- Medicare managed care plans are offered by private companies that have a contract with Medicare.
- These plans work in place of your original Medicare coverage.
- Many managed care plans offer coverage for services that original Medicare doesn’t.
- Medicare managed care plans are often known as Medicare Part C or Medicare Advantage plans.
What are Medicare managed care plans?
Medicare managed care plans are an alternative to Original Medicare. Otherwise known as Medicare Advantage plans with many plan types, most are either HMOs or PPOs. Managed-care plans provide benefits for gaps in Parts A and B coverage. These alternative health-care plans make up Part C of Medicare.
Which managed care plan has the most restrictions?
The Health Maintenance Organization carries the most restrictions of all managed care plans. With no surprise, it’s also the least expensive option – making it the most popular. Receive care ONLY from within the plans’ network of providers.
What is the opposite of a managed care plan?
The opposite of a managed care plan would be a Medicare PFFS (private fee for service) plan. These plans do not utilize a primary care physician or require referrals to see specialists, and they generally do not include a network of health care providers.
What are the key objectives of Medicaid Managed Care?
Improvement in health plan performance, health care quality, and outcomes are key objectives of Medicaid managed care. Some states are implementing a range of initiatives to coordinate and integrate care beyond traditional managed care.
What part of Medicare contains the Medicare managed care plans?
Medicare Part CManaged care plans are also referred to as Medicare Part C (Medicare Advantage) plans. These plans cover everything original Medicare does, and they often cover additional services as well. For example, original Medicare doesn't cover routine dental care, but many managed care plans do.
Does Medicare have a managed care product?
Medicare Advantage is Medicare's managed care program. If you join Medicare Advantage, you get all your care through an HMO or PPO that has a contract with Medicare.
What is a Medicare MCO plan?
A Medicare managed care plan is one way to get coverage for the health care bills that Medicare doesn't pay. Medicare managed care plans are HMOs or PPOs that provide basic Medicare coverage plus other coverage to fill the gaps in Medicare coverage.
Which type of health insurance plan is considered a managed care plan?
A good example of a managed care plan is an HMO (Health Maintenance Organization). HMOs closely manage your care. Your cost is lowest with an HMO. You are limited to seeing providers in a small local network, which also helps keep costs low.
What is a managed care plan?
Managed care plans are a type of health insurance. They have contracts with health care providers and medical facilities to provide care for members at reduced costs. These providers make up the plan's network. How much of your care the plan will pay for depends on the network's rules.
Which is better PPO or HMO?
HMO plans typically have lower monthly premiums. You can also expect to pay less out of pocket. PPOs tend to have higher monthly premiums in exchange for the flexibility to use providers both in and out of network without a referral. Out-of-pocket medical costs can also run higher with a PPO plan.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
What is Medicare Fee for Service vs managed care?
Under the FFS model, the state pays providers directly for each covered service received by a Medicaid beneficiary. Under managed care, the state pays a fee to a managed care plan for each person enrolled in the plan.
What is the difference between traditional Medicare and managed Medicare?
With Original Medicare, you can go to any doctor or facility that accepts Medicare. Medicare Advantage plans have fixed networks of doctors and hospitals. Your plan will have rules about whether or not you can get care outside your network. But with any plan, you'll pay more for care you get outside your network.
What is the most popular form of managed care plans?
PPOs are also the most popular form of Managed Care (Health Insurance In-Depth). Point of Service (POS) medical care limits choice, but offers lower costs when compared to HMOs and PPOs. Generally an individual chooses a primary health care physician within a health care network.
How many types of managed care plan are there?
There are four main types of managed health care plans: health maintenance organization (HMO), preferred provider organization (PPO), point of service (POS), and exclusive provider organization (EPO).
What is PPO and HMO?
To start, HMO stands for Health Maintenance Organization, and the coverage restricts patients to a particular group of physicians called a network. 1. PPO is short for Preferred Provider Organization and allows patients to choose any physician they wish, either inside or outside of their network. 2.
