How does the federal government pay Medicare claims?
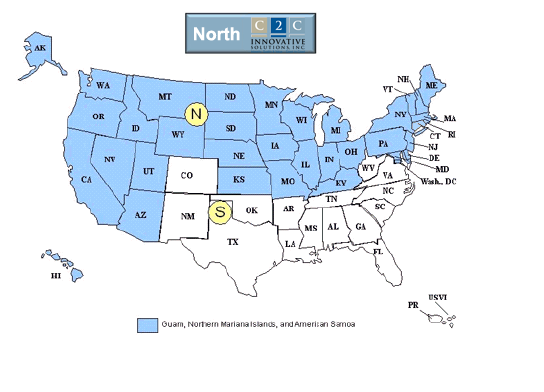
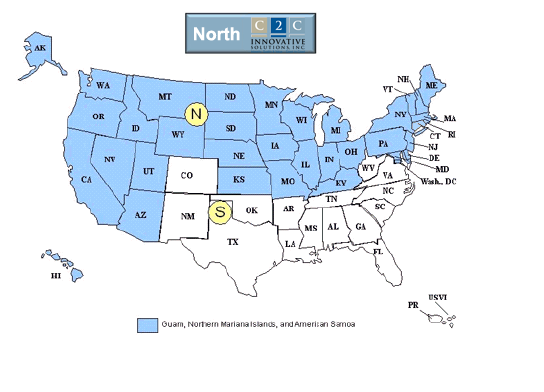
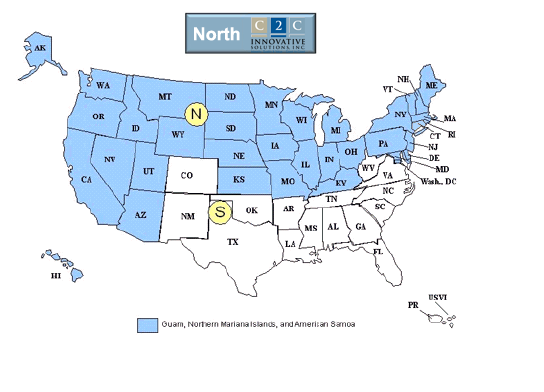
The federal government does not pay Medicare claims directly. Instead, it contracts with insurance organizations to process claims on its behalf. Insurance companies that process claims are called Medicare administrative contractors (MACs). Providers are assigned to a MAC based on the state in which they are physically located.
What does it mean when a provider accepts Medicare beneficiaries?
In the agreement between CMS and a provider, the provider agrees to accept Medicare beneficiaries for care and treatment. The provider cannot impose any limitations with respect to care and treatment of Medicare beneficiaries that it does not also impose on all other persons seeking care and treatment.
What is the Medicare claims processing manual Chapter 1?
Medicare Claims Processing Manual Chapter 1 - General Billing Requirements Table of Contents (Rev. 10840, 06-11-21) Transmittals for Chapter 1 01 - Foreword 01.1 - Remittance Advice Coding Used in this Manual 02 - Formats for Submitting Claims to Medicare 02.1 - Electronic Submission Requirements 02.1.1 - HIPAA Standards for Claims
How are physicians selected to participate in the Medicare program?
Annually, physicians choose whether they want to participate in the Medicare program. Participating physicians agree to accept assignment for all Medicare claims and to accept Medicare's allowed charge according to the Medicare Physician Fee Schedule as payment in full for services.
Why is Medicare conditional?
What is a POR in Medicare?
What is a CPN in BCRC?
What is conditional payment in Medicare?
What information is sent to the BCRC?
Can you get Medicare demand amount prior to settlement?
See more
About this website
Which organization can reference the Medicare Claims Processing Manual?
the National Uniform Claim Committee (NUCC)Providers sending professional and supplier claims to Medicare on paper must use Form CMS-1500 in a valid version. This form is maintained by the National Uniform Claim Committee (NUCC), an industry organization in which CMS participates.
Who processes Medicare claims in California?
