What are the Medicare enrollment periods?
Home/ Original Medicare/ Medicare Enrollment Periods Updated on October 25, 2021 There are many different types of Medicare Enrollment Periods. These enrollment periods fall into two categories. First, open enrollment is available to anyone eligible for Medicare. Then, Special Enrollment Periods.
Are you automatically enrolled in Medicare?
Individuals are automatically enrolled in Medicare if they: Are turning 65 and collect Social Security benefits. Have been receiving Social Security disability insurance for 24 months. Get SSDI because they have amyotrophic lateral sclerosis.
What happens if you miss the Medicare enrollment period?
The timeframe for enrolling in a Medicare plan is called an enrollment period. You have a seven-month window around the month you turn 65 to first sign up for a Medicare plan. If you miss the right time to enroll, your coverage may be delayed, or you could face penalties later on. And that may end up costing you more.
What are the special circumstances for delaying Medicare enrollment?
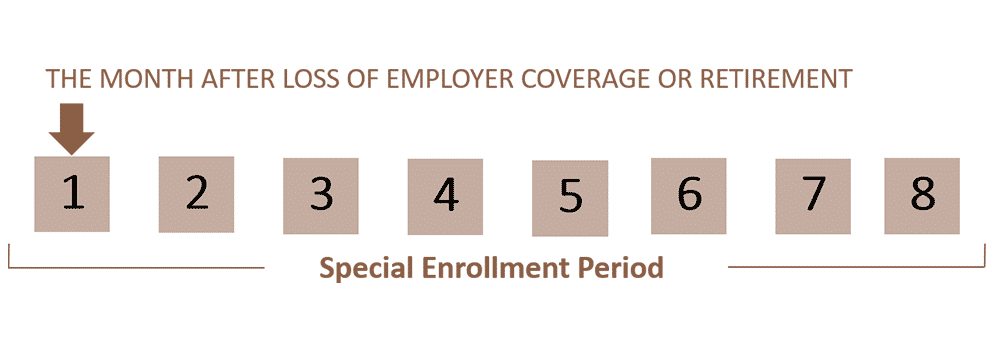
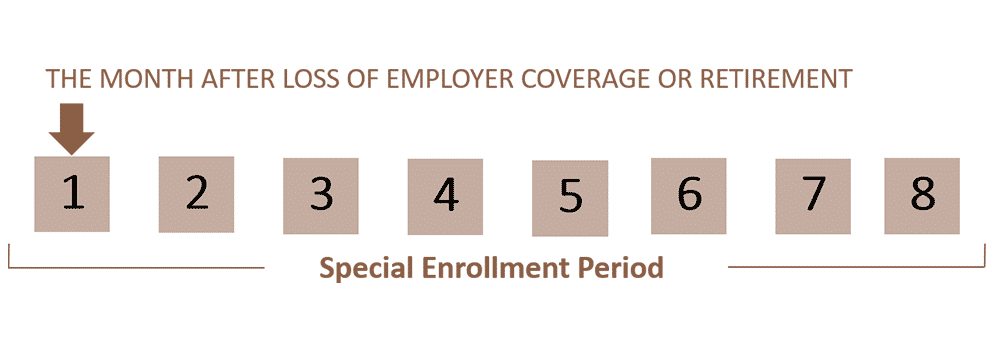
The most common special circumstance for delaying enrollment in Medicare is that the person is still working and covered by employer health insurance. An individuals SEP ends eight months after they lose group health insurance from a current employer.
What are the 3 Medicare enrollment periods?
When you turn 65, you have a seven month window to enroll in Medicare. This includes three months before the month you turn 65, your birth month, and three months after the month you turn 65.
What are the enrollment months for Medicare?
Between January 1-March 31 each year (General Enrollment Period) You can sign up between January 1-March 31 each year. This is called the General Enrollment Period.
What is the Medicare initial enrollment period?
Initial Enrollment Period – a 7-month period when someone is first eligible for Medicare. For those eligible due to age, this period begins 3 months before they turn 65, includes the month they turn 65, and ends 3 months after they turn 65.
Which of the following is not covered by Medicare?
does not cover: Routine dental exams, most dental care or dentures. Routine eye exams, eyeglasses or contacts. Hearing aids or related exams or services.
