How do I know what Medicare plan I have?
- Review your Medicare plan coverage options. It’s a good idea to review your Medicare coverage every year to make sure the benefits of your Medicare plan remain aligned with your ...
- Make changes to your Medicare plan coverage during the right time of year. ...
- Find out what Medicare plan may fit your needs. ...
What are the federal guidelines for Medicaid?
- State Plan Flexibilities
- Using Section 1115 Demonstrations for Disaster Response
- Home & Community-Based Services in Public Health Emergencies
- Federal Disaster Resources
- Section 1135 Waiver Flexibilities
- Coronavirus Disease 2019 (COVID-19)
What are the guidelines for Medicare?
or other qualified health care professional, per calendar month, with the following required elements: multiple (two or more) chronic conditions expected to last at least 12 months, or until the death of the patient chronic conditions place the patient at significant risk of death, acute exacerbation/ decompensation, or functional decline …
Will Medicaid pay for my Medicare Part B premium?
But, anyone with Medicaid or other forms of assistance that could pay the Part B premium can’t enroll in these plans. The plan only participates with Social Security; so, no direct payments are sent to you by the carrier. The amount you get back can range from $0.10 in some counties up to $148.50.

What does it mean when insurance follows Medicare guidelines?
Many plans say “We follow Medicare” — and most would take this to mean that the Medicare Advantage Plan will cover and process claims the same as original Medicare would.
What types of healthcare are not covered by Medicare?
In general, Original Medicare does not cover:Prescription drugs.Long-term care (such as extended nursing home stays or custodial care)Hearing aids.Most vision care, notably eyeglasses and contacts.Most dental care, notably dentures.Most cosmetic surgery.Massage therapy.More items...•
Who are the three groups covered by Medicare?
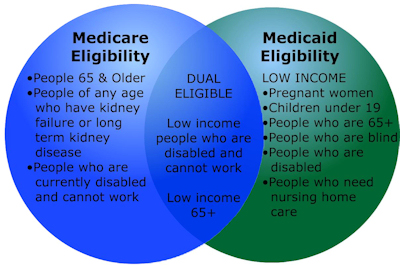
Medicare is the federal health insurance program for:People who are 65 or older.Certain younger people with disabilities.People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
Which of the following are covered by Medicare?
Many Medicare Advantage plans offer the following benefits:hospitalization.some home healthcare services.hospice care.doctor's visits.prescription drug coverage.preventive care.dental.vision.More items...
Do all hospitals accept Medicare?
Not all hospitals accept Medicare, but luckily, the vast majority of hospitals do. Generally, the hospitals that do not accept Medicare are Veterans Affairs and active military hospitals (they operate with VA and military benefits instead), though there are a few other exceptions nationwide.
Which of the following services would not be covered under Medicare Part B?
But there are still some services that Part B does not pay for. If you're enrolled in the original Medicare program, these gaps in coverage include: Routine services for vision, hearing and dental care — for example, checkups, eyeglasses, hearing aids, dental extractions and dentures.
Is Kaiser a Medicare?
Kaiser Permanente is an HMO plan with a Medicare contract. Enrollment in Kaiser Permanente depends on contract renewal. Every year, Medicare evaluates plans based on a 5-star rating system.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Which of the following services are covered by Medicare Part B quizlet?
Part B helps cover medically-necessary services like doctors' services, outpatient care, durable medical equipment, home health services, and other medical services.
Under which of the following Medicare plans for primary care and specialists services is the patient required to pay a monthly premium quizlet?
Part B is medical insurance for ambulatory care, including primary care and specialists for which patients are required to pay a monthly premium; Part B functions similar to a PPO in that patients can visit any specialist without a referral.
What services are covered under Medicare quizlet?
The program covers all those who are eligible regardless of their health status, medical conditions, or incomes. Basic health services, including hospital stays, physician visits, and prescription drugs. What are some gaps in Medicare coverage? Long-term care services, vision services, dental care, and hearing aids.
Which of the following is not true about Medicare?
Which of the following is not true about Medicare? Medicare is not the program that provides benefits for low income people _ that is Medicaid. The correct answer is: It provides coverage for people with limited incomes.
What is the age limit for Medicare?
If you are 65 years old, younger than 65 with a disability, or have end-stage rental disease, you are eligible for the U.S. federal health insurance program known as Original Medicare. Ever since its beginning in 1965, Medicare has provided medical services to millions of people for free or at a reduced cost.
What is part A insurance?
Part A is hospital insurance which pays for inpatient hospital stays, skilled nursing facility stays, some types of surgery, hospice care, and other forms of home health care. Part B is medical insurance which pays for medical services and supplies that are certified as medically necessary for treating a health condition.
Is Medicare Advantage mandatory?
Enrolling in a Medicare Advantage plan is not mandatory for individuals who are eligible for Medicare; it’s an alternative to Original Medicare. If you decide to enroll in a Medicare Advantage plan, you receive all your health care and Medicare coverage through the policy you choose.
Does Medicare Advantage cover dental care?
