How to find best Medicare supplement insurance?
Best for Comparison Shopping. United Medicare Advisors is an online marketplace that lets you search for Medicare Supplement Insurance quotes from multiple companies. By entering your address, zip code, and phone number, you can view policy rates from companies like Cigna, Aetna, and Mutual of Omaha, among others.
What is the best and cheapest Medicare supplement insurance?
The Medicare Supplement Plan N is best for the following people:
- People looking for complete coverage at a modest monthly rate
- Those who don’t mind paying a minor fee at the time of service
- People who are not subject to Part B excess charges
What are the top 5 Medicare supplement plans?
- Plan G
- Plan N
- Plan A
- Plan F
- High Deductible Plan F
Does my supplemental insurance cover what Medicare does not?
Medicare supplement plans don't work like most health insurance plans. They don't actually cover any health benefits. Instead, these plans cover the costs you're responsible for with Original Medicare. These costs can include: Your Medicare deductibles. Your coinsurance. Hospital costs after you run out of Medicare-covered days.

What is the cost of supplemental insurance for Medicare?
In 2020, the average premium for Medicare supplemental insurance, or Medigap, was approximately $150 per month or $1,800 per year, according to Senior Market Sales, a full-service insurance organization.
What is the common name for supplemental Medicare insurance?
(Medigap)Medicare Supplement Insurance (Medigap) is extra insurance you can buy from a private company that helps pay your share of costs.
Which Medicare Supplement plan has the highest level of coverage?
Plan FPlan F premiums are usually the highest of all Medicare Supplement plans. This makes sense because it offers the highest level of coverage. Medicare Supplement costs vary based on a number of factors, including your age, sex, smoking status, and even your ZIP code.
Who is the largest Medicare Supplement provider?
UnitedHealthCareAARP/United Health Group has the largest number of Medicare Supplement customers in the country, covering 43 million people in all 50 states and most U.S. territories. AARP licenses its name to insurer UnitedHealthCare, which helps make these policies so popular.
Who has the cheapest Medicare supplement insurance?
What's the least expensive Medicare Supplement plan? Plan K is the cheapest Medigap plan, with an average cost of $77 per month for 2022.
What are the top 3 most popular Medicare Supplement plans in 2021?
Three Popular Medicare Supplement PlansBlue Cross Blue Shield. According to Blue Cross Blue Shield (BCBS), Plans F and N are available in most areas. ... AARP United Healthcare. The United Healthcare Medicare Supplement plan is also very popular. ... Humana.
What is the average cost of AARP Medicare supplement insurance?
1. AARP Medigap costs in states where age doesn't affect the pricePlan nameAverage monthly cost for AARP MedigapPlan A$158Plan B$242Plan C$288Plan F$2566 more rows•Jan 24, 2022
What is the difference between plan G and plan N?
This is where the differences between Plan G and N start. Plan G covers 100% of all Medicare-covered expenses once your Part B deductible has been met for the year. Medicare Plan N coverage, on the other hand, has a few additional out-of-pocket expenses you will have to pay, which we'll cover next.
What is the deductible for plan G in 2022?
$2,490Effective January 1, 2022, the annual deductible amount for these three plans is $2,490. The deductible amount for the high deductible version of plans G, F and J represents the annual out-of-pocket expenses (excluding premiums) that a beneficiary must pay before these policies begin paying benefits.
What is the difference between a Medicare Advantage plan and a Medicare Supplement plan?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
What company has the best Medicare coverage?
Best Medicare Advantage Providers RatingsProviderForbes Health RatingsCoverage areaBlue Cross Blue Shield5.0Offers plans in 48 statesCigna4.5Offers plans in 26 states and Washington, D.C.United Healthcare4.0Offers plans in all 50 statesAetna3.5Offers plans in 44 states1 more row•Jun 8, 2022
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
Can you cancel a Medigap policy?
This means the insurance company can't cancel your Medigap policy as long as you pay the premium. Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
How to choose a Medigap plan?
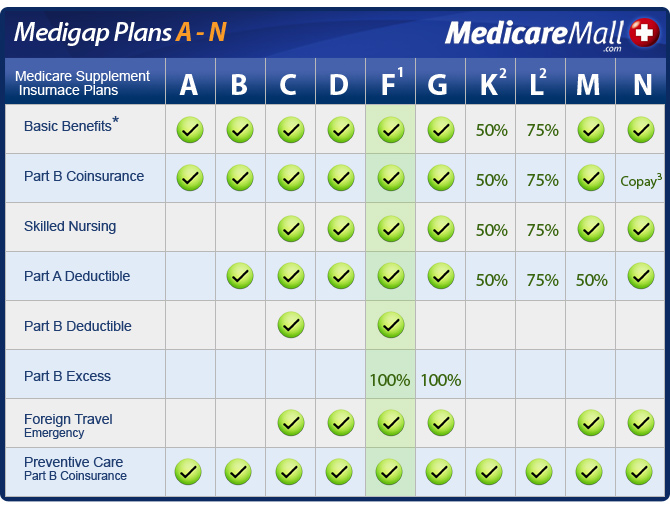
Medigap policies are standardized, and in most states are named by letters, Plans A-N. Compare the benefits each plan helps pay for and choose a plan that covers what you need. See benefits of each plan. Step 2.
What is Medigap insurance?
Medicare Supplement Insurance (Medigap) is extra insurance you can buy from a private company that helps pay your share of costs.
What is Medicare Supplement Insurance?
Medicare Supplement insurance is meant to limit unpleasant surprises from healthcare costs. Your health at age 65 may be no indicator of what’s to come just a few years later. You could get sick and face medical bills that devastate years of planning and preparation. Combine this with the fixed income that so many seniors find themselves on, ...
