Who is eligible for Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance). You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and …
What if I’m not enrolled in Original Medicare automatically?
Two groups of people are eligible for Medicare benefits: adults aged 65 and older, and people under age 65 with certain disabilities. The program was created in the 1960s to provide health insurance for senior citizens.
What are the two parts of Medicare?
May 28, 2019 · Learn More To learn about Medicare plans you may be eligible for, you can:. Contact the Medicare plan directly. Call 1-800-MEDICARE (1-800-633-4227), TTY users 1-877-486-2048; 24 hours a day, 7 days a week. Contact a licensed insurance agency such as eHealth, which runs Medicare.com as a non-government website.
Why can’t I enroll in Medicare Part D?
To be eligible for premium Part A, an individual must be age 65 or older and be enrolled in Part B. Enrollment in premium Part A and Part B can only happen at certain times. (The section titled Enrollment Periods and When Coverage Begins explains the times when someone can enroll).
What group is not covered by Medicare?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Who is not automatically eligible for Medicare?
People who must pay a premium for Part A do not automatically get Medicare when they turn 65. They must: File an application to enroll by contacting the Social Security Administration; Enroll during a valid enrollment period; and.Dec 1, 2021
Which groups of patients are eligible for Medicare?
Medicare is the federal health insurance program for:People who are 65 or older.Certain younger people with disabilities.People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
Who is eligible for Medicare Australia?
To enrol as an Australian resident you need to have a permanent resident visa or have applied for one. To enrol in Medicare you need to prove you live in Australia. To enrol as an Australian citizen in Medicare you need to prove your identity and residency.Feb 25, 2022
Who is eligible for Medicare Part B reimbursement?
How do I know if I am eligible for Part B reimbursement? You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B. 2.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
How do you know if you qualify for Medicare?
You are eligible for Medicare if you are a citizen of the United States or have been a legal resident for at least 5 years and: You are age 65 or older and you or your spouse has worked for at least 10 years (or 40 quarters) in Medicare-covered employment.
What are Medicare Parts A & B?
Part A (Hospital Insurance): Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and home health care. Part B (Medical Insurance): Helps cover: Services from doctors and other health care providers. Outpatient care.
How to Enroll in Medicare and When You Should Start Your Research Process
Getting older means making more decisions, from planning for your kids’ futures to mapping out your retirement years. One of the most important dec...
Who Is Eligible to Receive Medicare Benefits?
Two groups of people are eligible for Medicare benefits: adults aged 65 and older, and people under age 65 with certain disabilities. The program w...
When Should You Enroll For Medicare?
Just because you qualify for something doesn’t mean you need to sign up, right? Not always. In the case of Medicare, it’s actually better to sign u...
Can You Delay Medicare Enrollment Even If You Are Eligible?
The short answer here is yes, you can choose when to sign up for Medicare. Even if you get automatically enrolled, you can opt out of Part B since...
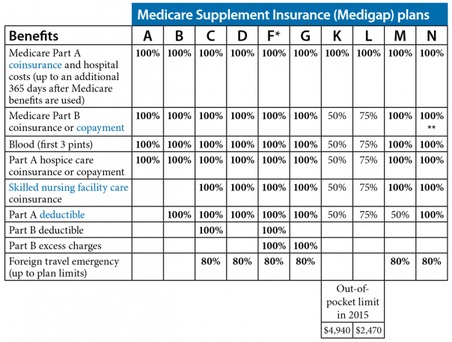
What About Medigap Plans?
Original Medicare covers a good portion of your care, but it’s not exhaustive. There’s a wide range of services that Parts A and B don’t cover, inc...
How long do you have to be a US citizen to qualify for Medicare?
To receive Medicare benefits, you must first: Be a U.S. citizen or legal resident of at least five (5) continuous years, and. Be entitled to receive Social Security benefits.
When do you sign up for Medicare Advantage?
Sign up for Medicare Advantage or Part D during the 7-month period that starts 3 months before the month you turn 65, includes your birthday month, and ends 3 months after your birthday month. Don’t have Medicare Part A, and you enrolled in Part B during general enrollment (January 1 to March 31)
Do you have to be 65 to get medicare?
Most people do. But once you turn 65, you become eligible for Medicare, a government-backed program designed specifically for seniors. There are also other reasons that you might be eligible for Medicare, which can muddy the waters when you’re researching your options for coverage.
How many parts are there in Medicare?
