If a doctor won’t accept a Medicare Supplement Plan, it is most likely due to the person mistakingly referring to their Medicare Advantage plan as a Medicare Supplement plan, according to Medicare.org. Medicare Advantage Plans have their own networks and are usually PPOs or HMOs. These networks change annually, sometimes in the middle of the year.
Full Answer
What happens if you don’t use a Medicare select Doctor?
If you don’t use a Medicare SELECT doctor or hospital, you might be responsible for paying some or all of what Medicare doesn’t pay. Why Won’t a Doctor Accept a Medicare Supplement Plan?
Do all doctors accept Medicare supplement (Medigap) plans?
Not all doctors accept Medicare supplement (Medigap) plans. However, if a doctor accepts Medicare (your primary coverage), they will accept your Medigap plan, regardless of the type of Medigap plan you’re enrolled in. If you aren’t familiar with what a Medicare supplement plan is,...
Is Medicare supplement plan F still available for new Medicare beneficiaries?
However, Medicare Supplement Plan F is no longer available for new Medicare beneficiaries. As a result, Plan G is quickly becoming the next most popular Medigap plan. Let's explore the differences between Plan F vs. Plan G.
What is the difference between Plan F and Plan G?
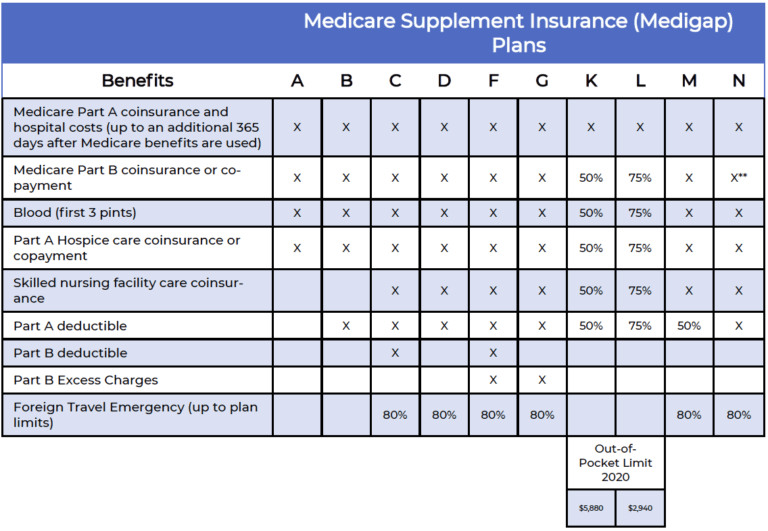
Plan F and Plan G both offer coverage for most of the nine Medicare costs that can be covered by a Medicare Supplement Insurance plan. The main difference is that Plan F covers the Medicare Part B deductible, and Plan G does not. Plan F and Plan G both offer 100 percent coverage for the following 2019 Medicare costs:

Why is Medigap plan F not available?
Medicare Supplement Plan F is being phased out as a result of “The Medicare Access and CHIP Reauthorization Act of 2015”, also known as MACRA. As a result of MACRA, anybody who becomes eligible for Medicare in 2020 will not be able to purchase Plan F.
Is Medicare getting rid of plan F?
Is Medicare Plan F Being Discontinued? No, Medicare Plan F is not being discontinued, but it is no longer an option for those who are new to Medicare. The 2015 Medicare Access and CHIP Reauthorization Act (MACRA) prevented Medicare Supplement plans (F and C, specifically) from providing coverage for Part B deductibles.
Is Medicare Plan F being discontinued in 2020?
It's been big news this year that as of Jan. 1, 2020, Medigap plans C and F will be discontinued. This change came about as a part of the Medicare Access and CHIP Reauthorization legislation in 2015, which prohibits the sale of Medigap plans that cover Medicare's Part B deductible.
Can I change from Medicare Plan F to plan G?
Switching from Plan F to Plan G If you enrolled in Plan F before 2020, you can continue your plan or switch to another Medigap plan, such as Plan G, if you prefer. You may want to make the change to reduce the price of your health insurance.