How much does Medicare Supplement cover?
Choosing Medicare Supplement insurance can help. It can cover up to 100% of out-of-pocket costs, depending on the plan. One out of every three Original Medicare beneficiaries — over 13 million seniors — have chosen to do so. 1.
How long is the open enrollment period for Medicare?
The Medigap Open Enrollment Period covers six months. It starts the month you are 65 or older and are enrolled in Medicare Part B. In this period, no insurer offering supplemental insurance in your state can deny you coverage or raise the premium because of medical conditions.
How many separate insurance plans are there?
Premiums for the same policy can vary between insurance companies. But, only the quoted price and the reputation of the insurer will vary. There are ten separate plans, labeled A through N. Two plans, C and F, are no longer offered to newly eligible beneficiaries.
Does Medicare Supplement cover all costs?
Original Medicare does not cover all costs. Medicare Supplement insurance, or Medigap, can cover what Medicare does not. Private insurance companies – vetted by the federal government – offer it to help manage out-of-pocket expenses. These policies do not add coverage.
Can you renew a Medigap policy?
You can renew your Medigap policy as long as you pay the premium. The insurer cannot use your health problems to cancel your policy or raise your premium.
Does Medicare Part C have a referral requirement?
Original Medicare allows you to see any doctor in the U.S. who accepts Medicare. It provides excellent flexibility: it has no networks or referral requirements. Medicare Part C (or Medicare Advantage) bundles hospital, doctor and drug coverage.
Do I Need a Medigap Plan?
If you have a Medicare Advantage (Part C) plan, you do not need to go any further. Medigap plans do not work with Medicare Advantage plans. In fact, it is illegal for an insurance company to see you a Medigap plan if you have Part C.
Important Facts to Know about Medigap Plans
There are some things common to all Medigap plans. The most important are these:
How Does a Medigap Plan Work?
In most policies, part of the agreement you will sign allows the Medigap carrier to receive your Medicare claim after the primary carrier processes it. This is sometimes known as “piggyback” coverage.
Best Time to Purchase a Policy
When you enroll in Original Medicare Part A and B, you have an automatic six-month open enrollment period. During this window, you may purchase any Medigap policy sold in your state, no matter what your health situation is. These are known as “guaranteed issue rights.”
Basic Comparison of Plans
There are thousands of Medicare Supplemental Insurance plans available in every state. With this many choices, you might wonder where to start.
Start Your Comparison Search
Medicare’s website has a good tool to start your search. Input your zip code and whether you already have a policy and click “continue.” You can also include your health status, but that’s not necessary at this point.
A Note Regarding Pricing Methods
In the middle of this screen is a column called “Pricing Method.” This is how each insurance company sets its own premiums. This method can greatly influence the pricing of their policies. There are three rating systems:
Why Do I Need Supplemental Insurance If I Have Medicare?
If you look at the Medicare website, they list out what you could owe out of pocket for needing care. You may be responsible for some sizable deductibles, co-payments and coinsurance costs.
How Do I Choose Medicare Supplement Insurance?
Insurance companies label Medigap plans with a letter (A through N) to show what benefits are included. For example, according to Medicare.gov, Medigap Plan F will pay for health care during foreign travel but Plan A will not.
Who Is Eligible for Supplemental Insurance?
Anyone who has Medicare Part A and Part B is eligible to apply for a Medicare supplement plan. However, you need to qualify for coverage with the private insurance company. When you first turn 65 and sign up for Medicare Part B, you have a Medigap open enrollment period that lasts six months.
Are There Any Other Considerations?
To keep your Medicare supplemental insurance coverage, you need to pay premiums throughout the year. This is an additional cost during retirement. If you don't end up needing treatment, it's possible you could pay more in premiums than the value you'd get from the policy, similar to any health insurance program.
Are There Alternative Insurance Programs?
Besides Medigap, you could also cover your retirement health insurance costs through a Medicare Advantage plan. Medicare Advantage is private health insurance. Through this program, you would leave traditional Medicare and instead have the private insurer pay for your health care bills.
The Bottom Line
As you figure out how to manage your retirement health care coverage, consider speaking with a financial representative. They can help you determine the next steps for managing health care costs in retirement.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is Medicare Advantage?
Medicare covers medical services and supplies in hospitals, doctors’ offices, and other health care settings. Services are either covered under Part A or Part B. Coverage in Medicare Advantage. Plans must cover all of the services that Original Medicare covers.
Does Medicare Advantage have a yearly limit?
If you join a Medicare Advantage Plan, once you reach a certain limit, you’ll pay nothing for covered services for the rest of the year. This option may be more cost effective for you. note:
Is coinsurance a part of Medicare Advantage?
Supplemental coverage in Medicare Advantage. It may be more cost effective for you to join a Medicare Advantage Plan because your cost sharing is lower (or included). And, many Medicare Advantage plans offer vision, hearing, and dental.
Can you use a Medigap policy?
You can’t use (and can’t be sold) a Medigap policy if you’re in a Medicare Advantage Plan. note: If you're in a Medicare plan, review the "Evidence of Coverage" (EOC)and "Annual Notice of Change" (ANOC) . Prescription drugs.
Does Medicare cover hearing?
Some plans offer benefits that Original Medicare doesn’t cover like vision, hearing, or dental. note: If you're in a Medicare plan, review the "Evidence of Coverage" (EOC)and "Annual Notice of Change" (ANOC) . Your other coverage.
Does Medicare Advantage include prescription drugs?
Most Medicare Advantage Plans include drug coverage. If yours doesn't, you may be able to join a separate Part D plan. note: If you're in a Medicare plan, review the "Evidence of Coverage" (EOC)and "Annual Notice of Change" (ANOC) . Doctor and hospital choice.
