Is Medicare supplement primary or secondary?
FAQs. Is a Medicare Supplement plan primary or secondary? Medicare Supplement plans are secondary payers to Medicare. Medicare will be billed first, then your supplement plan will be billed second.
Is supplemental insurance a primary?
The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) to pay. In some rare cases, there may also be a third payer.
How do you determine which insurance is primary and which is secondary?
The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer. The secondary payer only pays if there are costs the primary insurer didn't cover.
Is Medicare always the primary insurer?
If you don't have any other insurance, Medicare will always be your primary insurance. In most cases, when you have multiple forms of insurance, Medicare will still be your primary insurance. Here are several common instances when Medicare will be the primary insurer.
Does Medicare automatically forward claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.
How do you make Medicare primary?
Making Medicare Primary. If you're in a situation where you have Medicare and some other health coverage, you can make Medicare primary by dropping the other coverage. Short of this, though, there's no action you can take to change Medicare from secondary to primary payer.
When two insurance which one is primary?
If you have two plans, your primary insurance is your main insurance. Except for company retirees on Medicare, the health insurance you receive through your employer is typically considered your primary health insurance plan.
Can you have 2 primary insurances?
BY Anna Porretta Updated on January 21, 2022. Yes, you can have two health insurance plans. Having two health insurance plans is perfectly legal, and many people have multiple health insurance policies under certain circumstances.
What is considered primary insurance?
Primary insurance is a health insurance plan that covers a person as an employee, subscriber, or member. Primary insurance is billed first when you receive health care. For example, health insurance you receive through your employer is typically your primary insurance.
Will secondary pay if primary denies?
If your primary insurance denies coverage, secondary insurance may or may not pay some part of the cost, depending on the insurance. If you do not have primary insurance, your secondary insurance may make little or no payment for your health care costs.
Can a person have a Medicare Advantage plan and a Medicare supplement plan?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
What Is Medicare Primary Insurance?
Medicare Primary insurance simply means that Medicare pays first. Whether Medicare pays first or second depends on what types of other health cover...
Medicare Expects You to Know Who Is Primary
You see, Patricia didn’t realize that since her employer has less than 20 employees, Medicare would be her primary coverage. By failing to enroll i...
to Enroll Or Not to Enroll?
Not everyone needs to enroll in Medicare right when they turn 65. Many people continue to work past age 65 and have access to employer coverage thr...
When Medicare Is Secondary
Secondary insurance pays after your primary insurance. It serves to pick up costs that the primary coverage didn’t cover. For example, if your prim...
Feeling Unsure About When Is Medicare Primary?
Figuring all this out is enough to give anyone a headache – we know! Fortunately Boomer Benefits has helped tens of thousands of Medicare beneficia...
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
Does Medicare cover prescription drugs?
Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage. If you want prescription drug coverage, you can join a Medicare Prescription Drug Plan (Part D). If you buy Medigap and a Medicare drug plan from the same company, you may need to make 2 separate premium payments. Contact the company to find out how to pay your premiums.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
Does Medigap cover everything?
Medigap policies don't cover everything. Medigap policies generally don't cover. long-term care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
What does it mean when Medicare is primary?
When Medicare is Primary. Primary insurance means that it pays first for any healthcare services you receive. In most cases, the secondary insurance won’t pay unless the primary insurance has first paid its share. There are a number of situations when Medicare is primary.
When does Medicare end for ESRD?
You would then re-enroll when you turn 65. Typically Medicare due to ESRD will end 36 months after you’ve had your kidney transplant unless you also qualify for Medicare due to age or other disability.
What happens if you enroll late in Medicare Part B?
It’s critical that you understand your coverage. Late enrollment into Medicare Part B can cause you to pay a penalty if certain conditions are not met. Learn more about Medicare Part B costs here.
Does Medicare expect you to know who is primary?
Medicare Expects YOU to Know Who is Primary. In our example above, Patricia didn’t realize that since her employer has less than 20 employees, Medicare would be her primary coverage. By failing to enroll in Medicare, she was now responsible for paying for the cost of that MRI.
