same rights and responsibilities for MSP enforcement as traditional Medicare ...Aug 28, 2019
What happens when Medicare is secondary?
The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the remaining costs. If your group health plan or retiree coverage is the secondary payer, you may need to enroll in Medicare Part B before they'll pay.
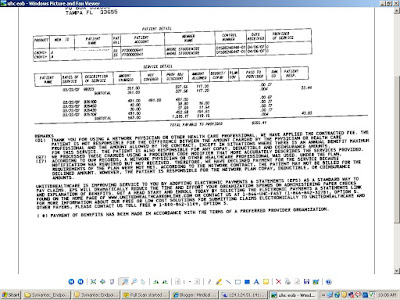
How do you fill out CMS 1500 when Medicare is secondary?
0:239:21Medicare Secondary Payer (MSP) CMS-1500 Submission - YouTubeYouTubeStart of suggested clipEnd of suggested clipEither through the patients or the spouse's employment or any other source the biller lists the nameMoreEither through the patients or the spouse's employment or any other source the biller lists the name of the insured. Here when the insured. And the patient are the same the biller enters the word.
What is the role of the CMS?
The CMS oversees programs including Medicare, Medicaid, the Children's Health Insurance Program (CHIP), and the state and federal health insurance marketplaces. CMS collects and analyzes data, produces research reports, and works to eliminate instances of fraud and abuse within the healthcare system.
What does CMS do for Medicare?
The Centers for Medicare and Medicaid Services (CMS) provides health coverage to more than 100 million people through Medicare, Medicaid, the Children's Health Insurance Program, and the Health Insurance Marketplace.
Is CMS and Medicare the same thing?
The Centers for Medicare and Medicaid Services (CMS) is a part of Health and Human Services (HHS) and is not the same as Medicare. Medicare is a federally run government health insurance program, which is administered by CMS.
Can Medicare Advantage be a secondary payer?
Medicare Supplement plans are secondary payers to Medicare. Medicare will be billed first, then your supplement plan will be billed second.
How do you know if Medicare is primary or secondary?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
How often must MSP be completed?
once every 90 daysFollowing the initial collection, the MSP information should be verified once every 90 days.