The Medicare enrollment period is:
- You can initially enroll in Medicare during the seven-month period that begins three months before you turn age 65.
- If you continue to work past age 65, sign up for Medicare within eight months of leaving the job or group health plan to avoid penalties.
- The six-month Medicare Supplement Insurance enrollment period begins when you are 65 or older and enrolled in Medicare Part B.
Full Answer
When can you enroll in Medicare supplement?
Medicare Supplement Insurance (Medigap) has a six-month open enrollment period (OEP). Your open enrollment period begins when you are both: 65 years old and. Enrolled in Medicare Part B. Unlike the Medicare OEP that happens once every year, you have only one Medigap OEP. If you get Medicare Part B before you turn 65, your Medigap OEP starts the ...
When can you start applying for Medicare?
You’re first eligible to sign up for Medicare 3 months before you turn 65. You may be eligible to get Medicare earlier if you have a disability, End-Stage Renal Disease (ESRD), or ALS (also called Lou Gehrig’s disease). Follow these steps to learn about Medicare, how to sign up, and your coverage options. Learn about it at your own pace. Step 1
When is the best time to apply for Medicare?
To help you learn all about Medicare health plans enrollment and the best time to enroll, we have put together all the information you need. To answer your question simply, the best time for people to sign up for Medicare is the age of 65, and it is even better if you apply a few months before 65 to avail Medicare as soon as you turn 65.
What is the best medical supplement for Medicare?
- You must have Medicare Part A and Part B.
- A Medigap policy is different from a Medicare Advantage Plan. ...
- You pay the private insurance company a monthly premium The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. ...
- A Medigap policy only covers one person. ...
What is the deadline for choosing a Medicare Supplement plan?
If you're enrolled in a Medicare Advantage plan and use the Medicare Advantage open enrollment period (January 1 to March 31) to switch to Original Medicare, you'll also have the option to sign up for a Part D plan to supplement your Original Medicare coverage.
Can you add a Medicare Supplement anytime?
One interesting feature of Medicare Supplement insurance plans is that you can apply for a plan anytime – you only need to be enrolled in Medicare Part A and Part B. However, a plan doesn't have to accept your application, unless you have guaranteed-issue rights.
How far in advance can I apply to a Medicare Supplement?
The best time to buy a Medigap policy is the 6-month period that starts the first day of the month you're 65 or older and enrolled in Part B. For example, if you turn 65 and are enrolled in Part B in June, the best time for you to buy a Medigap policy is from June to November.
Can Medicare Supplement plans be purchased any time of the year?
If you're in good health and comfortable answering medical questions, you can apply to change Medigap plans at any time of the year. Medicare Advantage plans and Medicare Part D prescription drug plans can only be changed during certain times of year, but Medicare supplements are different.
Can I switch from Medicare Advantage to Medicare Supplement?
Once you've left your Medicare Advantage plan and enrolled in Original Medicare, you are generally eligible to apply for a Medicare Supplement insurance plan. Note, however, that in most cases, when you switch from Medicare Advantage to Original Medicare, you lose your “guaranteed-issue” rights for Medigap.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
How long is the guaranteed issue period for Medicare Supplement?
63 daysIf you joined Medicare Advantage when you first became eligible for Medicare, but decided to switch to Original Medicare within the first 12 months, you have Medicare Supplement guaranteed issue rights for 60 days before your plan ends and 63 days after you switch.
Can I change my Medicare Supplement plan at any time?
As a Medicare beneficiary, you can change supplements at any time. As a result, there's no guarantee an application will be accepted if switched outside the designated Open Enrollment Period. An application may be “medically underwritten”.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
How long before you turn 65 do you apply for Medicare?
3 monthsYour first chance to sign up (Initial Enrollment Period) It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month.
Does Medicare coverage start the month you turn 65?
For most people, Medicare coverage starts the first day of the month you turn 65. Some people delay enrollment and remain on an employer plan. Others may take premium-free Part A and delay Part B. If someone is on Social Security Disability for 24 months, they qualify for Medicare.
Can Medigap insurance be denied for pre-existing conditions?
Be aware that under federal law, Medigap policy insurers can refuse to cover your prior medical conditions for the first six months. A prior or pre-existing condition is a condition or illness you were diagnosed with or were treated for before new health care coverage began.
When can I enroll in Medicare Advantage Plan A?
You're automatically eligible for Plan A if you’re 65 or older. If you’re under age 65, you are eligible for Plan A if you’ve lost coverage under a group policy after becoming eligible for Medicare. You can also enroll if you had Plan A, then enrolled in a Medicare Advantage plan, and now would like to return to Plan A.
How long do you have to live in Michigan to get Medicare Supplement?
Are enrolled in both Medicare Part A hospital and Part B medical insurance. Live in Michigan for at least six months of the year. Applying for these plans isn't restricted to certain times of the year like Medicare Advantage plans.
How long do you have to be in Medicare Advantage to return to Plan C?