Will plan F be grandfathered?
If you enrolled in Plan F before 2020, you will be “grandfathered” into the plan. This gives you the choice to keep the plan past 2020.
Is plan G better than plan F?
Ultimately, Plan G has the same benefits as the Plan F, except for coverage for the Part B deductible ($233 for 2022). Once you pay the Part B deductible, the coverage is the same for both plans.
Why are they getting rid of Plan F?
The reason Plan F (and Plan C) is going away is due to new legislation that no longer allows Medicare Supplement insurance plans to cover Medicare Part B deductibles. Since Plan F and Plan C pay this deductible, private insurance companies can no longer offer these plans to new Medicare enrollees.
When did plan f go away?
Your ZIP Code allows us to filter for Medicare plans in your area. Medicare Supplement Plan F is the most comprehensive of the standardized Medicare Supplement plans available in most states. These plans are being phased out, starting in 2021.
Can I go back to Plan F?
In order to keep your Plan F, you don't need to renew or re-enroll every year. As long as you pay your premiums on time, your coverage will continue. You can also switch to another carrier that offers Plan F in the future, if another company offers a better rate that you would like to apply for.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Can you switch from plan F to plan G in 2021?
Yes, you can. However, it usually still requires answering health questions on an application before they will approve the switch. There are a few companies in a few states that are allowing their members to switch from F to G without review, but most still require you to apply to switch.
What is the deductible for plan F in 2022?
$2,490Effective January 1, 2022, the annual deductible amount for these three plans is $2,490.
Why won't my doctor accept my Medicare Supplement?
Why Won’t a Doctor Accept a Medicare Supplement Plan? If a doctor won’t accept a Medicare Supplement Plan, it is most likely due to the person mistakingly referring to their Medicare Advantage plan as a Medicare Supplement plan, according to Medicare.org. Medicare Advantage Plans have their own networks and are usually PPOs or HMOs.
What is Medicare Select?
Insurance companies in some states offer what’s known as Medicare SELECT which is a type of Medigap plan that has its own network of doctors and hospitals. If you enroll in a SELECT plan, you might have some limits on which doctor you can choose. Typically, these networks are for non-emergency care.
What is Medicare Supplement Insurance?
Medicare supplement insurance covers the remaining costs you are responsible for after original Medicare pays its portion, such as Medicare deductibles, coinsurance costs, skilled nursing facility costs after Medicare runs out and hospital costs after the Medicare-covered days are over. In other words, you pay your Medicare supplement plan premium ...
What are the three Medicare Supplement Plans?
Three Medicare supplement plans – Plan F, Plan High-Deductible F, and Plan G – might completely cover these charges but if you have any other plan under Medicare supplement insurance, ...
Do doctors accept Medicare?
Be sure your doctor accepts Medicare when you make your appointment to avoid any denial of payment later on. Studies show that the vast majority of doctors do accept Medicare, though those taking on new patients has dwindled, which has made it more difficult to find a doctor once you are enrolled in Medicare.
Does Medicare cover coinsurance?
The doctor will not bill you more than your share of the cost, which is the copayment or coinsurance amount ( a percentage of the bill even after you’ve met your deductible) and deductible amount. That portion would then be covered by your Medicare supplement insurance policy, depending on which policy you chose.
What is Medicare Supplement Plan F?
Medicare Supplement Plan F provides coverage for two areas that Plan N does not: Medicare Part B deductible. Part B excess charges. Doctors who do not accept Medicare assignment reserve the right to charge up to 15 percent more than the Medicare-approved amount for services and items they provide.
What percent of private insurance companies sell Plan F?
85 percent of private insurance companies sell Plan F, and 66 percent sell Plan G policies. While new Plan F policies are no longer sold to new Medicare beneficiaries, existing policies still provide ongoing coverage in many states. Residents in most states can purchase and use Plan G policies, though Massachusetts, Minnesota, ...
What is the deductible for Medicare 2021?
