What is Medicare and is it mandatory?
Is Medicare mandatory? Medicare is a federal benefit that you pay for through taxes during your working years. At age 65, or if you have certain disabilities, you become eligible for health coverage through various parts of the Medicare program.
When does Medicare start at age 65?
If you sign up during one of the months before your 65th birthday, your coverage will begin on the first day of the month you turn 65 (or one month before your birthday if you were born on the first day of the month). Is Medicare Free at Age 65?
What is the initial enrollment period for Medicare?
Those are the first three months of your seven-month Initial Enrollment Period. Unless your birthday is on the first day of the month, your Initial Enrollment Period includes the three full months before turning 65, the month you turn 65, and the three months after you turn 65.
What are the health and safety standards of CMS?
These health and safety standards are the foundation for improving quality and protecting the health and safety of beneficiaries. CMS also ensures that the standards of accrediting organizations recognized by CMS (through a process called "deeming") meet or exceed the Medicare standards set forth in the CoPs / CfCs.
When did Medicare require EMR?
As a part of the American Recovery and Reinvestment Act, all public and private healthcare providers and other eligible professionals (EP) were required to adopt and demonstrate “meaningful use” of electronic medical records (EMR) by January 1, 2014 in order to maintain their existing Medicaid and Medicare ...
When did CMS require EHR?
2011In 2011, CMS established the Medicare and Medicaid EHR Incentive Programs (now known as the Medicare Promoting Interoperability Program) to encourage EPs, eligible hospitals, and CAHs to adopt, implement, upgrade, and demonstrate meaningful use of certified electronic health record technology (CEHRT).
In what year did Medicare begin payments to providers for implementation of EHR?
2011EHR Incentive Payments for Eligible Professionals The program started in 2011, and payments continued under Medicare through 2016 with no Medicare incentive payments available after 2016 pursuant to the statute.
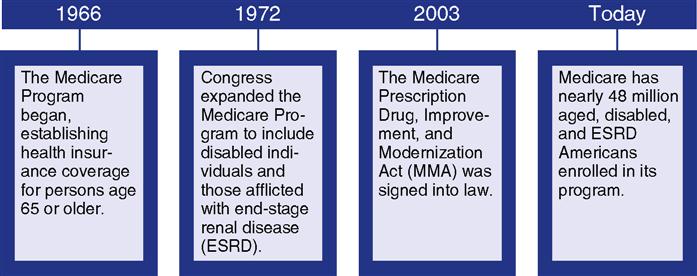
What did the Medicare Act of 1965 do?
On July 30, 1965, President Lyndon B. Johnson signed the Medicare and Medicaid Act, also known as the Social Security Amendments of 1965, into law. It established Medicare, a health insurance program for the elderly, and Medicaid, a health insurance program for people with limited income.
When did CMS start meaningful use?
2011Meaningful Use: Overview The program, which began in 2011, evolved over the course of 3 stages: Stage 1 established the base requirements for electronic capturing of clinical data.
When was meaningful use implemented?
2009The U.S. government introduced the Meaningful Use program as part of the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act, to encourage health care providers to show "meaningful use" of a certified Electronic Health Record (EHR).
Who has mandated the implementation of electronic health records?
President Bush made mention of the topic in his 2004 State of the Union address [2], and President Obama incorporated EHR into his American Recovery and Reinvestment Act of 2009 as part of the Health Information Technology for Economic and Clinical Health Act (HITECH).
Which federal act mandated that physicians use the health information exchange HIE?
In the US, the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 provided $564 million for establishment of HIE by states or state-designated entities [8].
Which of the following was established by the federal government to assist with the transition to electronic health records?
In 2009 as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act, the federal government set aside $27 billion for an incentive program that encourages hospitals and providers to adopt electronic health records systems (EHR).
When did Part D become mandatory?
Medicare Part D Prescription Drug benefit The MMA also expanded Medicare to include an optional prescription drug benefit, “Part D,” which went into effect in 2006.
When did Medicare supplement plans became standardized?
Medicare SELECT was authorized by OBRA-1990 as a 15-State demonstration and became a national program in 1995.
What was Medicare in the 1960s?