Noridian Healthcare SolutionsNoridian Healthcare Solutions is the Medicare Administrative Contractor for California and is responsible for processing all Medicare fee-for-service Part A and B claims.
What agency operates Medicare?
The Centers for Medicare & Medicaid ServicesThe Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
How do providers submit claims to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Is national government services the same as Medicare?
National Government Services, Inc., a subsidiary of Anthem, Inc., has a long history of supporting federal health agencies, including the CMS . Throughout the country, NGS has served as a Medicare contractor since the inception of the Medicare Program over 56 years ago.
What is the role of the CMS?
The Centers for Medicare and Medicaid Services (CMS) is the U.S. federal agency that works with state governments to manage the Medicare program, and administer Medicaid and the Children's Health Insurance program.
What organization is responsible for overseeing Medicare quizlet?
CMS was formerly known as the Health Care Financing Administration (HCFA). contains CMS rules and regulations that govern the Medicare program.
What is the difference between the FDA and CMS?
Although FDA and CMS regulate different aspects of health care—FDA regulates the marketing and use of medical products, whereas CMS regulates reimbursement for healthcare products and services for two of the largest healthcare programs in the country (Medicare and Medicaid)—both agencies share a critical interest in ...
CMS Medicare’s Recovery Process | Guidance Portal
Medicare does not pay for items or services to the extent that payment has been, or may reasonably be expected to be, made through a liability insurer (including a self-insured entity), no-fault insurer or workers' compensation entity (Non-Group Health Plan (NGHP). When an accident/illness/injury occurs, you must notify the Benefits Coordination & Recovery Center (BCRC).
How to determine how much of a Medicare lien needs to be paid back. - Avvo
Once you have determined how much money Medicare has paid for medical bills related to your case it is time to determine how much you will have to pay them back. 42 CFR 411.37 is the Federal law which
I had surgery out of state. Why is Medicare refusing to pay?
On the other hand, the story may be different if you have a private Medicare Advantage (MA) plan. Your note makes reference to being out of your service area, so I’m guessing you have an MA plan.
CMS Medicare Secondary Payer Recovery Portal
The Medicare Secondary Payer Recovery Portal (MSPRP) is a web-based tool designed to assist in the resolution of liability insurance, no-fault insurance, and workers' compensation Medicare recovery cases. The MSPRP gives you the ability to access and update certain case specific information online.
Medicare Coverage for Inpatient Rehabilitation
Medicare covers inpatient rehabilitation in a skilled nursing facility and inpatient rehabilitation facility differently. Learn about the rules and costs.
Medicare's Interest in a Third Party Liability Settlement
Lump-sum commutation of future benefits. If a lump-sum compensation award stipulates that the amount paid is intended to compensate the individual for all future medical expenses required because of the work-related injury or disease, Medicare payments for such services are excluded until medical expenses related to the injury or disease equal the amount of the lump-sum payment.
Why is Medicare conditional?
Medicare makes this conditional payment so you will not have to use your own money to pay the bill. The payment is "conditional" because it must be repaid to Medicare when a settlement, judgment, award, or other payment is made.
What is a POR in Medicare?
A Proof of Representation (POR) authorizes an individual or entity (including an attorney) to act on your behalf. Note: In some special circumstances, the potential third-party payer can submit Proof of Representation giving the third-party payer permission to enter into discussions with Medicare’s entities.
What is a CPN in BCRC?
If a settlement, judgment, award, or other payment has already occurred when you first report the case, a CPN will be issued. A CPN will also be issued when the BCRC is notified of settlement, judgement, award or other payment through an insurer/workers’ compensation entity’s MMSEA Section 111 report. The CPN provides conditional payment information and advises you on what actions must be taken. You have 30 calendar days to respond. The following items must be forwarded to the BCRC if they have not previously been sent:
What is conditional payment in Medicare?
A conditional payment is a payment Medicare makes for services another payer may be responsible for.
What information is sent to the BCRC?
The information sent to the BCRC must clearly identify: 1) the date of settlement, 2) the settlement amount, and 3) the amount of any attorney's fees and other procurement costs borne by the beneficiary (Medicare may only take beneficiary-borne costs into account).
