What diagnosis will Medicare cover for a DEXA scan?
Medicare Part B* (Medical Insurance) covers bone density test (DXA) as part of preventive screening once every 24 months (or more often if medically necessary) if you meet one or more of these conditions: You’re a woman whose doctor determines you’re estrogen deficient and at risk for osteoporosis, based on your medical history and other findings.
How often will Medicare pay for DEXA scan?
Medicare will pay for a bone density test (DXA) as part of preventive screening every two years for women 65 or older and men 70 or older. Many insurance providers will cover the test under certain circumstances.
Does Medicare cover a DEXA scan?
Medicare Part B usually covers the costs associated with a DEXA scan. Part B is the branch of Medicare that provides coverage benefits for medically-necessary outpatient procedures to help treat an ongoing illness.
How much does it cost to get a DEXA scan?
What to expect from a DEXA scan session. I booked an appointment with a large clinic in the Sydney CBD. The cost for a 30-minute session was $160, which includes the scan itself and a review afterwards with an accredited exercise physiologist.
What diagnosis covers DEXA scan for Medicare?
Medicare will cover bone density scans for a person who meets certain medical requirements, such as osteoporosis risk factors. Identifying thinning bone or osteoporosis at early stages before a person breaks a bone can allow them to receive treatments that may help reduce the risk of broken bones.
What ICD-10 code covers DEXA scan for Medicare 2021?
ICD-10 CM code Z79. 83 should be reported for DXA testing while taking medicines for osteoporosis/osteopenia. ICD-10 CM code Z09 should be reported for an individual who has COMPLETED drug therapy for osteoporosis and is being monitored for response to therapy.
What ICD-10 will Medicare cover for DEXA scan?
Many ICD-10 codes cover fractures, but there are other ICD-10 codes Medicare will cover when used with a DXA Bone Scan (77080): 0 // Asymptomatic menopausal state. 3 // Long term (current) use of hormonal contraceptives.
Who qualifies for DEXA scan?
The National Osteoporosis Foundation recommends people at average risk get a DEXA scan starting at 65 (women) and 70 (men). Family history: If one or more family members have had osteoporosis or more than one fracture, you could be at a higher risk for bone loss.
Does Medicare cover DEXA?
In most cases, Medicare insurance does cover DEXA scans under Part B. Medicare Part B (Medical Insurance) provides benefits for outpatient procedures that are deemed medically necessary for ongoing treatment of illness.
How often does Medicare pay for bone density scan?
once every 24 monthsBone mass measurements covers this test once every 24 months (or more often if medically necessary) if you meet one of more of these conditions: You're a woman whose doctor determines you're estrogen-deficient and at risk for osteoporosis, based on your medical history and other findings.
What diagnosis codes cover bone density?
77080CodeDescriptionM85.841Other specified disorders of bone density and structure, right handM85.842Other specified disorders of bone density and structure, left handM85.851Other specified disorders of bone density and structure, right thighM85.852Other specified disorders of bone density and structure, left thigh124 more rows
How do you bill for a DEXA scan?
Billing CPT 77080, 77081, 77082 with covered dxREIMBURSEMENT CODES FOR BONE DENSITOMETRY.CPT Code 77080 – Hip, spine or central DEXA (Dual Energy X-Ray Absorptiometry) studies. ... CPT Code 77081 – Peripheral DEXA Bone Mineral Density – $27.72.CPT Code 77082 – Peripheral Ultrasound Bone Mineral Density.Indications for DEXA.
What is the ICD-10 code for screening for osteoporosis?
Z13. 820 Encounter for screening for osteoporosis - ICD-10-CM Diagnosis Codes.
What is normal bone density for a 70 year old woman?
It is recommended that women < 70 years old are treated if the bone mineral density T-score is below -2.5. For women > or = 70 years of age, a lower cut-off point has been chosen, i.e. a Z-score below -1.
