How do I submit a reconsideration request to Medicare?
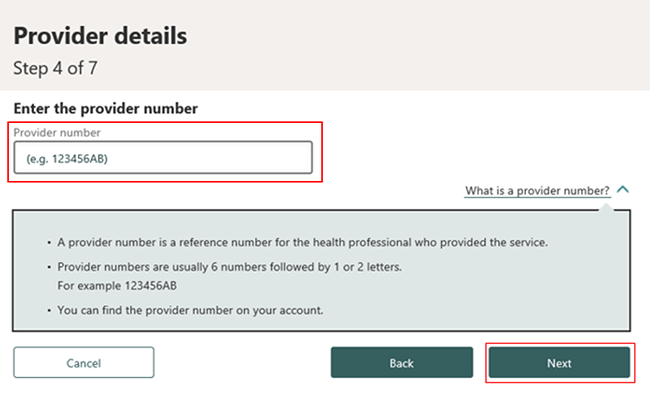
There are 2 ways to submit a reconsideration request.Fill out a "Medicare Reconsideration Request Form." [ PDF, 180 KB]Submit a written request to the QIC that includes: Your name and Medicare Number. The specific item(s) or service(s) for which you're requesting a reconsideration and the specific date(s) of service.
How do you address a letter to Medicare?
The Medicare appeal letter format should include the beneficiary's name, their Medicare health insurance number, the claim number and specific item or service that is associated with the appeal, dates of service, name and location of the facility where the service was performed and the patient's signature.
How long does Medicare have to respond to an appeal for reconsideration?
60 daysHow long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
What is Medicare claim address?
P.O. Box 2360. Jacksonville, FL 32231-0018.
How do I write a Medicare reconsideration letter?
Include this information in your written request:Your name, address, and the Medicare Number on your Medicare card [JPG]The items or services for which you're requesting a reconsideration, the dates of service, and the reason(s) why you're appealing.More items...
Can I email Medicare forms?
You can send us your form and supporting documents using the email address and postal address on the bottom of the form. To help us process your request please include copy or transfer in the subject line. You don't need to get your supporting documents certified.Feb 7, 2022
How do you write a redetermination letter?
How to Write an Appeal Letter in 6 Simple StepsReview the appeal process if possible.Determine the mailing address of the recipient.Explain what occurred.Describe why it's unfair/unjust.Outline your desired outcome.If you haven't heard back in one week, follow-up.Nov 11, 2019
What is the difference between reconsideration and redetermination?
Any party to the redetermination that is dissatisfied with the decision may request a reconsideration. A reconsideration is an independent review of the administrative record, including the initial determination and redetermination, by a Qualified Independent Contractor (QIC).Apr 4, 2022
What is redetermination in Medicare?
Any party to the initial claim determination that is dissatisfied with the decision may request a redetermination. A redetermination is a review of the claim by Medicare Administrative Contractor (MAC) personnel not involved in the initial claim determination.Dec 1, 2021
Where do I send Medicare Part B claims?
GBA Medicare Part B Claims.P.O. Box 6169 Indianapolis, IN 46206.
How do I contact Medicare Australia?
calling Medicare general enquiries on 132 011. visiting a Medicare Service Centre with your proof of identity.
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
What is a reconsideration in a redetermination?
A reconsideration is an independent review of the administrative record, including the initial determination and redetermination, by a Qualified Independent Contractor (QIC).
How long does it take to get a reconsideration decision?
Generally, the QIC will send this decision to all parties within 60 days of receipt of the request for reconsideration. If the QIC is unable to complete its reconsideration within this timeframe (with exceptions for extensions for additional evidence submissions and late filing), the QIC must send a notice to the parties and advise the appellant of the right to escalate the appeal to OMHA. If the party chooses to escalate the appeal to OMHA, a written request must be filed with the QIC in accordance with instructions on the escalation notice.
How long does it take for Medicare to redetermine?
The redetermination decision is presumed to be received 5 days after the date on the notice unless there is evidence to the contrary. A reconsideration must be requested in writing.
How long does a request for review take?
The request for review must be filed with the QIC within 60 days after the date of receipt of the dismissal. When the QIC performs its review of the dismissal, it will only decide on whether or not the dismissal was correct.
Can you request a reconsideration after a QIC has been filed?
A minimum monetary threshold is not required to request a reconsideration. Documentation that is submitted after the reconsideration request has been filed may result in an extension of the timeframe a QIC has to complete its decision. This does not apply to timely submission of documentation requested by the QIC.
Is it necessary to resubmit a document that was already submitted to the MAC?
It is not necessary to resubmit information that was already submitted to the MAC. Any documentation not submitted at the reconsideration level may be excluded from consideration at subsequent levels of appeal unless good cause is shown for not submitting the documentation previously.
Can a QIC dismiss a reconsideration request?