Can you get Medicare demand amount prior to settlement?
Also, if you are settling a liability case, you may be eligible to obtain Medicare’s demand amount prior to settlement or you may be eligible to pay Medicare a flat percentage of the total settlement. Please see the Demand Calculation Options page to determine if your case meets the required guidelines. 7.
What is noncompliance in Medicare?
Noncompliance will be considered in determining whether the provider is honoring its agreement, under which it may not charge for services for which payment may be made under the Medicare program.
What is M+CO in Medicare?
The provider must ascertain whether the patient is a member of a Medicare + Choice organization (M+CO). If the patient is a member of an M+CO, the provider must contact the M+CO specified by the patient or identified on the patient’s membership card, so the provider may determine whether to submit the claim to the M+CO.
What is encounter in medical?
The term “encounter” means a direct personal contact in the hospital between a patient and a physician, or other person who is authorized by State law and, if applicable, by hospital staff bylaws to order or furnish services for diagnosis or treatment of the patient. Direct personal contact does not include telephone contacts between a patient and physician. Nor is the compensation arrangement between the physician and the hospital relevant to whether an encounter has occurred. Patients will be treated as hospital outpatients for purposes of billing for certain diagnostic services that are ordered during or as a result of an encounter that occurred while such patients are in an outpatient status at the hospital. If a Medicare outpatient is referred to another provider or supplier for further diagnostic testing or other diagnostic services as a result of an encounter that occurs in this hospital, the hospital is responsible for arranging with the other entity for the furnishing of services. Hospitals are not required to verify that all ordered services are furnished but only to assure that, when it is necessary to refer a patient to an outside entity, the referral is made to a provider or supplier with which the referring hospital an arrangement. This requirement is necessary to assure that billing for services that are furnished is processed through the servicing hospital.
Can a provider collect a deductible?
The provider may collect deductible or coinsurance amounts only where it appears that the patient will owe deductible or coinsurance amounts and where it is routine and customary policy to request similar prepayment from non-Medicare patients with similar benefits that leave patients responsible for a part of the cost of their hospital services. In admitting or registering patients, the provider must ascertain whether beneficiaries have medical insurance coverage. Where beneficiaries have medical insurance coverage, the provider asks the beneficiary if he/she has a Medicare Summary Notice (MSN) showing his/her deductible status. If a beneficiary shows that the Part B deductible is met, the provider will not request or require prepayment of the deductible.
Why is Medicare conditional?
Medicare makes this conditional payment so you will not have to use your own money to pay the bill. The payment is "conditional" because it must be repaid to Medicare when a settlement, judgment, award, or other payment is made.
What is a POR in Medicare?
A Proof of Representation (POR) authorizes an individual or entity (including an attorney) to act on your behalf. Note: In some special circumstances, the potential third-party payer can submit Proof of Representation giving the third-party payer permission to enter into discussions with Medicare’s entities.
What is a CPN in BCRC?
If a settlement, judgment, award, or other payment has already occurred when you first report the case, a CPN will be issued. A CPN will also be issued when the BCRC is notified of settlement, judgement, award or other payment through an insurer/workers’ compensation entity’s MMSEA Section 111 report. The CPN provides conditional payment information and advises you on what actions must be taken. You have 30 calendar days to respond. The following items must be forwarded to the BCRC if they have not previously been sent:
What is conditional payment in Medicare?
A conditional payment is a payment Medicare makes for services another payer may be responsible for.
What information is sent to the BCRC?
The information sent to the BCRC must clearly identify: 1) the date of settlement, 2) the settlement amount, and 3) the amount of any attorney's fees and other procurement costs borne by the beneficiary (Medicare may only take beneficiary-borne costs into account).
Can you get Medicare demand amount prior to settlement?
Also, if you are settling a liability case, you may be eligible to obtain Medicare’s demand amount prior to settlement or you may be eligible to pay Medicare a flat percentage of the total settlement. Please see the Demand Calculation Options page to determine if your case meets the required guidelines. 7.