What is considered a grievance in Medicare?
A grievance is an expression of dissatisfaction (other than an organization determination) with any aspect of the operations, activities, or behavior of a Medicare health plan, or its providers, regardless of whether remedial action is requested.
How can Medicare problems be resolved?
Your plan is the best resource to resolve plan related issues. Call 1-800-MEDICARE. Call 1-800-633-4227, TTY users should call 1-877-486-2048. If your concern is related to Original Medicare, or if your plan was unable to resolve your inquiry, contact 1-800-MEDICARE for help.
How do I report to CMS?
Reporting FraudBy Phone. Health & Human Services Office of the Inspector General. 1-800-HHS-TIPS. (1-800-447-8477) ... Online. Health & Human Services Office of the Inspector General Website.By Fax. Maximum of 10 pages. 1-800-223-8164.By Mail. Office of Inspector General. ATTN: OIG HOTLINE OPERATIONS. P.O. Box 23489.
Is an appeal and grievance the same?
Grievance: Concerns that do not involve an initial determination (i.e. Accessibility/Timeliness of appointments, Quality of Service, MA Staff, etc.) Appeal: Written disputes or concerns about initial determinations; primarily concerns related to denial of services or payment for services.
What is a Medicare ombudsman?
The Medicare Beneficiary Ombudsman helps you with complaints, grievances, and information requests about Medicare. They make sure information is available to help you: Make health care decisions that are right for you. Understand your Medicare rights and protections. Get your Medicare issues resolved.
How do I ask Medicare a question?
Call 1-800-MEDICARE For questions about your claims or other personal Medicare information, log into (or create) your secure Medicare account, or call us at 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
Which is an example of Medicare abuse?
One example of Medicare abuse is when a doctor makes a mistake on a billing invoice and inadvertently asks for a non-deserved reimbursement. Medicare waste involves the overutilization of services that results in unnecessary costs to Medicare.
What is the purpose of CMS reporting?
The purpose of Section 111 reporting is to enable CMS to pay appropriately for Medicare-covered items and services furnished to Medicare beneficiaries.
What are CMS penalties?
A CMP is a monetary penalty the Centers for Medicare & Medicaid Services (CMS) may impose against nursing homes for either the number of days or for each instance a nursing home is not in substantial compliance with one or more Medicare and Medicaid participation requirements for long-term care facilities.
What should a grievance appeal include?
In an appeal hearing, the person carrying out the appeal process should:introduce everyone, explaining why they are there if necessary.explain the purpose of the meeting, how it will be conducted and what powers the person hearing the appeal has.ask you why you are appealing.look at new evidence, if there is any.More items...
What is a grievance from insurance?
A grievance is an expression of dissatisfaction (other than a coverage determination) with any aspect of the operations, activities, or behavior of a Part D plan sponsor, regardless of whether remedial action is requested.
What is the purpose of a grievance appeal hearing?
Within the grievance appeal hearing you will be doing one of two things; reviewing the decision previously made or re-hearing the employee's complaint. More on these later, but for now make sure there's sufficient time in your diary to do either.
What are grievances in healthcare?
Examples of grievance include: 1 Problems getting an appointment, or having to wait a long time for an appointment 2 Disrespectful or rude behavior by doctors, nurses or other plan clinic or hospital staff
What are some examples of grievances?
Examples of grievance include: Problems getting an appointment, or having to wait a long time for an appointment. Disrespectful or rude behavior by doctors, nurses or other plan clinic or hospital staff.
What is the role of each Medicare plan?
Each plan must provide meaningful procedures for timely resolution of both standard and expedited grievances between enrollees and the Medicare health plan or any other entity or individual through which the Medicare health plan provides health care services.
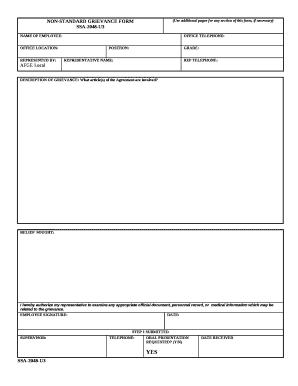
How to file a grievance with Medicare?
