
Full Answer
What was the Medicare Act of 1965 Quizlet?
Medicare Law of 1965. On July 30, 1965, President Johnson signed the Medicare Law as part of the Social Security Act Amendments. This established both Medicare, the health insurance program for Americans over 65, and Medicaid, the health insurance program for low-income Americans.
What is Medicare/Medicaid?
This established both Medicare, the health insurance program for Americans over 65, and Medicaid, the health insurance program for low-income Americans.
What does Medicare pay for hospitals?
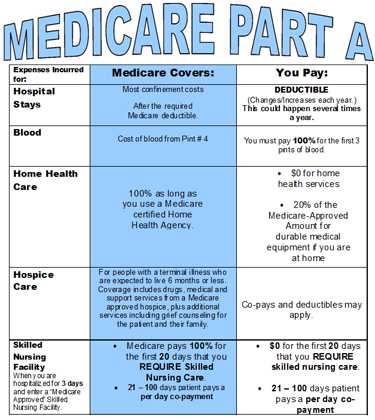
Medicare hospital insurance (Part A) pays for inpatient hospitla critical care access; skilled nursing facility stays; hospice care; and some home health care. Medicare hospital insurance (Part B) pays for doctors services; outpatient hospital care, durable medical equipment and some medical service that are not covered by Part A.
Is there legal guidance for Medicare&home health care?
“Medicare & Home Health Care” isn’t a legal document. Official Medicare Program legal guidance is contained in the relevant statutes, regulations, and rulings. 3 Table of Contents Section 1: Medicare Coverage of Home Health Care �������������������������5 Who’s eligible?
What happens when home health services end?
What is an appeal in Medicare?
How do I contact Medicare for home health?
Why is home health important?
Can Medicare take home health?
See more
About this website
How long is Medicare's definition of an episode of care for home health payment purposes?
ELEMENTS OF THE HH PPS The unit of payment under the HH PPS is a 60-day episode of care. A split percentage payment is made for most HH PPS episode periods.
Which of the following would be considered a patient's place of residence?
A patient's residence is wherever he or she makes his or her home. This may be his or her own dwelling, an apartment, a relative's home, a home for the aged, or some other type of institution.
Which is generally covered by Medicare for the homebound patient?
Medicare considers you homebound if: You need the help of another person or medical equipment such as crutches, a walker, or a wheelchair to leave your home, or your doctor believes that your health or illness could get worse if you leave your home.
How do you write home health frequency?
0:0011:35How to Write a Home Health Frequency - YouTubeYouTubeStart of suggested clipEnd of suggested clipDr. Smith physical therapist here and today I'm going to teach you how to properly write a homeMoreDr. Smith physical therapist here and today I'm going to teach you how to properly write a home health frequency for patients on Medicare Part A services.
How Much Does Medicare pay for home health care per hour?
Medicare will cover 100% of the costs for medically necessary home health care provided for less than eight hours a day and a total of 28 hours per week. The average cost of home health care as of 2019 was $21 per hour.
Which client would be appropriate for home health care services?
Which client would most likely require home health services? Home care is appropriate for a client with health needs that exceed the abilities of family and friends.
How does CMS define homebound?
To be homebound means that leaving home takes considerable and taxing effort. A person may leave home for medical treatment or short, infrequent absences for non-medical reasons, such as a trip to the barber or to attend religious service.
What is the criteria for being housebound?
A patient is housebound if they are unable to leave their home at all, or if they require significant assistance to leave the house due to illness, frailty, surgery, disability, mental ill-health, or nearing the end of life.
Which of the following are homebound criteria?
Medicare uses the following criteria to define homebound: To leave your home, you need help, including the help of another person, crutches, a walker, a wheelchair, or special transportation. Your need for help must stem from an illness or injury. It's difficult for you to leave your home and you typically can't do so.
How do you write a frequency therapy?
How should I document the intended frequency and duration of patient care?The first is a number of times per week for a number of weeks (3 times per week for 4 weeks).The second is based on the total number of treatment sessions (2 times per week for 12 treatment sessions).More items...
The booklet is now available in another format. Please visit https ...
Title: MLN908143 - Obsolete Medicare Home Health Benefit Booklet Author: Centers for Medicare & Medicaid Services \(CMS\) Medicare Learning Network \(MLN\)
Medicare and Home Health Care - CMS
3 Words in blue are defined on pages 26-27. Home health care includes skilled nursing care, as well as other skilled care services, like physical and occupational therapy, speech-
This official government booklet tells you - Medicare
Medicare & Home Health Care CENTERS for MEDICARE & MEDICAID SERVICES This . official government booklet tells you: Who’s eligible What services are covered
Home Health Medicare Billing Codes Sheet
Home Health Medicare Billing Codes Sheet Value Code (FL 39-41) 61 CBSA code for where HH services were provided. CBSA codes are required on all 32X TOB. Place “61” in the first value code field locator and the CBSA code in the dollar
Home Health Services Coverage - Medicare
$0 for covered home health care services. Aft er you meet the Part B deductible, 20% of the Medicare-Approved Amount for Medicare-covered medical equipment.; Before you start getting your home health care, the home health agency should tell you how much Medicare will pay.