Your Medicare Advantage plan may cover additional services such as hearing exams, vision care, dental care, or fitness plans, for example. As a Medicare Advantage enrollee, you are also required to adhere to all the plan regulations that have been set by CMS. For example, your policy does not cover services you receive outside your provider network unless it is an emergency or something urgent, therefore, you must receive services inside the plan’s network for them to be covered by your policy.
What is Medicare Advantage Policy?
Medicare Advantage Policy Guidelines are intended to ensure that coverage decisions are made accurately based on the code or codes that correctly describe the health care services provided.
What is UnitedHealthcare's Medicare Advantage Policy?
UnitedHealthcare has developed Medicare Advantage Policy Guidelines to assist us in administering health benefits. These Policy Guidelines are provided for informational purposes, and do not constitute medical advice.
What is a member specific benefit plan?
The member specific benefit plan document identifies which services are covered, which are excluded, and which are subject to limitations. In the event of a conflict, the member specific benefit plan document supersedes the Medicare Advantage Policy Guidelines.
Where is the provider service number on a health card?
For questions, please contact your local Network Management representative or call the Provider Services number on the back of the member’s health ID card.
Do you have to consult your physician before making a decision about medical care?
Members should always consult their physician before making any decisions about medical care. Benefit coverage for health services is determined by the member specific benefit plan document* and applicable laws that may require coverage for a specific service.
What is original Medicare?
Your costs in Original Medicare. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. for most services.
What is a doctor in Medicare?
A doctor can be one of these: Doctor of Medicine (MD) Doctor of Osteopathic Medicine (DO) In some cases, a dentist, podiatrist (foot doctor), optometrist (eye doctor), or chiropractor. Medicare also covers services provided by other health care providers, like these: Physician assistants. Nurse practitioners.
What does "covered" mean in medical terms?
medically necessary. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
Do you pay for preventive services?
for most services. You pay nothing for certain preventive services if your doctor or other provider accepts
How many days can you be on Medicare?
Fewer than 7 days each week. ■ Daily for less than 8 hours each day for up to 21 days. In some cases, Medicare may extend the three week limit if your
How many days can you have home health care?
care. You can have more than one 30-day period of care. Payment for each 30-day period is based on your condition and care needs. Getting treatment from a home health agency that’s Medicare-certified can reduce your out-of-pocket costs. A Medicare-certified home health
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
What is the ABN for home health?
The home health agency must give you a notice called the “Advance Beneficiary Notice of Noncoverage” (ABN) in these situations. See the next page.
What happens when home health services end?
When all of your covered home health services are ending, you may have the right to a fast appeal if you think these services are ending too soon. During a fast appeal, an independent reviewer called a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) looks at your case and decides if you need your home health services to continue.
Does Medicare cover nursing and therapy?
5), Medicare covers these services if they’re reasonable and necessary for the treatment of your illness or injury. “Skilled nursing and therapy services are covered when your doctor determines that the care you need requires the specialized judgment, knowledge, and skills of a nurse or therapist to be safely and effectively provided.
Does Medicare cover wound dressings?
Medicare covers supplies, like wound dressings, when your doctor orders them as part of your care. Medicare pays separately for durable medical equipment
What is the first choice for Medicare?
The first choice is between going with the original program, Parts A and B, or to choose a private plan through Part C.
Who is eligible for Medicare?
The biggest group that Medicare covers is adults over the age of 65. Anyone over 65 who has been a legal resident in the U.S. for at least five years, who has worked long enough (or whose spouse has) to be eligible for Social Security, or who is a government employee or retiree who did not pay into Social Security, is eligible for Medicare.
What is Medicare?
Medicare is a public and federal health insurance program for Americans over the age of 65 and for certain other individuals who qualify for coverage. Medicare is funded entirely by the federal government through the Social Security Administration. The funding comes from taxes that workers in the U.S. pay into Social Security. Medicare is managed by the federal department known as the Centers for Medicare and Medicaid Services.
How is Medicare different from Medicaid?
While Medicaid is funded by both federal and state governments and is administered separately by each state government, Medicare is entirely federal. It is funded by the federal government and administered by the federal government. This means that rules for eligibility and coverage under Medicare are the same across all states.
Why is Medicare important?
Medicare reaches many people in the U.S., but it is only useful if those enrollees get good health care and have good access to physicians, treatments, procedures, hospitals, and other services.
What percentage of Medicare patients accept new patients?
While most physicians, 91 percent , accept new Medicare patients, there is a big gap in mental health.
What is a Part D plan?
Part D. This is the prescription drug program, which is optional. Enrollees can choose from among Medicare-approved private insurers for medication coverage. Part D plans usually have premiums, deductibles, and co-pays.
What is CKD guideline?
This guideline outlines evidence-based recommendations to aid clinicians in the treatment of particular diseases or groups of patients for all stages of chronic kidney disease (CKD) and related complications.
Where is the provider service number on a network card?
For questions, please contact your local Network Management representative or call the Provider Services number on the back of the member’s ID card.