You can do this as long as it’s within the first 12 months of your Medicare Advantage plan. You're automatically eligible for Plan A if you’re 65 or older. If you’re under age 65, you are eligible for Plan A ...
Does Blue Cross Blue Shield of Michigan cover Medicare Supplement?
Blue Cross Blue Shield of Michigan administers Blue Cross Medicare Supplement plans. Where you live, your age, gender and whether you use tobacco may affect what you pay for your plan. Your health status may also affect what you pay. This is a solicitation of insurance. We may contact you about buying insurance.
Can you stay with Blue Cross Medicare Supplement?
government or the federal Medicare program. If you're currently enrolled in Plan A or Plan C, you can stay with your plan as long as you pay your premium.
Can I go to a doctor for Medicare?
The Medicare deductibles, coinsurance and copays listed are based on the 2019 numbers approved by the Centers for Medicare and Medicaid Services. You can go to any hospital, doctor or other health care provider in the U.S. or its territories that accepts Medicare. You don't have to use our network.
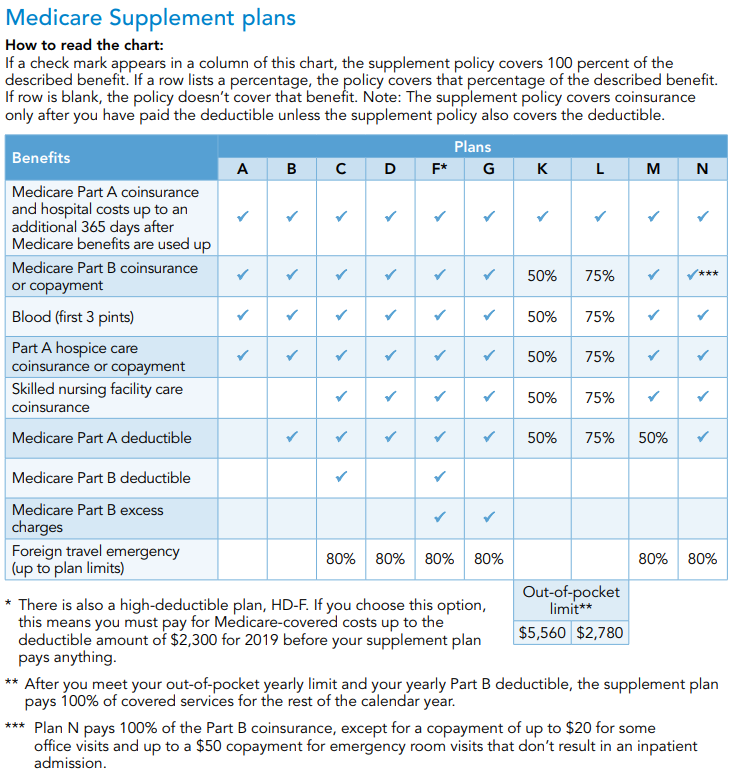
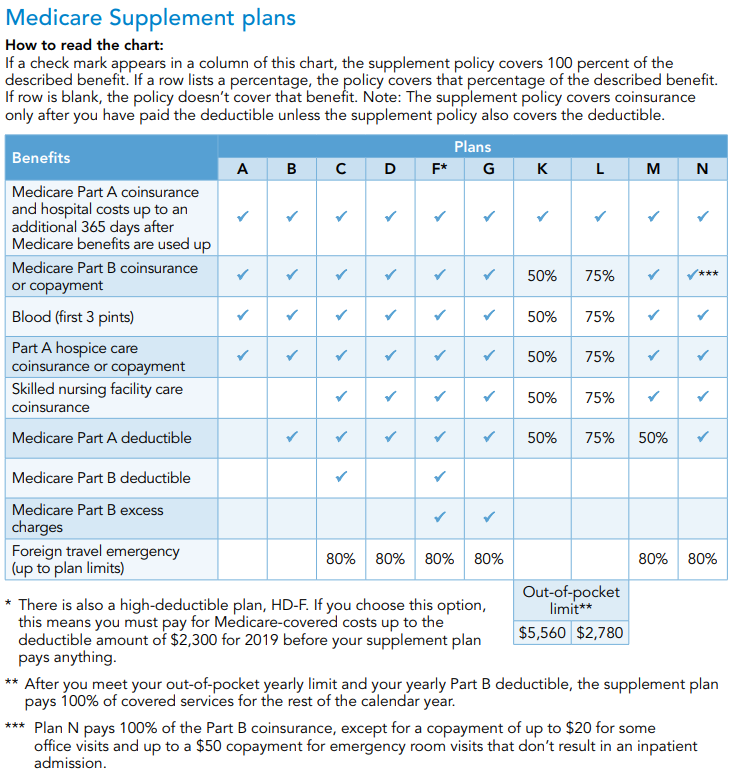
What is Medicare Supplement Insurance?
