
Full coverage Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Full Answer
What medications are not covered by Medicare?
Some examples of medications that may not be covered by Medicare include: Weight loss or weight gain medications Medications used to treat cold or cough symptoms Fertility medications Vitamins and minerals (with the exception of prenatal vitamins or fluoride preparation products) Medications used ...
What does Medicare cover and what can you claim?
Under Medicare you can be treated as a public patient in a public hospital, at no charge. Medicare will also cover some or all the costs of seeing a GP or specialist outside of hospital, and some pharmaceuticals.
What does a Medicare supplement really cover?
Medicare supplement plans don't work like most health insurance plans. They don't actually cover any health benefits. Instead, these plans cover the costs you're responsible for with Original Medicare. These costs can include: Your Medicare deductibles ; Your coinsurance ; Hospital costs after you run out of Medicare-covered days
Who decides what Medicare or Medicaid covers?
What Medicare covers may be based on several factors, like: • Federal laws describing Medicare benefits, or state laws that tell what services a particular type of practitioner is licensed to provide. • National coverage decisions made by Medicare about whether a particular item or service is covered nationally under Medicare’s rules.

Do Medicaid and Medicare cover the same things?
Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second. Medicaid never pays first for services covered by Medicare. It only pays after Medicare, employer group health plans, and/or Medicare Supplement (Medigap) Insurance have paid.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
When a patient is covered through Medicare and Medicaid which coverage is primary?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors' visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
Does Medicaid cover surgery?
Medicaid does cover surgery as long as the procedure is ordered by a Medicaid-approved physician and is deemed medically necessary. Additionally, the facility providing the surgery must be approved by Medicaid barring emergency surgery to preserve life.
Is Medicare better than Medicaid?
Coverage. In general, Medicaid is a more comprehensive health insurance policy. Original Medicare, which includes Part A and B, has many gaps in coverage that can be filled if you are willing to purchase additional Medicare plans such as Part D or Medicare Advantage.
How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
Does Medicare cover 100 percent of hospital bills?
Medicare generally covers 100% of your medical expenses if you are admitted as a public patient in a public hospital. As a public patient, you generally won't be able to choose your own doctor or choose the day that you are admitted to hospital.
Do I need Medicare Part B if I have Medicaid?
Once you become dual-eligible, most – if not all – of your healthcare costs will be covered. Thus, you are not eligible to enroll in a Medicare Supplement plan. Medicaid covers your Medicare Part A premium (if applicable) and the standard Medicare Part B premium for all eligible enrollees.
What are Medicaid requirements?
Medicaid beneficiaries generally must be residents of the state in which they are receiving Medicaid. They must be either citizens of the United States or certain qualified non-citizens, such as lawful permanent residents. In addition, some eligibility groups are limited by age, or by pregnancy or parenting status.
Does Social Security count as income for Medi-Cal?
Most Social Security disability and retirement income does count as income for purposes of Medicaid eligibility. The income figure used to decide whether you are eligible for Medicaid is known as modified adjusted gross income, or MAGI.
Does Medicare coverage start the month you turn 65?
The date your coverage starts depends on which month you sign up during your Initial Enrollment Period. Coverage always starts on the first of the month. If you qualify for Premium-free Part A: Your Part A coverage starts the month you turn 65.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
Does Medicaid cover cost sharing?
If you are enrolled in QMB, you do not pay Medicare cost-sharing, which includes deductibles, coinsurances, and copays.
Does Medicare cover medicaid?
If you qualify for a Medicaid program, it may help pay for costs and services that Medicare does not cover.
Is medicaid the primary or secondary insurance?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors’ visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
Does Medicaid offer care coordination?
Medicaid can offer care coordination: Some states require certain Medicaid beneficiaries to enroll in Medicaid private health plans, also known as Medicaid Managed Care (MMC) plans. These plans may offer optional enrollment into a Medicare Advantage Plan designed to better coordinate Medicare and Medicaid benefits.