There are four parts to the program (A, B, C and D); Part C is a private portion known as Medicare Advantage, and Part D is drug coverage. Please note that throughout this article, we use Medicare as shorthand to refer to Parts A and B specifically.
When does Medicare open enrollment start?
You can also switch to Medicare Advantage (from original) or join a Part D drug plan during the Medicare annual open enrollment period, which runs from October 15 through December 7 each year. Eligibility for Medicare Advantage depends on enrollment in original Medicare.
Does Medicare cover ALS?
For people with ALS, Medicare enrollment is automatic and starts the same month as your disability benefits. To qualify for Medicare based on ESRD, you first need to meet the following qualifications: Your kidneys no longer work; You’ve had a kidney transplant or you need regular dialysis; and.
How long does it take to enroll in Medicare?
If you don’t get automatic enrollment (discussed below), then you must sign up for Medicare yourself, and you have seven full months to enroll.
How old do you have to be to get Medicare?
If you are age 65 or older, you are generally eligible to receive Medicare Part A (hospital insurance) and Medicare Part B (medical insurance) if you are a United States citizen or a permanent legal resident who has lived in the U.S. for at least five years in a row.
When do you get Medicare Part A and Part B?
If you meet Medicare eligibility requirements and you have received Social Security benefits for at least four months prior to turning age 65, you will typically get Medicare Part A and Part B automatically the first day of the month you turn age 65.
Is Medicare available to everyone?
Medicare coverage is not available to everyone. To receive benefits under this federal insurance program, you have to meet Medicare eligibility requirements. Find affordable Medicare plans in your area. Find Plans. Find Medicare plans in your area. Find Plans.
What is MEC in Medicare?
Medicare and Minimum Essential Coverage (MEC) Medicare Part A counts as minimum essential coverage and satisfies the law that requires people to have health coverage. For additional information about minimum essential coverage (MEC) for people with Medicare, go to our Medicare & Marketplace page.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
What age do you have to be to get a Social Security card?
Understanding the Rules for People Age 65 or Older. To be eligible for premium-free Part A on the basis of age: A person must be age 65 or older; and. Be eligible for monthly Social Security or Railroad Retirement Board (RRB) cash benefits.
How long does Part A coverage last?
If the application is filed more than 6 months after turning age 65, Part A coverage will be retroactive for 6 months. NOTE: For an individual whose 65th birthday is on the first day of the month, Part A coverage begins on the first day of the month preceding their birth month.
When do you get Part A?
An individual who is receiving monthly Social Security or RRB benefits at least 4 months prior to turning age 65 does not need to file a separate application to become entitled to premium-free Part A. In this case, the individual will get Part A automatically at age 65.
Do you have to pay Part A and Part B?
Also enroll in or already have Part B. To keep premium Part A, the person must continue to pay all monthly premiums and stay enrolled in Part B. This means that the person must pay both the premiums for Part B and premium Part A timely to keep this coverage. Premium Part A coverage begins prospectively, based on the enrollment period ...
What is the best Medicare plan?
We may use a few terms in this piece that can be helpful to understand when selecting the best insurance plan: 1 Deductible: This is an annual amount that a person must spend out of pocket within a certain time period before an insurer starts to fund their treatments. 2 Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. 3 Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is the difference between coinsurance and deductible?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%.
How long do you have to wait to get Medicare?
Some people with a disability do not need to wait until they reach the age of 65 to become eligible for Medicare. Those who have collected Social Security disability benefits for 24 months receive automatic enrollment into traditional Medicare, which comprises parts A and B. This article will examine the eligibility of people with a disability ...
Does Medicare cover nursing home stays?
Through Medicare, healthcare coverage for a person with a disability is identical to the coverage for an individual who qualifies because of their age . Areas of coverage include certain hospital and nursing home stays, along with doctor visits and community-based services.
How old do you have to be to get Medicare?
A person with a disability who is under 65 years of age may be eligible for Medicare. There are three groups of people eligible for Medicare if they are under the age of 65. The time frame in which each group becomes eligible differs as follows:
Does Medicare Part D include prescriptions?
Part D and Medicare Advantage costs. The coverage from parts A and B does not include prescription drug costs. Coverage for prescribed medication is known as Medicare Part D. A person may wish to include Part D as part of their plan, or they may decide to explore available options through Medicare Advantage.
How long does Medicare Part D last?