Medicare Supplement Insurance (Medigap or MedSup), sold by private companies, helps pay some health care costs that Original Medicare (Part A and Part B) doesn’t cover. Policies can include coverage for deductibles, coinsurance, hospital costs, skilled nursing facility costs, and sometimes health care costs when traveling outside the U.S.
How long is the free look period for Medigap?
If you’re within your six-month Medigap Open Enrollment Period and considering a different Medigap plan, you may try a new Medigap policy during a 30-day “free look period.”. During this period, you will have two Medigap plans, and pay the premium for both.
What happens if a Medigap policy goes bankrupt?
Your Medigap insurance company goes bankrupt and you lose your coverage , or your Medigap policy coverage otherwise ends through no fault of your own. You leave a Medicare Advantage plan or drop a Medigap policy because the company hasn’t followed the rules, or it misled you.
Answer a few questions to find out
These questions don’t apply if you have End-Stage Renal Disease (ESRD).
Do you have health insurance now?
Are you or your spouse still working for the employer that provides your health insurance coverage?
Your first chance to sign up (Initial Enrollment Period)
Generally, when you turn 65. This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65.
Between January 1-March 31 each year (General Enrollment Period)
You can sign up between January 1-March 31 each year. This is called the General Enrollment Period. Your coverage starts July 1. You might pay a monthly late enrollment penalty, if you don’t qualify for a Special Enrollment Period.
Special Situations (Special Enrollment Period)
There are certain situations when you can sign up for Part B (and Premium-Part A) during a Special Enrollment Period without paying a late enrollment penalty. A Special Enrollment Period is only available for a limited time.
Joining a plan
A type of Medicare-approved health plan from a private company that you can choose to cover most of your Part A and Part B benefits instead of Original Medicare. It usually also includes drug coverage (Part D).
When to buy Medigap policy?
Buy a policy when you're first eligible. The best time to buy a Medigap policy is during your 6-month Medigap Open Enrollment Period. You generally will get better prices and more choices among policies. During that time you can buy any Medigap policy sold in your state, even if you have health problems. This period automatically starts the first ...
What is a select Medicare policy?
Medicare Select. A type of Medigap policy that may require you to use hospitals and, in some cases, doctors within its network to be eligible for full benefits. . If you buy a Medicare SELECT policy, you have rights to change your mind within 12 months and switch to a standard Medigap policy.
How long does it take for a pre-existing condition to be covered by Medicare?
Coverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded. When you get Medicare-covered services, Original Medicare.
Can Medigap refuse to cover out-of-pocket costs?
A health problem you had before the date that new health coverage starts. . In some cases, the Medigap insurance company can refuse to cover your. out-of-pocket costs. Health or prescription drug costs that you must pay on your own because they aren’t covered by Medicare or other insurance.
Can you shorten the waiting period for a pre-existing condition?
It's possible to avoid or shorten waiting periods for a. pre-existing condition. A health problem you had before the date that new health coverage starts. if you buy a Medigap policy during your Medigap open enrollment period to replace ".
Can you get Medicare if you are 65?
Some states provide these rights to all people with Medicare under 65. Other states provide these rights only to people eligible for Medicare because of disability or only to people with ESRD. Check with your State Insurance Department about what rights you might have under state law.
Can you charge more for a Medigap policy?
Charge you more for a Medigap policy. In some cases, an insurance company must sell you a Medigap policy, even if you have health problems. You're guaranteed the right to buy a Medigap policy: When you're in your Medigap open enrollment period. If you have a guaranteed issue right.
What happens if you don't get Medicare?
If you don't get Medicare drug coverage or Medigap when you're first eligible, you may have to pay more to get this coverage later. This could mean you’ll have a lifetime premium penalty for your Medicare drug coverage . Learn more about how Original Medicare works.
How much does Medicare pay for Part B?
For Part B-covered services, you usually pay 20% of the Medicare-approved amount after you meet your deductible. This is called your coinsurance. You pay a premium (monthly payment) for Part B. If you choose to join a Medicare drug plan (Part D), you’ll pay that premium separately.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is the original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). (Part A and Part B) or a.
Does Medicare Advantage cover prescriptions?
Most Medicare Advantage Plans offer prescription drug coverage. . Some people need to get additional coverage , like Medicare drug coverage or Medicare Supplement Insurance (Medigap). Use this information to help you compare your coverage options and decide what coverage is right for you.
How does Medicare work with my job-based health insurance when I stop working?
Once you stop working, Medicare will pay first and any retiree coverage or supplemental coverage that works with Medicare will pay second.
When & how do I sign up for Medicare?
You can sign up anytime while you (or your spouse) are still working and you have health insurance through that employer. You also have 8 months after you (or your spouse) stop working to sign up.
Do I need to get Medicare drug coverage (Part D)?
Prescription drug coverage that provides the same value to Medicare Part D. It could include drug coverage from a current or former employer or union, TRICARE, Indian Health Service, VA, or individual health insurance coverage.