A QIC may dismiss a reconsideration request in the following instances: If the party (or appointed representative) requests to withdraw the appeal; or. If there are certain defects, such as. The party fails to file the request within the appropriate timeframe and did not show (or the QIC did not accept) good cause for late filing. ...
Enrollment forms
I have Part A and want to apply for Part B (Application for Enrollment in Part B/CMS-40B).
Appeals forms
I want to appoint a representative to help me file an appeal (Appointment of Representative form/CMS-1696).
How long does it take to get a reconsideration notice?
A request for reconsideration must be filed within 180 days after the date of receipt of the redetermina tion notice.
What is the Medicare block 1?
Block 1 - Beneficiary name: Include the first and last name of the beneficiary as it appears on the Medicare card. Block 2 - Medicare number: Include the beneficiary's complete Medicare number as found on their Medicare card. Block 3 - Item or service you wish to appeal: Provide a complete description of the item or service in question.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
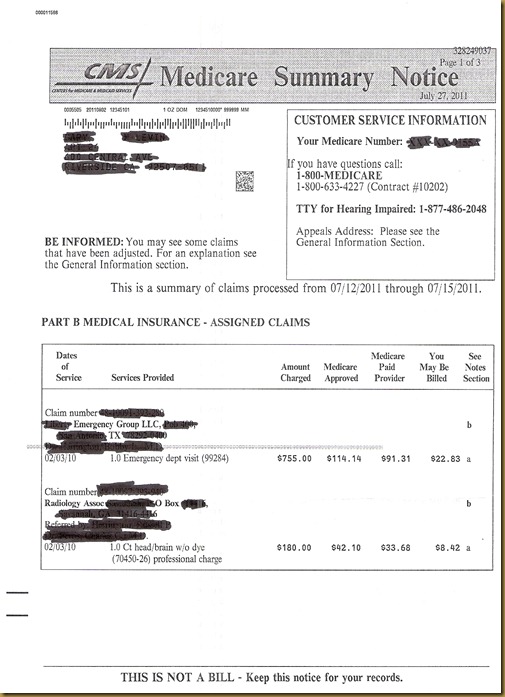
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
How long does Medicare take to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 calendar days. Payment request—60 calendar days. Learn more about appeals in a Medicare health plan.
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
What to do if you didn't get your prescription yet?
If you didn't get the prescription yet, you or your prescriber can ask for an expedited (fast) request. Your request will be expedited if your plan determines, or your prescriber tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function.
How to ask for a prescription drug coverage determination?
To ask for a coverage determination or exception, you can do one of these: Send a completed "Model Coverage Determination Request" form. Write your plan a letter.
How long does it take for a Medicare plan to make a decision?
The plan must give you its decision within 72 hours if it determines, or your doctor tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function. Learn more about appeals in a Medicare health plan.
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
What is a redetermination in Medicare?
A redetermination is a review of the claim by Medicare Administrative Contractor (MAC) personnel not involved in the initial claim determination.
Can a MAC dismiss a request for redetermination?
A MAC may dismiss a request for a redetermination for various reasons, some of which may be: If the party (or appointed representative) requests to withdraw the appeal. The party fails to file the request within the appropriate timeframe and did not show (or the MAC did not determine) good cause for late filing.
How to appeal a disability claim denied for medical reasons?
If you do not wish to appeal a medical decision online, you can use the Form SSA-561, Request for Reconsideration.
What to do if you disagree with a non medical decision?
If You Disagree With A Non-Medical Decision. You may request an appeal online for a "non-medical" decision. If you do not wish to appeal a "non-medical" decision online, you can use the Form SSA-561, Request for Reconsideration. Some examples of "non-medical" decisions are: you were denied another type of benefit, such as retirement or spouse's;
What is a home health change of care notice?
The “Home Health Change of Care Notice” is a written notice that your home health agency should give you when your home health plan of care is changing because of one of these:
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
What to do if you are not satisfied with QIC?
If you’re not satisfied with the QIC’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or , in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
Requesting A Reconsideration
- The appellant (the individual filing the appeal) has 180 days from the date of receipt of the redetermination decision to file a reconsideration request. The redetermination decision can be communicated through a Medicare Redetermination Notice (MRN), a Medicare Summary Notice (MSN), or a Remittance Advice (RA). The redetermination decision is pres...
QIC Review of A Dismissal of A Redetermination Request
- If a MAC has dismissed a redetermination request, any party to the redetermination has the right to appeal a dismissal of a redetermination request to a QIC if they believe the dismissal is incorrect. The request for review must be filed with the QIC within 60 days after the date of receipt of the dismissal. When the QIC performs its review of the dismissal, it will only decide on whethe…
Dismissal of A Reconsideration Request
- A QIC may dismiss a reconsideration request in the following instances: 1. If the party (or appointed representative) requests to withdraw the appeal; or 2. If there are certain defects, such as 2.1. The party fails to file the request within the appropriate timeframe and did not show (or the QIC did not accept) good cause for late filing 2.2. The representative is not appointed properly 2.…