Medicare is primary when your employer has less than 20 employees. Medicare will pay first and then your group insurance will pay second. If this is your situation, it’s important to enroll in both parts of Original Medicare when you are first eligible for coverage at age 65.
Which is primary provider Medicare or Blue Cross?
If you have Medicare and Blue Cross which is primary provider? In most cases, Medicare is primary. Some of the most common situations where Medicare can pay secondary are: -The individual or his/her spouse is currently employed/working and covered under an employer group health plan as a result of current employment.
When do you have to enroll in both Medicare and group insurance?
You are 65 or Older and Your Employer is a Small Business Medicare is primary when your employer has less than 20 employees. Medicare will pay first and then your group insurance will pay second. If this is your situation, it’s important to enroll in both parts of Original Medicare when you are first eligible for coverage at age 65.
What is the BCN 65 plan?
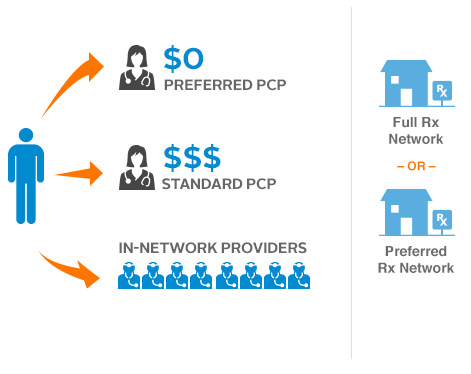
BCN 65 is an HMO plan. When you get your health coverage from an HMO, or health maintenance organization, you choose a primary care physician from the plan's network. That doctor coordinates all your care and refers you to other doctors when needed.
Is BlueChoice part a coinsurance part of Medicare?
Part A coinsurance. BlueChoice 65 and BlueChoice 65 Select are not connected with or endorsed by the U.S. government or the federal Medicare program. Please see your agent for benefit exclusions, limitations and reductions.

Does Medicare become primary at 65?
I dropped employer-offered coverage. If you're 65 or older, Medicare pays first unless both of these apply: You have coverage through an employed spouse. Your spouse's employer has at least 20 employees.
How do I know if my Medicare is primary or secondary?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
How do you determine which health insurance is primary?
Primary insurance is a health insurance plan that covers a person as an employee, subscriber, or member. Primary insurance is billed first when you receive health care. For example, health insurance you receive through your employer is typically your primary insurance.
Is Medicare considered primary?
Even if you have a group health plan, Medicare is the primary insurer as long as you've been eligible for Medicare for 30 months or more.
Does Medicare automatically forward claims to secondary insurance?
If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
How do you make Medicare primary?
Making Medicare Primary. If you're in a situation where you have Medicare and some other health coverage, you can make Medicare primary by dropping the other coverage. Short of this, though, there's no action you can take to change Medicare from secondary to primary payer.
When two insurance which one is primary?
If you have two plans, your primary insurance is your main insurance. Except for company retirees on Medicare, the health insurance you receive through your employer is typically considered your primary health insurance plan.
Can you have 2 primary insurances?
BY Anna Porretta Updated on January 21, 2022. Yes, you can have two health insurance plans. Having two health insurance plans is perfectly legal, and many people have multiple health insurance policies under certain circumstances.
How does it work if you have 2 insurances?
When you have two forms of health insurance coverage, your primary insurance pays the first portion of the claim up to your coverage limits. Your secondary insurance may pick up some or all of the remaining costs. However, you still might be responsible for some cost-sharing.
Can I keep my private insurance and Medicare?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
Will Medicare pay my primary insurance deductible?
“Medicare pays secondary to other insurance (including paying in the deductible) in situations where the other insurance is primary to Medicare.
When a patient is covered through Medicare and Medicaid which coverage is primary?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors' visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
What Is Medicare Primary Insurance?
Medicare Primary insurance simply means that Medicare pays first. Whether Medicare pays first or second depends on what types of other health cover...
Medicare Expects You to Know Who Is Primary
You see, Patricia didn’t realize that since her employer has less than 20 employees, Medicare would be her primary coverage. By failing to enroll i...
to Enroll Or Not to Enroll?
Not everyone needs to enroll in Medicare right when they turn 65. Many people continue to work past age 65 and have access to employer coverage thr...
When Medicare Is Secondary
Secondary insurance pays after your primary insurance. It serves to pick up costs that the primary coverage didn’t cover. For example, if your prim...
Feeling Unsure About When Is Medicare Primary?
Figuring all this out is enough to give anyone a headache – we know! Fortunately Boomer Benefits has helped tens of thousands of Medicare beneficia...
What is the difference between Medicare and Medicaid?
Eligible for Medicare. Medicare. Medicaid ( payer of last resort) 1 Liability insurance only pays on liability-related medical claims. 2 VA benefits and Medicare do not work together. Medicare does not pay for any care provided at a VA facility, and VA benefits typically do not work outside VA facilities.
Is Medicare a secondary insurance?
When you have Medicare and another type of insurance, Medicare is either your primary or secondary insurer. Use the table below to learn how Medicare coordinates with other insurances. Go Back. Type of Insurance. Conditions.
What does it mean when Medicare is primary?
When Medicare is Primary. Primary insurance means that it pays first for any healthcare services you receive. In most cases, the secondary insurance won’t pay unless the primary insurance has first paid its share. There are a number of situations when Medicare is primary.