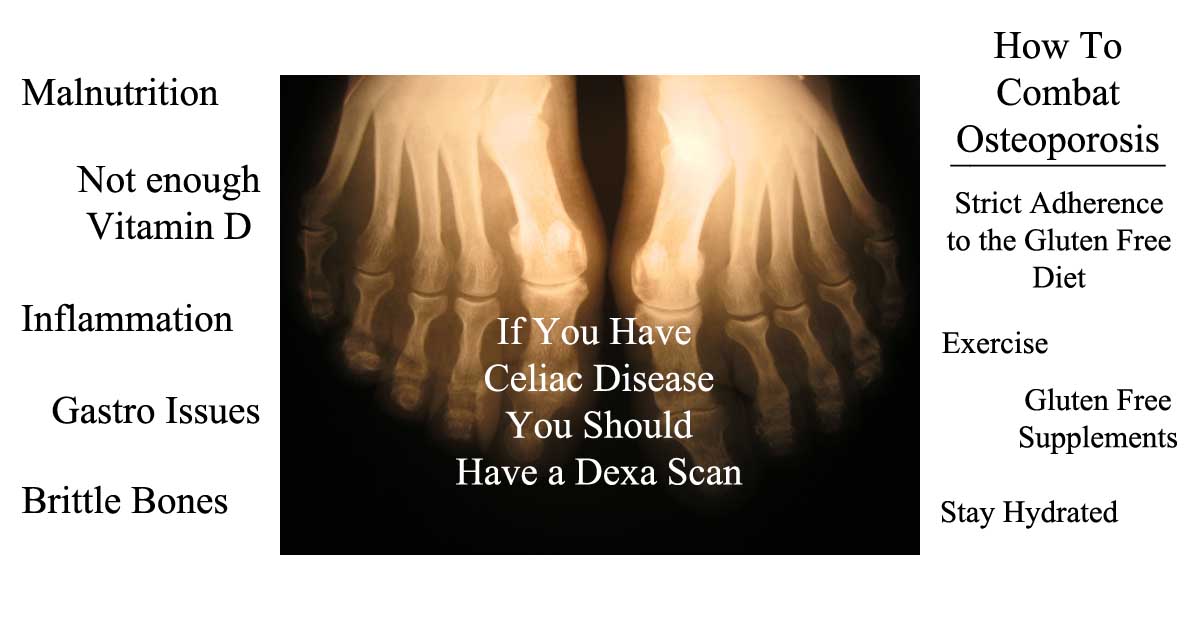
What is the difference between a DEXA scan and a bone density test?
A bone density test, also referred to as a DEXA scan, is a noninvasive test that measures calcium and other minerals in your bones. It measures the strength and thickness, or mass, of your bones. As we age, bones naturally become thinner. Osteopenia occurs when bones are thinner than normal.
What is considered severe osteoporosis?
Severe (established) osteoporosis is defined as having a bone density that is more than 2.5 SD below the young adult mean with one or more past fractures due to osteoporosis.
What are the risk factors for DXA?
With any one of these factors, your insurance company should cover a DXA. 1) Early menopause (before age 40) 2) Adults with a prior low-impact fracture. 3) Adults with a disease or condition ...
Does Medicare cover bone density?
Medicare coverage. Medicare will pay for a bone density test (DXA) as part of preventive screening every two years for women 65 or older and men 70 or older. Many insurance providers will cover the test under certain circumstances.
Medicare Coverage Of Osteoporosis Medications
Many medications available today can slow the rate of bone loss and, in some cases, even rebuild bone strength.
Who Should Undergo A Bone Density Test
Postmenopausal women, men ages 70 and older, or those who recently suffered from a broken bone are advised to take a bone density test. Women are at high risk for osteoporosis. Bone loss is women is fastest during the first few years after menopause and continues into old age.
Osteoporosis And Its Complications
Osteoporosis is a medical condition characterized by architectural weakening in the bones and decreased bone mass. These changes make the bones more fragile and increase the risk of fractures, especially at the spine, hip, and wrist.
Risk Factors For Osteoporosis
When you think of osteoporosis, you likely think of women. It is true that postmenopausal women are at highest risk for the condition. Once their bodies no longer produce premenopausal levels of estrogen, the protective benefits of the hormone on their bones go away.
Does Medicare Cover Bone Density Testing
Fortunately, Medicare feels that bone health is essential and can help you get excellent bone care, whether it be testing or treatment. There are about 10 million people in the United States alone with Osteoporosis and almost 34 million more with low bone mass.
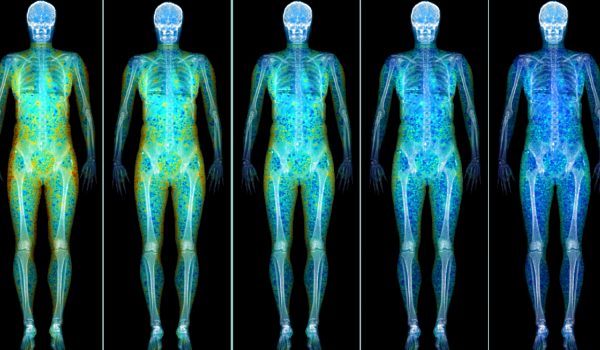
How Is Bone Density Testing Done
Bone density testing is typically done in a clinical setting such as a hospital or an outpatient facility. After putting on a loose gown, youll be asked to lie on a padded platform. A suspended mechanical arm then passes over parts of your body, taking images of your skeleton.