To file a grievance, send a letter to your plan’s Grievance and Appeals department. Check your plan’s website or contact them by phone for the address. You can also file a grievance with your plan over the phone, but it is best to send your complaints in writing. Be sure to send your grievance to your plan within 60 days of the event that led to the grievance. You may also want to send a copy of the grievance to your regional Medicare office and to your representatives in Congress, if you feel they should know about the problem. Go to www.medicare.gov or call 1-800-MEDICARE to find out the address of your regional Medicare office. Keep a copy of any correspondence for your records.
What to do if you are dissatisfied with Medicare Advantage?
Register. If you are dissatisfied with your Medicare Advantage or Part D prescription drug plan for any reason, you can choose to file a grievance. A grievance is a formal complaint that you file with your plan. It is not an appeal, which is a request for your plan to cover a service or item it has denied.
How long does it take for a medical plan to get back to you?
Your plan must investigate your grievance and get back to you within 30 days. If your request is urgent, your plan must get back to you within 24 hours. If you have not heard back from your plan within this time, you can check the status of your grievance by calling your plan or 1-800-MEDICARE.
Complaints about the quality of your care
Contact your Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) for complaints about the quality of care you got from a Medicare provider.
note
For questions about a specific service you got, look at your Medicare Summary Notice (MSN) or log into your secure Medicare account . You can file an appeal if you disagree with a coverage or payment decision made by one of these:
How long does it take to file a grievance with a health insurance company?
Grievances must be filed with the plan sponsor no later than 60 days after the event or incident that brought about the grievance.
How long does a health insurance plan have to notify the enrollee of a grievance?
The plan sponsor must notify the enrollee of its decision as expeditiously as the enrollee's health requires, but no later than 30 days after the date the plan sponsor receives the grievance, unless in the best interest of the enrollee the timeframe is extended by the plan sponsor for up to 14 calendar days.
What is a grievance in Part D?
The grievance involves a refusal by the Part D plan sponsor to grant an enrollee's request for an expedited coverage determination or expedited redetermination, and
How long does it take to respond to a grievance?
However, the plan must respond to a grievance within 24 hours if: 1 The grievance involves a refusal by the Part D plan sponsor to grant an enrollee's request for an expedited coverage determination or expedited redetermination, and 2 The enrollee has not yet purchased or received the drug that is in dispute.
What's New
December 2019: The Parts C and D Enrollee Grievance, Organization/Coverage Determinations and Appeals Guidance has been updated to include recent regulatory changes and will be effective January 1, 2020. Questions related to the guidance or appeals policy may be submitted to the Division of Appeals Policy at https://appeals.lmi.org.
Overview
Medicare health plans, which include Medicare Advantage (MA) plans (such as Health Maintenance Organizations, Preferred Provider Organizations, Medical Savings Account plans and Private Fee-For-Service plans) Cost Plans and Health Care Prepayment Plans, must meet the requirements for grievance, organization determination, and appeals processing under the MA regulations found at 42 CFR Part 422, Subpart M.
Web Based Training Course Available for Part C
The course covers requirements for Part C organization determinations, appeals, and grievances. Complete details can be accessed on the "Training" page, using the link on the left navigation menu on this page.
How to file a complaint about nursing home care?
To file a complaint about improper care or unsafe conditions in a hospital, home health agency, hospice, or nursing home, contact your State Survey Agency. The State Survey Agency is usually part of your State department of health services.
How to complain about home health?
If you have a complaint about the quality of care you’re getting from a home health agency, call the home health agency and ask to speak to the administrator. If you don’t believe your complaint has been resolved, call your state home health hotline. Your home health agency should give you this number when you start getting home health services.
What is an improper care complaint?
Improper care or unsafe conditions. You may have a complaint about improper care (like claims of abuse to a nursing home resident) or unsafe conditions (like water damage or fire safety concerns).
