Morphine infusion via an external infusion pump is covered when used in the treatment of intractable pain caused by cancer (in either an inpatient or outpatient setting, including a hospice). e. Continuous Subcutaneous Insulin Infusion (CSII) Pumps (Effective for Services Performed On or after December 17, 2004)
Is morphine covered by Medicare?
Some Medicare plans have restrictions on coverage of morphine that may include: Quantity Limits. Most Medicare plans restrict the amount of this prescription that can be purchased at one time. If you need to purchase a greater amount at one time, it may not be covered.
Does Medicare cover infusion pumps?
Medicare Part B (Medical Insurance) covers infusion pumps (and some medicines used in infusion pumps) if considered reasonable and necessary. These are covered as durable medical equipment (DME) that your doctor prescribes for use in your home.
Does Medicare cover prescription opioids?
Prescription opioids, like hydrocodone (Vicodin®), oxycodone (OxyContin®), morphine, codeine, and fentanyl can be used to help relieve severe pain. Some Medicare plans have certain coverage rules to help you use opioids safely. Get more information on drug plan coverage rules.
What are intrathecal morphine pumps used to treat?
Intrathecal morphine pump as a treatment option in chronic pain of nonmalignant origin. Surg Neurol. Jan 1998;49 (1):92-8. Chang HM. Chronic Pain, Cancer Pain Management. Med. Clinics of North America.

Does insurance pay for pain pump?
covers infusion pumps (and some medicines used in infusion pumps) if considered reasonable and necessary. These are covered as durable medical equipment (DME) that your doctor prescribes for use in your home.
Does Medicare cover nerve block injections?
Medicare does not have a National Coverage Determination (NCD) for paravertebral facet joint/nerve blocks: diagnostic and therapeutic.
Does Medicare cover Baclofen pump?
ITB therapy with Lioresal® Intrathecal (baclofen injection) with related medical care and medication is an FDA-approved, commercially available treatment for severe spasticity that is covered for the approved uses by most health insurance companies, Medicare, and most state Medicaid programs.
How many epidurals does Medicare allow in a year?
How many epidural steroid injections will Medicare cover per year? Medicare will cover epidural steroid injections as long as they're necessary. But, most orthopedic surgeons suggest no more than three shots annually.
What should I not tell my pain management doctor?
Don'ts: Things Pain Patients Wish Doctors Would AvoidDon't label patients. ... Don't tell patients the pain is 'in our heads. ... Don't tell us to just 'live with the pain.
Are cortisone injections covered by Medicare?
Does Medicare Cover Cortisone Shots? Medicare guidelines state that cortisone injections usually have coverage. Using this medication to treat inflammation, it goes directly into the problematic joint area. Make sure to check with your medical provider.
How do you qualify for a pain pump?
Who is a candidate?Conservative therapies have failed.You would not benefit from additional surgery.You are dependent on pain medication.You do not have psychological problems.You have no medical conditions that would keep you from undergoing implantation.You are not allergic to any of the drugs used in the pump.More items...
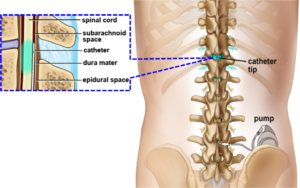
Is a baclofen pump considered infusion therapy?
ITB Therapy with Lioresal® Intrathecal (baclofen injection) for the management of severe spasticity uses an implantable infusion system to deliver precise amounts of Lioresal® Intrathecal (baclofen injection) directly to the intrathecal space via a surgically implanted infusion pump and catheter.
Is baclofen a Tier 1?
What drug tier is baclofen typically on? Medicare prescription drug plans typically list baclofen on Tier 2 of their formulary.
What is the average cost of an epidural steroid injection?
On MDsave, the cost of an Epidural Steroid Injection ranges from $1,027 to $1,487. Those on high deductible health plans or without insurance can save when they buy their procedure upfront through MDsave. Read more about how MDsave works.
Are epidural steroid injections FDA approved 2021?
Epidural injections of corticosteroids are a common treatment offered to patients who experience back pain, neck pain, or pain that radiates to the arms and legs. However, such injections are not FDA approved, and there is limited evidence backing their safety or effectiveness, according to the agency.
Does Medicare pay for lidocaine injections?
Yes. 100% of Medicare prescription drug plans cover this drug.
Prefer to talk?
You can talk to one of our friendly licensed sales agents on the phone during our opening hours. They're fully trained and happy to help. No question is too small!
Still have questions?
Our Advice Center contains important information you should know about Medicare. So if you have a question, the answer is just a click away.
What drug tier is morphine typically on?
Medicare prescription drug plans typically list morphine on Tier 2 of their formulary. Generally, the higher the tier, the more you have to pay for the medication. Most plans have 5 tiers.
What is the deductible stage of a drug?
In the Deductible stage, you may be responsible for the full cost of your drug.
What is the post deductible stage?
After your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost. In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for your drug.
What is the donut hole in Medicare?
In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for your drug. Therefore, you may pay more for your drug.
Is Medicare price accurate?
Medicare prices are provided by the Centers for Medicare and Medicaid Services (CMS). They are accurate as-of April 2020 and the information may be updated. If you encounter any issues, please let us know .
Does Medicare have a quantity limit?
Most Medicare prescription drug plans have quantity limits to restrict the amount of this drug that can be filled at one time.
Does Medicare cover lifestyle concerns?
While Medicare does provide coverage for a large variety of durable medical equipment, it does not currently cover medical treatment for lifestyle concerns, meaning treatment to enhance sexual activity is not covered.