A person with a disability who wishes to enroll in either Medicare Part D or an Advantage plan may do so during: the 7-month period that begins 3 months before the 25th month of Social Security disability benefits . the 7-month period that includes the 25th month of disability benefits.
What is Medicare a federal program?
Medicare is a federal healthcare program that Americans pay into with taxes. It makes sense that the government would want to make sure that you have ties to the country before they allowed you access to that benefit.
How long does a disability last?
You have a disability that is expected to last longer than 12 months. This disability can be for any number of reasons but must be approved for Social Security Disability Insurance (SSDI) to be eligible for Medicare. You cannot sign up for Medicare until you have been on SSDI for 24 months.
Who is James Lacy?
James Lacy, MLS, is a fact checker and researcher. James received a Master of Library Science degree from Dominican University. Before you can take advantage of a Part D plan, you must first be eligible to sign up. There are specific criteria you need to meet in order to qualify for the program. 1 .
Is Medicare and Medicaid the same?
Millions of Americans are eligible for both Medicare and Medicaid every year. This dual eligibility may provide extra coverage to beneficiaries but with that comes extra regulation. It is important to note that both programs are managed by the same federal agency, the Centers for Medicare and Medicaid Services (CMS).
What is the second requirement for Medicare?
The second requirement for Medicare eligibility is to demonstrate medical need. Medicare leaves no room for interpretation here. You will be eligible for the program if you meet at least one of the following criteria.
What is MA PD?
There are Medicare Advantage Prescription Drug Plans (MA-PD plans) that include Part D coverage. In summary, you will need to have one of these Medicare plans or combinations to be eligible for Part D coverage: Part D + Part A. Part D + Part B. Part D + Original Medicare (Parts A and B) MA-PD. There are times you may be eligible for Medicare ...
What happens if you don't sign up for Medicare?
If you do not sign up yourself, you will be automatically enrolled in Original Medicare and a Part D plan by the government. You will have the option to change to a MA-PD or pick a different Part D plan at a later time. What It Means to Be Dual Eligible for Medicare and Medicaid.
What is EGWP in Medicare?
Group Medicare Advantage plans are also called employer group waiver plans (EGWP), pronounced “egg-whips.”. EGWPs are a type of Medicare Advantage plan offered by some employers to employees and retirees of some companies, unions, or government agencies. EGWPs may offer more benefits than traditional Medicare Advantage plans. EGWPs are often PPOs.
How many stars does Medicare Advantage have?
The Medicare Advantage Star Ratings program rates Medicare Advantage plans on a scale of up to five stars. Medicare Advantage considers plans that earn four or five stars to be high-quality. Other Medicare Advantage plan options.
Do you have to pay out of pocket for Medicare?
While the monthly premiums are low for Medicare, you will usually have an out-of-pocket limit for other costs as well. Other out-of-pocket costs may include: Copays . These are fees you pay for healthcare services at the time of care. You may have a copay every time you see a doctor on your plan.
What is EGWP insurance?
These Group Medicare Advantage plans are also called employer group waiver plans (EGWP), which insurance experts call “egg-whip.”. Many employers offer them to their retired or retiring employees. These Advantage plans may offer extra benefits to you as well as more relaxed enrollment guidelines. Keep reading to find out more about EGWPs, benefits ...
What is a PPO?
A PPO is a type of insurance in which you pay the lowest fees if you use preferred providers or in-network doctors, hospitals, and other healthcare providers. You can still use out-of-network providers, but you will have to pay more.
What is coinsurance in health insurance?
Coinsurance. Coinsurance is a percentage of the cost that you must pay for a medical service after your deductible has been met.
How old do you have to be to get medicaid?
For the most part, to be eligible for Medicaid you must be one of the following: Be age 65 or older. Have a permanent disability as that term is defined by the Social Security Administration. Be blind. Be a pregnant woman. Be a child, or the parent or caretaker of a child.
Does Medicaid pay for nursing home care?
That means that Medicaid can pay for all of the care you receive from the beginning of your stay in the nursing home. Although the special income level group is aimed at people who are in institutions such as nursing homes, states can use the same rules to make people eligible for home and community-based services.
Does medicaid cover long term care?
If you do not meet Medicaid's functional eligibility criteria, Medicaid will not cover long-term care services, regardless of financial eligibility. But, if you meet the general and financial requirements for eligibility, Medicaid will still cover other services such as doctor visits and prescription drugs.
What is the income limit for medically needy?
In most of the states that cover the medically needy, the income limit for an individual is less than $500 a month.