In 1965, the budget for Medicare was around $10 billion. In 1966, Medicare's coverage took effect, as Americans age 65 and older were enrolled in Part A and millions of other seniors signed up for Part B. Nineteen million individuals signed up for Medicare during its first year.
Do I Automatically Get Medicare When I Turn 65?
Some people automatically get Medicare at age 65, but those numbers have declined as the Medicare and Social Security ages have continued to drift...
What if I’m Not Automatically Enrolled at 65?
If your Medicare enrollment at 65 is not automatic, but you want to enroll, here are some more magic numbers.
Is Medicare Free at Age 65?
While Medicare Part B has a standard monthly premium, 99 out of 100 people don’t have to pay a premium for Medicare Part A. Still, no part of Medic...
How Much Does Medicare Cost at Age 65?
The standard premium for Part B modestly increases year over year. Part A costs also can increase, including the annual deductible and other coinsu...
Can You Get on Medicare at Age 62?
No, but while the standard age of eligibility remains 65, some call for lowering it. In a recent GoHealth survey, among respondents age 55 and olde...
Can a 55-Year-Old Get Medicare?
While 65 has always been Medicare’s magic number, there are a few situations where the Medicare age limit doesn’t apply, and you may be able to get...
Key Takeaways
The standard age for Medicare eligibility has been 65 for the entirety of the health insurance program, which debuted in 1965.
Medicare Eligibility Age Chart
Most older adults are familiar with Medicare and its eligibility age of 65. Medicare Part A and Medicare Part B are available based on age or, in some cases, health conditions, including:
Do I Automatically Get Medicare When I Turn 65?
Some people automatically get Medicare at age 65, but those numbers have declined as the Medicare and Social Security ages have continued to drift apart.
Is Medicare Free at Age 65?
While Medicare Part B has a standard monthly premium, 99 out of 100 people don’t have to pay a premium for Medicare Part A. Still, no part of Medicare can genuinely be called “free” because of associated costs you have to pay, like deductibles, coinsurance and copays.
Can You Get on Medicare at Age 62?
No, but while the standard age of eligibility remains 65, some call for lowering it. In a recent GoHealth survey, among respondents age 55 and older who weren’t on Medicare and had heard about proposals to lower the age of eligibility, 64% favored lowering the age.
Full Retirement Age by Year - What to Know
Full retirement age is the age you begin to receive full Social Security benefits. If you start to draw your Social Security benefits before reaching your full retirement age, the payment you receive will be less.
Answer a few questions to find out
These questions don’t apply if you have End-Stage Renal Disease (ESRD).
Do you have health insurance now?
Are you or your spouse still working for the employer that provides your health insurance coverage?
Your first chance to sign up (Initial Enrollment Period)
Generally, when you turn 65. This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65.
Between January 1-March 31 each year (General Enrollment Period)
You can sign up between January 1-March 31 each year. This is called the General Enrollment Period. Your coverage starts July 1. You might pay a monthly late enrollment penalty, if you don’t qualify for a Special Enrollment Period.
Special Situations (Special Enrollment Period)
There are certain situations when you can sign up for Part B (and Premium-Part A) during a Special Enrollment Period without paying a late enrollment penalty. A Special Enrollment Period is only available for a limited time.
Joining a plan
A type of Medicare-approved health plan from a private company that you can choose to cover most of your Part A and Part B benefits instead of Original Medicare. It usually also includes drug coverage (Part D).
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
Many errors reported in Medicare audits are due to claims submitted with incomplete or missing requisite documentation.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is a CfC in Medicare?
CMS develops Conditions of Participation (CoPs) and Conditions for Coverage (CfCs) that health care organizations must meet in order to begin and continue participating in the Medicare and Medicaid programs. These health and safety standards are the foundation for improving quality and protecting the health and safety of beneficiaries. CMS also ensures that the standards of accrediting organizations recognized by CMS (through a process called "deeming") meet or exceed the Medicare standards set forth in the CoPs / CfCs.
What is the purpose of health and safety standards?
These health and safety standards are the foundation for improving quality and protecting the health and safety of beneficiaries. CMS also ensures that the standards of accrediting organizations recognized by CMS (through a process called "deeming") meet or exceed the Medicare standards set forth in the CoPs / CfCs.