Is Medicare primary or secondary?
Then of course there is employer coverage. If you have active employer coverage, whether Medicare is primary or secondary also depends on the size of the insurance company.
Is Medicare a secondary insurance?
Medicare is secondary to your group health insurance if the company has 20 or more employees. If the group insurance is affordable, you may choose to delay your enrollment in Part B. ALWAYS speak with a licensed insurance agent who specializes in Medicare before making this decision.
Can you get medicaid if you are low?
Otherwise, you may be responsible for the portions that Medicaid can’t cover. Medicare is primary to Medicaid. People who qualify for Medicaid can get help paying for their Medicare Part B and D premiums. If your income is low and you think you might be eligible, contact your state Medicaid office for an application.
What does the secondary payer pay for?
The secondary payer only pays if there are costs the first payer didn’t cover.
Does Medicare know if you have other coverage?
Medicare doesn’t automatically know if you have other coverage. But your insurers must report to Medicare when they’re the primary payer on your medical claims.
What is the difference between Medicare and Medicaid?
Eligible for Medicare. Medicare. Medicaid ( payer of last resort) 1 Liability insurance only pays on liability-related medical claims. 2 VA benefits and Medicare do not work together. Medicare does not pay for any care provided at a VA facility, and VA benefits typically do not work outside VA facilities.
Is Medicare a secondary insurance?
When you have Medicare and another type of insurance, Medicare is either your primary or secondary insurer. Use the table below to learn how Medicare coordinates with other insurances. Go Back. Type of Insurance. Conditions.
How long can you be on Medicare if you have a group health plan?
Even if you have a group health plan, Medicare is the primary insurer as long as you’ve been eligible for Medicare for 30 months or more. 4
How long do you have to be on Medicare for end stage renal disease?
If you have end-stage renal disease (ESRD) Even if you have a group health plan, Medicare is the primary insurer as long as you’ve been eligible for Medicare for 30 months or more. 4.
How long does it take for Medicare to kick in?
In that case, even if you did enroll in Medicare at age 65, it would be a secondary insurance and only kick in after your primary insurance paid its share of your claims. To avoid penalties after you (or your spouse) leave your job, you’ll need to enroll in Medicare within eight months. 9. If your employer has fewer than 20 employees, Medicare ...
What happens if you miss Medicare Part B?
If you miss this chance to enroll in Medicare Part B, you may face a late enrollment penalty.
What is primary for workers compensation?
Your workers’ compensation insurance will be primary for any services or items related to your workers’ compensation claim. Medicare will serve as your primary service for all covered medical expenses unrelated to that claim. 8
Is Medicare a secondary insurance?
While Medicare is the only insurance for some beneficiaries, it’s also common to have Medicare along with another type of insurance in order to reduce out-of-pocket costs. When that happens, there’s a predetermined coordination of benefits, in which one policy is the “primary insurance” and one is the “secondary insurance.” The primary insurance pays first, and the secondary insurance may then make additional payments before the policyholder owes money. That might include some portion of your deductibles or copayments, but it may not.
Is Medicare the only insurance?
While Medicare is the only insurance for some beneficiaries, it’s also common to have Medicare along with another type of insurance in order to reduce out-of-pocket costs. When that happens, there’s a predetermined coordination of benefits, in which one policy is the “primary insurance” and one is the “secondary insurance.”.
How many Medicare Supplement Plans are there?