The How-To Guide to Home Health Billing, HOME HEALTH BILLING Second ...
Joan L. Usher, BS, RHIA, ACE The How-To Guide to HOME HEALTH BILLING SECOND EDITION 100 Winners Circle, Suite 300 Brentwood, TN 37027 www.hcmarketplace.com
What happens when home health services end?
When all of your covered home health services are ending, you may have the right to a fast appeal if you think these services are ending too soon. During a fast appeal, an independent reviewer called a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) looks at your case and decides if you need your home health services to continue.
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
How do I contact Medicare for home health?
If you have questions about your Medicare home health care benefits or coverage and you have Original Medicare, visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) . TTY users can call 1-877-486-2048. If you get your Medicare benefits through a Medicare Advantage Plan (Part C) or other
Why is home health important?
In general, the goal of home health care is to provide treatment for an illness or injury. Where possible, home health care helps you get better, regain your independence, and become as self-sucient as possible. Home health care may also help you maintain your current condition or level of function, or to slow decline.
Can Medicare take home health?
In general, most Medicare-certified home health agencies will accept all people with Medicare . An agency isn’t required to accept you if it can’t meet your medical needs. An agency shouldn’t refuse to take you because of your condition, unless the agency would also refuse to take other people with the same condition.
What is the 30-day period for Medicare?
The agency that establishes the 30-day period is the only entity that can bill and receive payment for medical supplies during a 30- day period for a patient under a home health plan of care. Both routine and nonroutine medical supplies are included in the base rates for every Medicare home health patient regardless of whether or not the patient requires medical supplies during the 30-day period.
What is freedom of choice for Medicare home health?
beneficiary exercises his or her freedom of choice for the services under the home health benefit listed in §1861(m) of the Act, including medical supplies, but excluding DME covered as a home health service by choosing the HHA. Once a home health patient chooses a particular HHA, he or she has clearly exercised freedom of choice with respect to all items and services included within the scope of the Medicare home health benefit (except DME). The HHA's consolidated billing role supersedes all other billing situations the beneficiary may wish to establish for home health services covered under the scope of the Medicare home health benefit during the certified episode.
How is partial payment adjustment calculated?
The partial payment adjustment for the original 30-day period is calculated to reflect the length of time the beneficiary remained under the care of the original HHA based on the first billable visit date through and including the last billable visit date.The partial payment adjustment will be calculated by using the span of days (first billable service date through and including the last billable service date) under the original plan of care as a proportion of the 30-day period. The proportion will then be multiplied by the original case-mix and wage index to produce the 30-day payment.
What happens when you change ownership of a home health plan?
When there is a change of ownership and the new owner accepts assignment of the existing provider agreement, the new owner is subject to all the terms and conditions under which the existing agreement was issued. The provider number remains the same if the new HHA owner accepts assignment of the existing provider agreement. As long as the new owner complies with the regulations governing home health PPS, billing, and payment for 30-day periods with applicable adjustments for existing patients under an established plan of care will continue on schedule through the change in ownership with assignment. The 30-day period would be uninterrupted spanning the date of sale. The former owner is required to file a terminating cost report. Instructions regarding when a cost report is filed are in the Provider Reimbursement Manual, Part 1, §1500.
How long does it take for a HHA to receive a payment?
An HHA receives a national, standardized 30-day payment of a predetermined rate for home health services unless CMS determines an intervening event warrants a new 30-day period for purposes of payment.
What is a full 30-day period payment?
The documented event of a patient's death would result in a full 30-day period payment, unless the death occurred in a low utilization payment adjusted 30-day period. Consistent with all episodes in which a patient receives four or fewer visits, if the patient's death occurred during a low utilization adjusted 30-day payment period, the period would be paid at the low utilization payment adjusted amount. In the event of a patient's death during an adjusted 30-day period, the total adjusted period would constitute the full 30-day period payment.
When is the last day covered by the HHA plan of care?
medication administration every 2 weeks. The last day covered by the plan of care is July 31. The patient's next I.V. medication administration is scheduled for August 5 and the physician or allowed practitioner does not sign the plan of care until August 6. The HHA acquires an oral order for the I.V. medication administration before the August 5 visit, and therefore the visit is considered to be provided under a plan of care established and approved by the physician or allowed practitioner.
What is Medicare Part C?