Does Medicare pay for ED pumps?
As a result, Medicare does not generally pay for ED pumps unless the use of such devices is an integral part of a larger treatment approach to a serious medical condition.
Does Medicare cover erectile dysfunction?
Medicare and Erectile Dysfunction Hospital Treatment. Medicare benefits under Part A generally provide for care in a skilled nursing facility or while hospitalized, but once again, the rule regarding medical necessity would apply to erectile dysfunction treatment in these situations. While it’s extremely unlikely that a man would be treated ...
Does Medicare cover vacuum constriction?
Although Medicare does not cover the cost of a vacuum constriction device or related sexual aides, some men may be able to receive coverage for certain erectile dysfunction medications if they are prescribed for a condition other than erectile dysfunction.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What percentage of Medicare payment does a supplier pay for assignment?
If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment:
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers infusion pumps (and some medicines used in infusion pumps) if considered reasonable and necessary. These are covered as durable medical equipment (DME) that your doctor prescribes for use in your home.
Does Medicare cover DME equipment?
You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.
Do DME providers have to accept assignment?
If suppliers are participating suppliers, they must accept assignment (which means, they can charge you only the coinsurance and Part B deductible for the Medicare‑approved amount). If suppliers aren’t participating and don’t accept assignment , there’s no limit on the amount they can charge you. Medicare won’t pay claims for doctors or suppliers who aren’t enrolled in Medicare.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. for visits to your doctor or other.
What are the optional benefits of Medicare?
helps pay for: Medication Therapy Management programs for complex health needs. Opioid pain medication.
What is coinsurance in healthcare?
An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%). amount to the hospital. You pay nothing for a yearly depression screening if your doctor or health care provider accepts assignment.
What is a health care provider?
for visits to your doctor or other. health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. to diagnose or treat your condition.
Does Medicare cover m assage?
Your doctor may recommend treatment options that Medicare doesn’t cover. For example, Medicare doesn't cover m assage therapy. If this happens, or if your doctor or other health care provider recommends you get services more often than Medicare covers, you may have to pay some or all of the costs.
Do you pay for a depression screening?
You pay nothing for a yearly depression screening if your doctor or health care provider accepts assignment.
Can you take prescription pain medication with Medicare?
While prescription pain medications covered under Medicare prescription drug coverage (Part D) may be effective at treating certain types of pain , especially during short-term use, you might be able to take other medications or do other things to help effectively manage your pain with less risk long term.
What is an external chemo pump?
The external chemotherapy infusion pump is covered when used in the treatment of primary hepatocellular carcinoma or colorectal cancer where this disease is unresectable; OR, where the patient refuses surgical excision of the tumor.
What labeling is needed for a pump?
The Food and Drug Administration-approved labeling for the pump must specify that the drug being administered and the purpose for which it is administered is an indicated use for the pump.
When did the TN 67 infusion pump come into effect?
Effective date 03/04/1994. (TN 67)
Is heparin covered by external infusion pumps?
When used in the administration of heparin for the treatment of thromboembolic disease and/or pulmonary embolism, only external infusion pumps used in an institutional setting are covered.
Is morphine covered by hospice?
Morphine infusion via an external infusion pump is covered when used in the treatment of intractable pain caused by cancer (in either an inpatient or outpatient setting, including a hospice).
Does Medicare cover CSII?
The Centers for Medicare & Medicaid Services will continue to allow coverage of all other uses of CSII in accordance with the Category B investigational device exemption clinical trials regulation (42 CFR 405.201) or as a routine cost under the clinical trials policy (Medicare National Coverage Determinations Manual 310.1 ).
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Articles. CMS believes that the Internet is an effective method to share Articles that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Does CMS have a CDT license?
Organizations who contract with CMS acknowledge that they may have a commercial CDT license with the ADA, and that use of CDT codes as permitted herein for the administration of CMS programs does not extend to any other programs or services the organization may administer and royalties dues for the use of the CDT codes are governed by their commercial license.
What is a patch pump?
Tubed pumps have a small tube or tubes that extend from the insulin in the pump to deliver the insulin to you. Patch pumps don’t have tubes, so that means fewer connections. Currently only one patch pump, called the Omnipod, is on the market, though several companies are developing other versions.
What is a Medigap policy?
Medigap is a Medicare supplemental insurance policy for people with original Medicare. Medicare standardizes these policies.
How much does an insulin pump cost?
According to a 2018 article in Modern Healthcare, the Omnipod tubeless insulin pump may cost as much as $3,000 to $4,000 per month. Both of these costs are before Medicare pays a portion. Insulin pump costs can vary by manufacturer and model.
What is Part B for Medicare?
Part B typically covers doctor’s office visits and durable medical equipment, such as wheelchairs or crutches. Medicare considers an insulin pump a piece of durable medical equipment. You must meet certain requirements for a doctor to prescribe the pump.
What is Medicare Part A?
Medicare Part A is the first part of original Medicare. It’s the Medicare portion that provides hospital and rehabilitation care.
Does Medicare cover tubeless insulin pumps?
You select a Medicare Part D plan from a private insurance company. Some plans cover tubeless insulin pumps, but not all do. Part D plans have a list of covered medications, called a formulary. Often, plans don’t include the tubeless insulin pump on their formulary.
Does Medicare pay for insulin pumps?
Medicare will pay a portion of the cost for an insulin pump, as long as a doctor prescribes the pump and you meet certain criteria. Which part of Medicare pays for the pump depends on the type of pump you choose. Besides purchasing the pump, you may also have to pay for a portion of supplies, such as tubing and infusion sets.