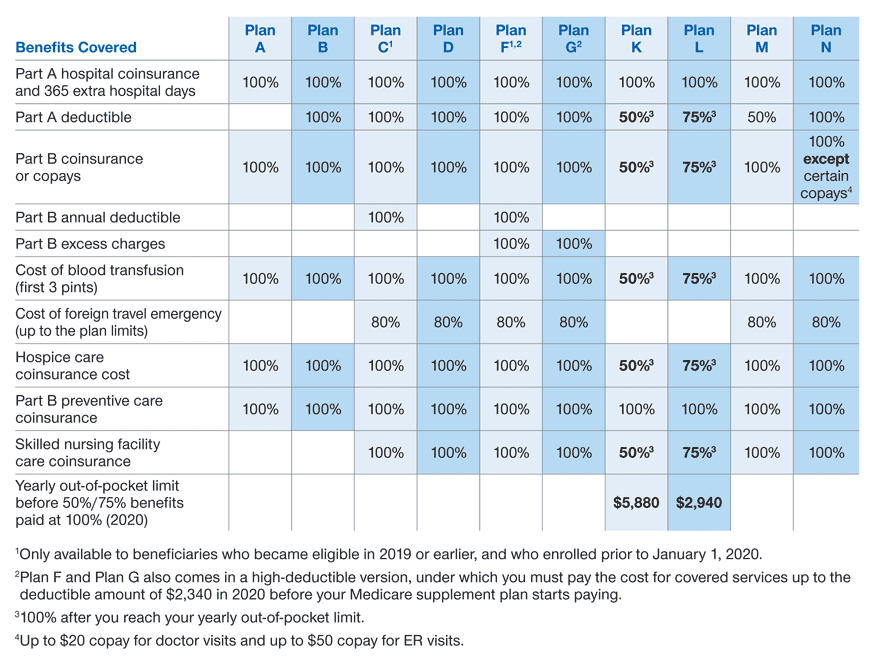
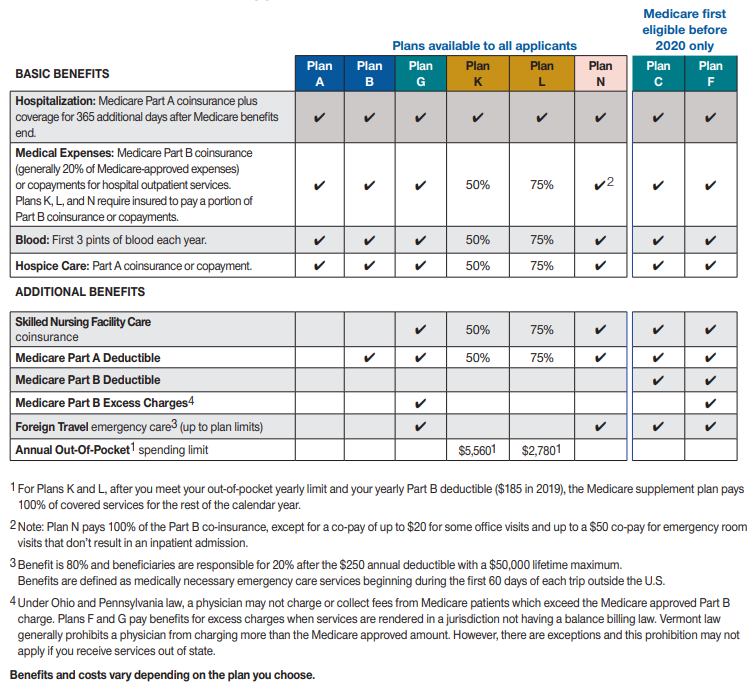
Medicare Supplement Plans, also called Medigap Plans, are standardized across most of the United States, though there are some exceptions. Each of the ten plans is designated a letter: A, B, C, D, F, G, K, L, M, and N. Though these plans are provided by private insurance companies, all plan types with the same letter must offer the same set ...
What does Medicare plan N cover?
Though both plans cover all of Medicare Part A coinsurance and hospital costs, as well as Part B coinsurance or copayments, Plan N may have copayments of up to $20 for some office visits, and some emergency room visits that don't result in hospital admissions may charge $50 in copayments. Other than that, both plans also cover the first three pints of blood, Part A hospice care copayments or coinsurance, and skilled nursing facility care coinsurance. However, Plan M only covers half of Part A's deductible, though Plan N covers it completely. Both M & N cover 80% of foreign travel emergencies.
