When to enroll in Medicare if still working?
Feb 08, 2022 · When to Sign Up for Medicare When Still Working You can (and should) enroll in Part A as soon as you’re eligible, regardless of your working status. If your company has fewer than 20 employees, you’ll likely need to enroll in Part B. Those enrolled in Part A who want prescription drug coverage – but ...
Should you enroll in Medicare while still working?
Generally, if you have job-based health insurance through your (or your spouse’s) current job, you don’t have to sign up for Medicare while you (or your spouse) are still working. You can wait to sign up until you (or your spouse) stop working or you …
Who pays if you are Medicare eligible but still work?
Dec 22, 2021 · Generally, we advise people to file for Medicare benefits 3 months before age 65. Remember, Medicare benefits can begin no earlier than age 65. If you are already receiving Social Security, you will automatically be enrolled in Medicare Parts A and B …
Should I sign up for Medicare if I am still working?
A: Medicare eligibility begins at age 65, and signing up on time can help you avoid premium surcharges. But if you’re working at 65, you get a bit more leeway. You can’t add your family to your Medicare coverage. Learn how to make sure they have health insurance once you’re enrolled. Medicare eligibility starts at age 65.

When should I start my Medicare application?
Generally, you're first eligible starting 3 months before you turn 65 and ending 3 months after the month you turn 65. If you don't sign up for Part B when you're first eligible, you might have to wait to sign up and go months without coverage.
Can you get Medicare while working?
You can get Medicare if you're still working and meet the Medicare eligibility requirements. You become eligible for Medicare once you turn 65 years old if you're a U.S. citizen or have been a permanent resident for the past 5 years. You can also enroll in Medicare even if you're covered by an employer medical plan.
Can I keep my Medicare if I go back to work?
Under this law, how long will I get to keep Medicare if I return to work? As long as your disabling condition still meets our rules, you can keep your Medicare coverage for at least 8 ½ years after you return to work. (The 8 ½ years includes your nine month trial work period.)
What should I be doing 3 months before 65?
You can first apply for Medicare during the three months before your 65th birthday. By applying early, you ensure your coverage will start the day you turn 65. You can also apply the month you turn 65 or within the following three months without penalty, though your coverage will then start after your birthday.Nov 22, 2021
How long does it take to get Medicare?
Learn how to make sure they have health insurance once you’re enrolled. Medicare eligibility starts at age 65. Your initial window to enroll is the seven-month period that begins three months before the month of your 65th birthday and ends three months after it. Seniors are generally advised to sign up on time to avoid penalties ...
What happens if you don't sign up for Medicare?
Specifically, if you fail to sign up for Medicare on time, you’ll risk a 10 percent surcharge on your Medicare Part B premiums for each year-long period you go without coverage upon being eligible.
Does Medicare pay for Part A?
That said, it often pays to enroll in Medicare Part A on time even if you have health coverage already. It won’t cost you anything, and this way, Medicare can serve as your secondary insurance and potentially pick up the tab for anything your primary insurance (in this case, your work health plan) doesn’t cover.
How long can you delay Medicare?
As long as you have group health insurance from an employer for which you or your spouse actively works after you turn 65, you can delay enrolling in Medicare until the employment ends or the coverage stops (whichever happens first), without incurring any late penalties if you enroll later. When the employer-tied coverage ends, you’re entitled to a special enrollment period of up to eight months to sign up for Medicare.
What happens if you don't sign up for Medicare?
Therefore, if you fail to sign up for Medicare when required, you will essentially be left with no coverage. It’s therefore extremely important to ask the employer whether you are required to sign up for Medicare when you turn 65 or receive Medicare on the basis of disability.
Can you sell a Medigap policy?
Insurance companies are prohibited from refusing to sell you a Medigap policy or charge higher premiums based on your health or preexisting medical conditions, if you buy the policy within six months of enrolling in Part B. Outside of that six-month window, except in very limited circumstances, they can do both.
Can you delay Medicare enrollment?