What is Medicare managed care?
Medicare care managed care plans are an optional coverage choice for people with Medicare. Managed care plans take the place of your original Medicare coverage. Original Medicare is made up of Part A (hospital insurance) and Part B (medical insurance). Plans are offered by private companies overseen by Medicare.
What is Medicare Advantage?
Sometimes referred to as Medicare Part C or Medicare Advantage, Medicare managed care plans are offered by private companies. These companies have a contract with Medicare and need to follow set rules and regulations. For example, plans must cover all the same services as original Medicare.
What is a Medigap plan?
A Medigap plan, also known as Medicare supplement insurance, is optional coverage you can add to original Medicare to help cover out-of-pocket costs. Medigap plans can help you pay for things like: coinsurance costs. copayments. deductibles. These aren’t a type of managed care plan.
How much does Medicare cost in 2021?
Most people receive Part A without paying a premium, but the standard Part B premium in 2021 is $148.50. The cost of your managed care plan will be on top of that $148.50.
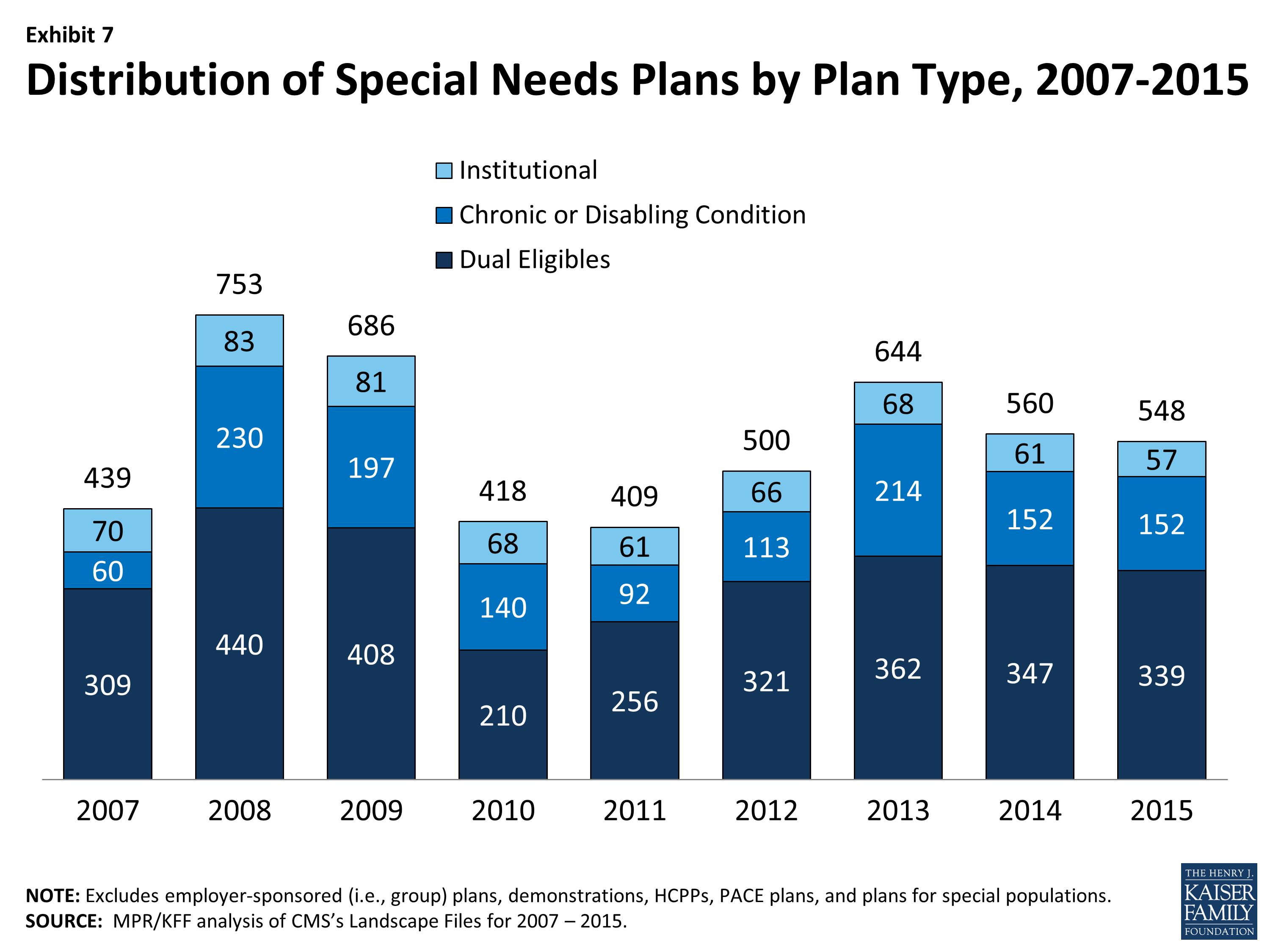
What is a SNP?
Special Needs Plan (SNP). An SNP is a managed care plan designed with a specific population in mind. SNPs offer additional coverage beyond a standard plan. There are SNPs for people with limited incomes, who are managing certain conditions, or who live in long-term care facilities.
What is a poor performer health plan?
you live in a “disaster area,” as declared by the Federal Emergency Management Agency (FEMA) — for example, if your area has been struck by a hurricane or other natural disaster. your current health plan is a “poor performer,” according to Medicare.
Does Medicare Part A cover managed care?
When you have a managed care plan, all your costs will be included. You don’t need to know whether Part A or Part B cover a service because your managed care plan will cover all the same things.
What is Medicare managed care?
A Medicare managed care plan is a type of Medicare Advantage plan. Learn what managed care plans are and how they could be a good fit for you. A Medicare managed care plan is one type of Medicare Advantage plan. The term “managed care plan” generally refers to HMO (health maintenance organization), PPO (preferred provider organization) ...