How long is enrollment period for Medicare Mcq?
During certain enrollment periods, such as the Initial Enrollment Period, 8- month Special Enrollment Period, and Special Enrollment Period, you may sign up for Medicare for the first time.
Do I have to enroll in Medicare every year?
In general, once you're enrolled in Medicare, you don't need to take action to renew your coverage every year. This is true whether you are in Original Medicare, a Medicare Advantage plan, or a Medicare prescription drug plan.
What does initial enrollment mean?
Initial Enrollment - This usually means that payment is still required in order to activate the policy, but documents have been approved. Active - The first premium payment has been made and the policy is active. Please note, there still may be documents required.
What is Medicare Sep?
You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
What is the initial coverage election period?
The ICEP, or the Initial Coverage Election Period, refers to the period during which people who are newly eligible for Medicare can enroll in a Medicare Advantage plan. During the ICEP, your clients can enroll in a Medicare Advantage health plan with or without prescription drug coverage.
Which of the following is not covered by Medicare Part A quizlet?
Medicare Part A covers 80% of the cost of durable medical equipment such as wheelchairs and hospital beds. The following are specifically excluded: private duty nursing, non-medical services, intermediate care, custodial care, and the first three pints of blood.
Which of the following services would not be covered under Medicare Part B?
Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing. Long-term supports and services can be provided at home, in the community, in assisted living, or in nursing homes.
Which type of care is not covered by Medicare quizlet?
Medicare Part A does not cover custodial or long-term care. Following is a breakdown of Part A SNF coverage, and the cost-sharing amounts that must be paid by the enrolled individual: -During the first 20 days of a benefit period, Medicare pays for all approved charges.
Your first chance to sign up (Initial Enrollment Period)
Generally, when you turn 65. This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65.
Between January 1-March 31 each year (General Enrollment Period)
You can sign up between January 1-March 31 each year. This is called the General Enrollment Period. Your coverage starts July 1. You might pay a monthly late enrollment penalty, if you don’t qualify for a Special Enrollment Period.
Special Situations (Special Enrollment Period)
There are certain situations when you can sign up for Part B (and Premium-Part A) during a Special Enrollment Period without paying a late enrollment penalty. A Special Enrollment Period is only available for a limited time.
Joining a plan
A type of Medicare-approved health plan from a private company that you can choose to cover most of your Part A and Part B benefits instead of Original Medicare. It usually also includes drug coverage (Part D).
What is Medicare enrollment period?
Let's unpack what you need to know about Medicare enrollment periods. An enrollment period is a window of time when you can make changes to your insurance plan. It's actually multiple periods because different circumstances call for different ways to enroll. Let's take a look at the different times to enroll. The initial enrollment period.
How long is the Medicare Supplement open enrollment period?
Medicare Supplement Open Enrollment Period. If you’re looking to supplement your Original Medicare coverage to help with additional costs, you have a six-month enrollment period that starts the first day of the month you turn 65 as long as you have signed up for Medicare Part B. This includes a 6-month window.
What is Medicare star rating?
The Medicare Star Ratings is an independent ratings system that allows consumers to evaluate plan performance on a number of factors. The Centers for Medicare and Medicaid Services created these star ratings for consumers. Learn more about Special Enrollment Periods.
How long does it take to enroll in Medicare?
Let's take a look at the different times to enroll. The initial enrollment period. When you turn 65, you have a seven month window to enroll in Medicare. This includes three months before the month you turn 65, your birth month, and three months after the month you turn 65.
When is the best time to buy Medicare Supplement?
If you’re looking to supplement your Original Medicare coverage to help with additional costs, the best time to buy a Medicare Supplement plan is during the six-month enrollment period that starts the first day of the month you turn 65 — as long as you have signed up for Medicare Part B.
What is the phone number for a spouse to sign up for Medicare?
Health insurance information (type and dates of coverage). If you are applying for a spouse or signing up for Medicare by phone (1-800-772-1213) or in person at the Social Security office, you may need to submit additional information.
Can you change your insurance plan outside of the enrollment period?
This period allows you to change plans outside of the annual enrollment period. It's usually based on a life event. For example, if you move outside your plan's area, or leave a job and lose your coverage, you may qualify to change or enroll in a new plan.