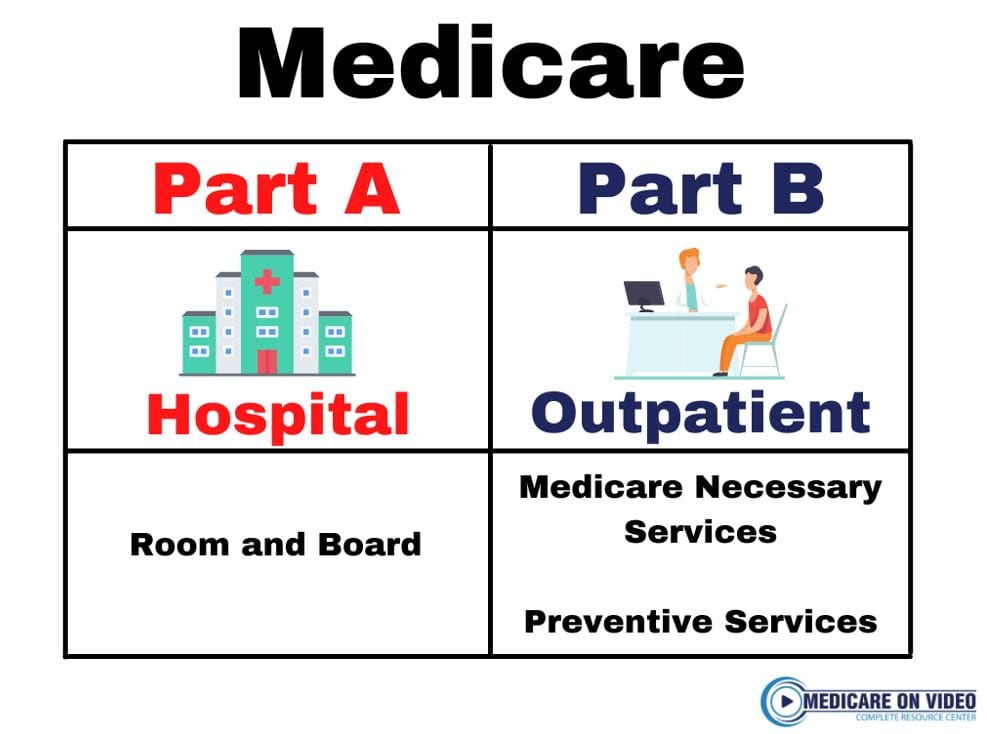
What is Medicare Part A?
Under Medicare Part A, hospital care as well as some nursing home, rehabilitation, mental health, and hospice care are generally covered. However, you may have to meet certain qualifications. Inpatient hospital care. Medicare Part A covers general nursing services, a semi-private room, meals, medical supplies, and certain medications.
What are the different parts of Medicare?
Here’s a quick rundown of the “parts” of Medicare, and the choices you may have about your Medicare coverage. Medicare Part A and Part B make up Original Medicare. Many people are automatically enrolled in Part A and Part B. You may be automatically enrolled if you’re receiving Social Security retirement or disability benefits when you qualify ...
What is skilled nursing in Medicare?
Skilled nursing facility care. Medicare covers room, board, and a range of skilled nursing services provided in a skilled nursing facility . This may include certain medications, tube feedings, and wound care, among other approved services.
How many days of home health care is covered by Medicare?
Medicare covers up to 100 days of part-time daily care or intermittent care if medically necessary. You must have spent at least three consecutive days as a hospital inpatient within 14 days of receiving home health care. If you don’t qualify for home health care coverage under Part A, you might have Medicare coverage under Part B.
What is medically necessary?
Medically necessary services you receive from a doctor or other licensed health professional. This includes some preventive care services, such as annual wellness exams, flu shots, and screens to help detect certain forms of cancer. Durable medical equipment such as walkers, wheelchairs, and oxygen tanks.
What medical equipment do you need to be a doctor?
Durable medical equipment such as walkers, wheelchairs, and oxygen tanks. This is medical equipment your doctor certifies you need that you use repeatedly and typically at home. You generally rent or purchase durable medical equipment from a Medicare-certified supplier. Diagnostic tests such as lab work and x-rays.
Does Medicare Advantage cover prescription drugs?
Medicare Advantage plans must offer you at least the same level of Medicare coverage as Part A and Part B. Frequently, Medicare Advantage plans combine Medicare coverage for prescription drugs along with medical benefits. Some Medicare Advantage plans offer additional benefits to standard Medicare coverage.
Medicare Advantage (Part C)
You pay for services as you get them. When you get a covered service, Medicare pays part of the cost and you pay your share.
You can add
You join a Medicare-approved plan from a private company that offers an alternative to Original Medicare for your health and drug coverage.
Most plans include
Some extra benefits (that Original Medicare doesn’t cover – like vision, hearing, and dental services)
Medicare drug coverage (Part D)
If you chose Original Medicare and want to add drug coverage, you can join a separate Medicare drug plan. Medicare drug coverage is optional. It’s available to everyone with Medicare.
Medicare Supplement Insurance (Medigap)
Medicare Supplement Insurance (Medigap) is extra insurance you can buy from a private company that helps pay your share of costs in Original Medicare.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
Does Medicaid cover nursing home care?
Medicaid also pays for nursing home care, and often limited personal care assistance in one’s home. While some states offer long-term care and supports in the home and community thorough their state Medicaid program, many states offer these supports via 1915 (c) Medicaid waivers.
What does Medicare cover?
Funded by the federal government, Medicare is our nation’s health insurance program for seniors, certain younger people with disabilities and people with end-stage renal disease.
How does Medicare work?
You become eligible for Medicare when you turn 65. You’re initially enrolled in Original Medicare unless you choose Medicare Advantage.
How has Medicare changed over the years?