What is managed care network?
The networks of managed care plans often include pharmacies, which can help make ordering and filling prescriptions faster and easier for everyone involved . There’s less uncertainty about a beneficiary’s costs for care in a managed care plan, provided they stay within the assigned network for qualified services.
What is a HMO plan?
Health maintenance organization (HMO) In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. Preferred provider organization (PPO)
What are the different types of Medicare plans?
Types of Medicare managed care plans 1 Health maintenance organization (HMO)#N#In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. 2 Preferred provider organization (PPO)#N#In a Medicare PPO plan, you may or may not use a primary care physician, and you are typically not required to get a referral to see a specialist. You’ll have a network of providers from which to choose .You will generally can receive at least some coverage when receiving care outside of the network of providers, though your health care services may cost more than if you received them from a provider within your plan network. 3 Point of service (POS)#N#You can use a primary care physician in a Point of Service plan, as you would with an HMO plan. But as with a PPO plan, you can go outside of the plan network and still receive some coverage for services, though you may pay higher out-of-pocket costs than if you selected an in-network provider.
How to contact Medicare Advantage?
For more information about managed care plans or other types of Medicare Advantage plans, including plan benefits, eligibility, enrollment and availability, contact a licensed insurance agent by calling. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 24 hours a day, 7 days a week.
Why do you see a primary care physician?
Seeing a primary care physician allows patients to build a rapport with their doctor, and the doctor gets to know the patient’s health history firsthand . When a patient is referred to a specialist, there is communication between the primary care physician and the specialist regarding the patient’s health and treatment.
Can you use a primary care physician in a point of service plan?
But as with a PPO plan, you can go outside of the plan network and still receive some coverage for services, though you may pay higher out-of-pocket costs than if you selected an in-network provider.