How To Get Help Covering The Cost Of Bone Density Testing Under Medicare
Supplemental plans fill in the gaps by covering the 20% you would otherwise pay under Part B. By relieving you of this cost, you can worry less about bills and more about recovery. The best part about a supplement is that when Medicare approves a service, the supplement must authorize the service as well.
What to expect from bone density test?
What to Expect. Bone density tests are painless and don’t require much preparation. Aside from avoiding calcium supplements 24 hours in advance, you should wear loose, comfortable clothing. Several bone density tests use ultrasound, urine tests, and X-rays or some form of radiation, such as: DXA (Dual-energy X-ray Absorptiometry)
Can you get a hyperparathyroid test with Medicare?
The test may be ordered more often if your physician deems it medically necessary. If you have Original Medicare, you will pay nothing for this test as long as your doctor accepts assignment.
How often does Medicare cover bone density?
Because certain conditions put you at a higher risk for bone problems and related injuries, Medicare covers bone density testing once every 24 months. You may qualify for more frequent testing if you have any of the following conditions, which could lead to decreased bone density: rheumatoid arthritis. chronic kidney disease.
How long has it been since your last bone density scan?
It’s been 23 months since your last bone density scan or you have a condition that needs more frequent testing. The facility where the scan is done accepts Medicare. To check whether a medical facility participates in Medicare, click here.
Do you have to have a bone density test if you have Medicare?
If you need to have a bone density test more often, your doctor will have to provide proof of a reason for more frequent testing. You may be asked to have your test done within a certain network if you have a Medicare Advantage plan. If you go outside your network, you may have to pay a share of the testing cost.
Does Medicare Advantage match Part A?
Medicare Advantage (Part C) must match the coverage of original Medicare (Part A and Part B). However, each plan may have its own requirements on where you can be tested and how much your share of the cost will be.
Can a radiology doctor perform a bone density scan?
Most outpatient facilities with radiology services can perform a bone density scan. This may be: The basic conditions for coverage are: Your doctor has ordered the scan as a medically necessary test. It’s been 23 months since your last bone density scan or you have a condition that needs more frequent testing.
About this Community
The Bone Health and Osteoporosis Foundation Support Community connects patients, families, friends and caregivers for support and inspiration. This community is sponsored by the Bone Health and Osteoporosis Foundation, an Inspire trusted partner.
Has anyone used the Marodyne LiV to help with their osteoporosis?
I’m 59 and diagnosed with osteoporosis last October after falling and breaking both elbows. I have been o Alendronic Acid for 5 months with some side effects so cane of it. Now taking a range of supplements and being more active. I’d love to hear from anyone who has used or knows about the Marodyne LiV plate. Thanks Mary Sign up to continue reading
Marodyne vs Juvent LIV (vibration devices)
I've been reading a few posts about low intensity vibration devices, and especially about how they compare to each other, so I thought I'd take the plunge and start a discussion ... never done this before on the internet! So, please be kind... The Marodyne device (LIVmd) and the Juvent device are basically the same technology.
Rib pain after compression fractures... looking for solutions
I am recovering from multiple compression fractures, last one 8-24, my abdominal muscles are very weak but hopefully slowly improving. My ribs (front), are so sore....at bottom. Know area comprised due to loss of height, but not sure why so sore at base of ribs..almost more sore than back.
Vit K2-7 Heart Arrhythmias and Palpitations
Dear Friends, I have already posted a discussion on which is better Vitamin K2-7 or Vitamin K2-4 and the overall consensus there seems to be that K2-4 has much less side effects.
Pain after kyphoplasty
I had a kyphoplasty done on November 2, 2016 for an L5 fracture. I have not gotten any relief from the pain and it is now two and a half months after the procedure. I do have very bad osteoporosis, (four back fractures altogether), but thought that I would get some relief.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This First Coast Billing and Coding Article for Local Coverage Determination (LCD) L36356 Bone Mineral Density Studies provides billing and coding guidance for frequency limitations as well as diagnosis limitations that support diagnosis to procedure code automated denials.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.