1 Plans F and G offer high-deductible plans that each have an annual deductible of $2,370 in 2021. Once the annual deductible is met, the plan pays 100% of covered services for the rest of the year. The high-deductible Plan F is not available to new beneficiaries who became eligible for Medicare on or after January 1, 2020.
What percentage of Medicare beneficiaries are enrolled in a Medigap plan?
Close to 34 percent of all Medicare beneficiaries are enrolled in a Medicare supplement insurance (Medigap) plan. These optional plans, issued by private insurance companies, help pay for some of the out-of-pocket costs that Original Medicare (Part A and Part B) doesn’t cover. Plan F has long been the most popular Medigap plan.
Is Medigap Plan F deductible?
While the deductibles mean you must pay a certain amount of money out of pocket before the plan coverage kicks in, the monthly premiums are typically much lower than the premiums for other Medigap plans or for the standard non-deductible versions of Plan F and Plan G.
Is Plan F available for 2020?
80 %. * Plan F and Plan C are not available to Medicare beneficiaries who became eligible for Medicare on or after January 1, 2020. If you became eligible for Medicare before 2020, ... you may still be able to enroll in Plan F or Plan C as long as they are available in your area.
Can I sell my Medicare Part B policy?
As part of that act, from January 1, 2020, insurers couldn't sell a policy that covers the annual Medicare Part B deductible to new Medicare beneficiaries. This ruling effectively meant insurers couldn't offer Plan F or Medigap Plan C ...
How many doctors don't accept Medicare?
Only about 4% of American doctors don’t accept Medicare. And if you’re a Medicare beneficiary, as you can see, provider enrollment can make a huge difference, primarily for your pocketbook.
What are the benefits of choosing a doctor who accepts Medicare?
Benefits of Choosing a Doctor Who Accepts Medicare. When you use a doctor who accepts Medicare, you’ll know exactly what to expect when you pay the bill. An enrolled provider won’t charge more than the Medicare-approved amount for covered services.
What happens if you opt out of Medicare Supplement?
If you use a Medicare Supplement plan, your benefits won’t cover any services when your provider has opted out of Medicare. When you see a non-participating provider, you may have to pay the “limiting charge” in addition to your copay. The limiting charge can add up to 15% of the Medicare-approved amount to your bill.
How much does a limiting charge add to Medicare?
The limiting charge can add up to 15% of the Medicare-approved amount to your bill. If your provider has opted out of Medicare, the limiting charge does not apply, and your provider can bill any amount he or she chooses. Of course, Medicare provider enrollment is just one of the things you’ll need to consider when you choose a doctor.
Do Medicare enrollees have to accept Medicare?
Medicare-Enrolled Providers will only charge the Medicare-approved amount for covered services and often cost less out of pocket than services from doctors who don’t accept Medicare. Non-Participating Providers have no obligation to accept the Medicare-approved amount. However, they can choose to do so for any service.
Can you use a Medicare Advantage card if you switch to Original Medicare?
You’ll use your Medicare Advantage card when you seek care, but hold on to both cards in case you switch back to Original Medicare. (Medicare’s hospice benefit is covered through Original Medicare even if you’re enrolled in a Medicare Advantage plan.)
Does Medicare change your insurance card?
Insurers will usually send you a new card each year, although your Original Medicare card will not change.
Does Medicare cover urgent care?
Medicare Advantage plans must cover emergency room and urgent care at in-network rates even if you are treated out-of-network. Some plans cover routine out-of-network care, meaning you can see any Medicare provider for routine care. (These plans will have a separate out-of-pocket maximum for out-of-network services.)
Does Medicare Advantage have access to physicians?
While Original Medicare is known for offering expansive access to physicians, it is not always a guarantee of access to a specific physician. Some medical practices only take patients with Medicare Advantage plans, while others see patients who have Original Medicare.
Do all Advantage plans have to include an adequate number of providers and hospitals in their networks?
If you have to seek routine care from an out-of-network provider, your insurer may agree to cover it at in-network rates if an appropriate provider is unavailable in-network.