When does Medicare end for ESRD?
You would then re-enroll when you turn 65. Typically Medicare due to ESRD will end 36 months after you’ve had your kidney transplant unless you also qualify for Medicare due to age or other disability.
What is the term for a former employer providing health insurance for you after you are no longer working?
You Have Retiree Coverage or COBRA. Sometimes a former employer provides group health insurance coverage for you AFTER you are no longer working. This is called retiree coverage. Medicare is primary and your providers must submit claims to Medicare first. Your retiree coverage through your employer will pay secondary.
What is tricare for life?
You Have Tricare-for-Life. Tricare-for-Life (TFL) is for military retirees and their spouses who are also eligible for Medicare. In this scenario, Medicare is the primary insurance for any care you receive at non-military providers, so you need to enroll in both Part A and B.
What happens if you enroll late in Medicare Part B?
It’s critical that you understand your coverage. Late enrollment into Medicare Part B can cause you to pay a penalty if certain conditions are not met. Learn more about Medicare Part B costs here.
Does Medicare expect you to know who is primary?
Medicare Expects YOU to Know Who is Primary. In our example above, Patricia didn’t realize that since her employer has less than 20 employees, Medicare would be her primary coverage. By failing to enroll in Medicare, she was now responsible for paying for the cost of that MRI.
Is Medicare primary or secondary?
Then of course there is employer coverage. If you have active employer coverage, whether Medicare is primary or secondary also depends on the size of the insurance company.
When is Medicare paid first?
When you’re eligible for or entitled to Medicare because you have End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, the group health plan or retiree coverage pays first and Medicare pays second. You can have group health plan coverage or retiree coverage based on your employment or through a family member.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What does BCRC do?
The BCRC will gather information about any conditional payments Medicare made related to your settlement, judgment, award or other payment. If you get a payment, you or your lawyer should call the BCRC. The BCRC will calculate the repayment amount (if any) on your recovery case and send you a letter requesting repayment.
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
What percentage of Medicare is covered by BCN 65?
For other medical services, Medicare usually pays for 80 percent of the cost and you pay 20 percent. Your share of those amounts is called coinsurance. BCN 65 is a plan from Blue Care Network that pays your Medicare deductibles and coinsurance.
How much does BCN 65 pay?
You can also learn more about BCN 65 from the plan coverage (PDF). It shows you how much BCN 65 pays for services covered by Medicare. $211 a month.
How much does Medicare cost if you end up in the hospital?
You have to pay an amount called a deductible before Medicare starts paying for services. If you end up in the hospital, after 60 days you pay around $300 per day — and that amount increases the longer you're there. For other medical services, Medicare usually ...
How much is Medicare Part A and Part B?
Medicare Part A and Part B is your primary health coverage. Yes. Yes. Monthly payment you have in addition to your Medicare Part B premium. $211 a month. Payment varies and can be based on your age, gender, health status and more. Network.
Is BCN 65 an HMO?
But that's how it works. BCN 65 is an HMO plan. When you get your health coverage from an HMO, or health maintenance organization, you choose a primary care physician from the plan's network. That doctor coordinates all your care and refers you to other doctors when needed.
Hospitalization
Part A coinsurance plus coverage for 365 additional days after Medicare benefits end.
Medical Expenses
Part B coinsurance (generally 20% of Medicare-approved expenses) or copayments for hospital outpatient services. Plan N requires insureds to pay a portion of Part B coinsurance or copayments.
What is Medicare for people over 65?
GET TO KNOW MEDICARE. Medicare is a health insurance program provided by the federal government, available to people: • 65 and older • Under 65 with certain disabilities • With permanent kidney failure who need dialysis treatment or a transplant (End-Stage Renal Disease) .
What is Blue365 for Blue Cross?
Blue365 is a discount program exclusively for Blue Cross and Blue Shield members. Through the program, you can get discounts on different products and services that can help you live a healthy lifestyle, such as diet and exercise plans, gym shoes and athletic apparel, hearing aids and more.
What is Part D coverage?
Part D. Prescription drug coverage Covers prescriptions which aren’t included in Part A and B coverage Benefits and premiums vary based on the plan you choose. To learn more about Medicare coverage and premiums, visit medicare.gov . or call 1-800-MEDICARE (TTY: 1-877-486-2048). << Previous Next >>. 3.
What is Blue365 discount?
Through the program, you can get discounts on different products and services that can help you live a healthy lifestyle, such as diet and exercise plans, gym shoes and athletic apparel, hearing aids and more. View all the current available deals at
How to contact Medicare for service benefits?
or call 1-800-MEDICARE (TTY: 1-877-486-2048) . << Previous Next >>. 3. Combining your Service Benefit Plan coverage with Medicare is a choice. Here are some things to know that can help you decide: Keep your future healthcare needs in mind before making a decision.
How much is the penalty for delay in Medicare?
The penalty is a 10% premium increase for each year you choose to delay your enrollment. So, if you decide to enroll five years after you’re first eligible, your premium would be 50% higher than it would be if you had taken Medicare initially. There is an exception to this.
How long do you have to enroll in Part B?
Once you retire, you’ll have eight months to enroll in Part B before the penalty kicks in. . General Enrollment Period .