You can’t delay Medicare enrollment without penalty if your employer-sponsored coverage comes from retiree benefits or COBRA — by definition, these do not count as active employment. Nor does it count if you work beyond 65 but rely on retiree benefits from a former employer.
How long does Medicare enrollment last?
The general rule for Medicare signup is that unless you meet an exception, you get a seven-month enrollment window that starts three months before your 65th birthday month and ends three months after it. Having qualifying insurance through your employer is one of those exceptions. Here’s what to know.
How much is the penalty for Part D?
For Part D, the penalty is 1% of the base premium ($33.06 in 2021) multiplied by the number of full, uncovered months you didn’t have Part D or creditable coverage.
Who is Elizabeth Gavino?
“I find it is always good to just confirm,” said Elizabeth Gavino, founder of Lewin & Gavino and an independent broker and general agent for Medicare plans.
Does Medicare have a premium?
Part A has no premium as long as you have at least a 10-year work history of contributing to the program through payroll (or self-employment) taxes.
Do you have to sign up for Medicare at age 65?
Medicare may not be top of mind if you’re nearing the eligibility age of 65 and already have health insurance through your employer. However, it probably deserves some attention. While not everyone must sign up, many are required to enroll unless they want to face life-lasting late-enrollment penalties.
What happens if you don't have Part B insurance?
If you don’t, your employer’s group plan can refuse to pay your claims. Your insurance might cover claims even if you don’t have Part B, but we always recommend enrolling in Part B. Your carrier can change that at any time, with no warning, leaving you responsible for outpatient costs.
What is CMS L564?
You will need your employer to fill out the CMS-L564 form. This form is a request for employment information form. Once the employer completes section B of the form, you can send in the document with your application to enroll in Medicare.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
Can employers contribute to Medicare premiums?
Medicare Premiums and Employer Contributions. Per CMS, it’s illegal for employers to contribute to Medica re premiums. The exception is employers who set up a 105 Reimbursement Plan for all employees. The reimbursement plan deducts money from the employees’ salaries to buy individual insurance policies.
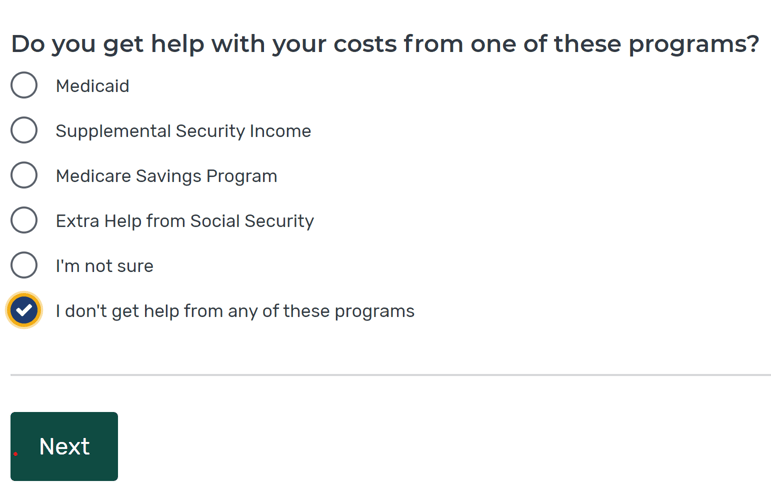
Is Part B premium free?
Since Part B is not premium-free like Part A is for most, you may wish to delay enrollment if you have group insurance. As stated above, the size of your employer determines whether your coverage will be considered creditable once you retire and are ready to enroll. Group coverage for employers with 20 or more employees is deemed creditable ...
Is Medicare billed first or second?
If your employer has fewer than 20 employees, then Medicare becomes primary. This means Medicare is billed first, and your employer plan will be billed second. If you have small group insurance, it’s HIGHLY recommended that you enroll in both Parts A and B as soon as you’re eligible. If you don’t, your employer’s group plan can refuse ...