Medicare Part C. also known as Medicare Advantage Plans, are health plan options that are approved by Medicare but managed by private companies.
When is the 7 month enrollment period for Medicare?
General Enrollement period. held every Jan. 1st through March 31 of each year. is for those individuals that wait until they reach age 65 causing ...
What is Medicare special needs?
Medicare special needs plans. cover all Medicare part A & B health care for individuals who can benefit the most from special care for chronic illnesses, care management of multiple diseases, and focused care management. Medicare part D.
How many days does a spell of illness last?
begins with the first day of hospitalization and ends when the patient has been out of the hospital for 60 consecutive days. Medicare literature - "spell of illness". formerly called "spell of sickness", in place of benefit period. lifetime reserve days.
How long is respite care?
1. two periods of 90 days each. 2. one 30 day period. 3. a final lifetime extension of unlimited duration. respite care. is the temporary hospitalization of a terminally ill, dependent hospice pt for the purpose of providing relief for the nonpaid person who has the major day to day responsibility for care of that pt.
How old do you have to be to qualify for medicare?
individuals or their spouses to have worked at least 10 years in medicare covered employment. 2. individuals to be the minimum of 65 years old. 3. individuals to be citizens or permanent residents of the united states.
Do you have to pay Medicare premiums if you are 65?
individuals age 65 and over do not pay a monthly premium for medicare part A, IF they or a spouse paid Medicare taxes while they were working. Those who didn't pay medicare taxes "buy in" to medicare part A by paying monthly premiums. Applying for Medicare.
What is Medicare Part B?
These policies are known as. Medigap insurance policies.
Can Medicare Part B be covered by private insurance?
Medicare Part B deductibles, coinsurance, and some noncovered services can be covered by buying policies from federally approved private insurance carriers. These policies are known as. Click card to see definition 👆. Tap card to see definition 👆. Medigap insurance policies.
What are the laws that govern Medicare fraud?
Medicare Fraud and Abuse Laws. In an effort to eliminate erroneous healthcare spending for Medicare and Medicaid programs, Congress passed several acts that target the fraud and abuse that is present in the Medicare and Medicaid systems. There are several laws that govern Medicare Fraud. -The False Claims Act.
What is Medicare fraud?
medicare fraud (2/4) Fraud is an occurrence where someone intentionally falsifies information or deceives Medicare. Abuse is when a healthcare provider or supplier does not follow good medical practices that results in unnecessary costs, improper payment, or services that are not medically necessary.
What is Section 3729-3733?
Sections 3729-3733 protects the government from being overcharged or sold substandard goods or services. Will impose civil liability on any person who knowingly submits, or causes to a claim to be submitted that is a false or fraudulent claim to the federal government for payment.
What is the Affordable Care Act?
The Affordable Care Act requires health insurance companies to submit data on the proportion of premium revenues spent on clinical services and quality improvement.
When was the 1/3 law passed?
In 1981 , there was the enactment of the Civil Monetary Penalties Law (CMPL) 1/3.
Is Medicare fraud a crime?
medicare fraud (3/4) Fraud is not only limited to practitioners, it is now becoming involved with organized crime where they are masquerading as Medicare providers and suppliers. Fraud can be committed by a healthcare provider such as a doctor or healthcare practitioner or supplier.
What is professional health care?
Professional health care organizations are stakeholders in the health care system. They provide. taxes paid at both the federal and state level. The total cost of health care in the United States is often expressed as a percentage of the country's gross domestic product (GDP).
What is the science that defines how individuals are genetically programmed to respond to drugs called?
The science that defines how individuals are genetically programmed to respond to drugs is called. pharmacogenomics. The use of this technique will allow the recreation of a solid object from a digital file that could help in drug testing and organ structure. It is known as. three-dimensional bioprinting.
What happens when home health services end?
When all of your covered home health services are ending, you may have the right to a fast appeal if you think these services are ending too soon. During a fast appeal, an independent reviewer called a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) looks at your case and decides if you need your home health services to continue.
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
How do I contact Medicare for home health?
If you have questions about your Medicare home health care benefits or coverage and you have Original Medicare, visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) . TTY users can call 1-877-486-2048. If you get your Medicare benefits through a Medicare Advantage Plan (Part C) or other
Why is home health important?
In general, the goal of home health care is to provide treatment for an illness or injury. Where possible, home health care helps you get better, regain your independence, and become as self-sucient as possible. Home health care may also help you maintain your current condition or level of function, or to slow decline.
Can Medicare take home health?
In general, most Medicare-certified home health agencies will accept all people with Medicare . An agency isn’t required to accept you if it can’t meet your medical needs. An agency shouldn’t refuse to take you because of your condition, unless the agency would also refuse to take other people with the same condition.