What is the difference between Medicare Part A and Part B?
As mentioned above, they offer 100% coverage of Medicare Part A coinsurance and hospital costs, Part B coinsurance or copayments, the first three pints of blood, and Part A hospice care or copayments. The only difference between Plans A and B is that Plan B also covers Medicare Part A's deductible.
What is Medicare Advantage?
The first thing to do is understand the different options available to you. Medicare is available for people over 65, or who have certain types of conditions and receive Social Security Disability Insurance. They're divided into three parts: A, B, and C. Part A covers approved inpatient costs, and Part B focuses on providing approximately 80% of your outpatient costs. Part C (also called Medicare Advantage), isn't really separate health insurance, but rather allows private health insurance companies to provide Medicare benefits.
Does Medicare cover 80% of Part B?
Likewise, since Medicare typically only covers 80% of Part B coinsurance or copayments, all Medigap plans pay for some or all of the remaining 20% cost. This is also true for the first three pints of blood needed, and for Part A hospice care coinsurance or copayments.
Does Medicare cover coinsurance?
After that period, beneficiaries are charged ever-increasing fees until the 151st day, after which Medicare coverage ends. All Medigap plans pay for those copay fees, as well as 100% of an additional 365 days. Likewise, since Medicare typically only covers 80% of Part B coinsurance or copayments, all Medigap plans pay for some or all of the remaining 20% cost . This is also true for the first three pints of blood needed, and for Part A hospice care coinsurance or copayments.
Do all insurance plans have the same letter?
Though these plans are provided by private insurance companies, all plan types with the same letter must offer the same set of basic benefits, regardless the location. You'll see that there are some elements which are always covered, no matter what.
What is the difference between Medicare Advantage and Medicare Supplement?
Medicare Advantage vs Medicare Supplement: the basics. Medicare Supplement insurance plans go alongside Original Medicare and help pay for out-of-pocket costs not typically covered by Original Medicare. Since Original Medicare has no out-of-pocket maximum, a Medicare Supplement plan could give you a safety net against high medical costs ...
What is Medicare premium?
Premiums: A premium is an amount you pay monthly to have insurance, whether or not you use covered services. Some Medicare Advantage plans have premiums as low as $0 a month. However, you still must pay your Medicare Part B premium. Most Medicare Supplement insurance plans also have monthly premiums.
What are the benefits of Medicare Advantage?
When it comes to bonus benefits, Medicare Advantage plans more commonly include them. Medicare Advantage plans may cover the following benefits Medicare Part A and Part B typically don’t cover: 1 Routine vision, including eye glasses, contacts, and eye exams 2 Routine hearing, including hearing aids 3 Routine dental care 4 Prescription drugs and some over the counter medications 5 Fitness classes and gym memberships 6 Meal delivery to your home 7 Transportation to doctor visits 8 Other benefits
Does Medicare cover out of pocket expenses?
Medicare Supplement insurance plans generally only cover out-of-pocket costs, such as copayments, coinsurance, and deductibles, for services that Original Medicare already covers.
Do you have to pay deductible for Medicare Part B?
This combination of insurance is fairly comprehensive. You may have to pay deductible and copayment/coinsurance amounts. You generally pay separate premiums for Medicare Part B and for your Medicare Advantage plan, if it charges a premium.
Do you pay Medicare out of pocket?
You still may have some out-of-pocket Medicare costs. You generally pay separate premiums for Medicare Part B, Medicare Supplement insurance, and Medicare prescription drug coverage. If the above equation seems like too many pieces to put together, you may appreciate the simplicity of a Medicare Advantage plan.
Does Medicare Supplement cover prescription drugs?
Neither Original Medicare nor Medicare Supplement insurance plans typically cover the prescription drugs you take at home. If you want coverage for most prescription drugs, you will generally need to combine Original Medicare and a Medicare Supplement insurance plan with a stand-alone Medicare Part D prescription drug plan.