Original Medicare started in 1965. There have been numerous changes to offerings, benefits and costs over the years.
What does Medicare Part A cover and not cover?
Part A covers inpatient hospital, hospice and home health care. And it helps pay a stay in a skilled nursing facility like a nursing home for up to 100 days.
What does Medicare Part B cover and not cover?
Part B pays for doctor visits, lab tests, diagnostic screening, mental health, outpatient care at hospitals and clinics, emergency care, durable medical equipment and associated expenses. But first, you have to pay a $203 annual deductible before Medicare starts paying for care.
What does Medicare Part C (Medicare Advantage) cover and not cover?
Not everyone chooses to get their Medicare through Original Medicare. Vasta says one in every three people eligible for Medicare enrolls instead in Medicare Advantage plans, offered through private insurance carriers.
What does Medicare Part D cover and not cover?
Part D, a prescription drug plan, is available separately if you’re enrolled in Parts A and/or B. Part D plans are provided via private companies.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is a health care provider?
Tell your doctor and other. health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. about any changes in your insurance or coverage when you get care.
What does Medicare cover?
Medicare coverage: what costs does Original Medicare cover? Here’s a look at the health-care costs that Original Medicare (Part A and Part B) may cover. If you’re an inpatient in the hospital: Part A (hospital insurance) typically covers health-care costs such as your care and medical services. You’ll usually need to pay a deductible ($1,484 per ...
What type of insurance is used for Medicare Part A and B?
This type of insurance works alongside your Original Medicare coverage. Medicare Supplement insurance plans typically help pay for your Medicare Part A and Part B out-of-pocket costs, such as deductibles, coinsurance, and copayments.
How much does Medicare Supplement pay for hospital visits?
(Under Medicare Supplement Plan N, you might have to pay a copayment up to $20 for some office visits, and up to $50 for emergency room visits if they don’t result in hospital admission.)
What does Part B cover?
Part B typically covers certain disease and cancer screenings for diseases. Part B may also help pay for certain medical equipment and supplies.
Does Medicare have a maximum spending limit?
Be aware that Original Medicare has no annual out-of-pocket maximum spending limit. If you meet your Medicare Part A and/or Part B deductibles, you still generally pay a coinsurance or copayment amount – and there’s no limit to what you might pay in a year.
Does Medicare Advantage work?
To answer that question, here’s a quick rundown on how the Medicare Advantage (Medicare Part C) program works. When you have a Medicare Advantage plan, you still have Medicare – but you get your Medicare Part A and Part B benefits through the plan, instead of directly from the government.
Does Medicare cover out of pocket expenses?
Unlike Original Medicare, Medicare Advantage plans have annual out-of-pocket spending limits. So, if your Medicare-approved health -care costs reach a certain amount within a calendar year, your Medicare Advantage plan may cover your approved health-care costs for the rest of the year. The table below compares health-care costs ...
Health
- Heres a quick overview of Medicare and what it covers. Original Medicare is the health insurance program created and administered by the federal government.
Services
- Medicare Part A generally covers medically necessary services such as: Medicare Part B generally covers the following services:
Content
- Before going into what Medicare Part C covers, heres a quick rundown on what Part C is. Medicare Part C, commonly known as Medicare Advantage, provides an alternative way to receive your Original Medicare (Part A and Part B) coverage. Medicare Advantage plans are offered by private insurance companies that have contracts with Medicare. So, Medicare Advantage plans …
Benefits
- Many Medicare Advantage plans cover prescription drugs. They may include additional benefits, such as routine vision, hearing, and dental services. Not every Medicare Advantage plan covers prescription medications, but the ones that do are called Medicare Advantage Prescription Drug plans (sometimes abbreviated as MA-PDs). If you enroll in a Medica...
Definition
- Medicare Part D covers prescription drugs through private insurance companies contracted with Medicare. Medicare Part D prescription drug coverage is available not only from Medicare Advantage Prescription Drug plans (described above), but also from stand-alone Medicare Part D Prescription Drug Plans.
Use
- Each Medicare Prescription Drug Plan has a formulary, which is a list of prescription medications covered by that plan. Formularies include medications from all the therapeutic drug categories and typically include brand name and generic prescription drugs. Formularies and costs vary by plan, so it may be a good idea to compare the plans available where you live to identify the one t…
Cost
- If you enroll in a Medicare Prescription Drug Plan, you may have to pay a monthly premium in addition to your Medicare Part B coverage. You may be able to buy a Medicare Supplement (Medigap) plan to help pay for Medicare Part A and Part B out-of-pocket costs. Different Medicare Supplement plans pay for different amounts of those costs, such as copayments, coinsurance, a…
Scope
- While Medicare covers many medical services, it doesnt cover everything. You may be surprised to learn that Original Medicare (Part A and Part B) doesnt cover long-term care when the focus is on daily living activities (custodial care) rather than skilled care. Here are some examples of services and items Original Medicare doesnt typically cover: