What screening labs are covered by Medicare?
Types of labs covered by Medicare include: doctors’ offices; hospital labs; independent labs; nursing facility labs; other institution labs
What lab tests are covered by Medicare?
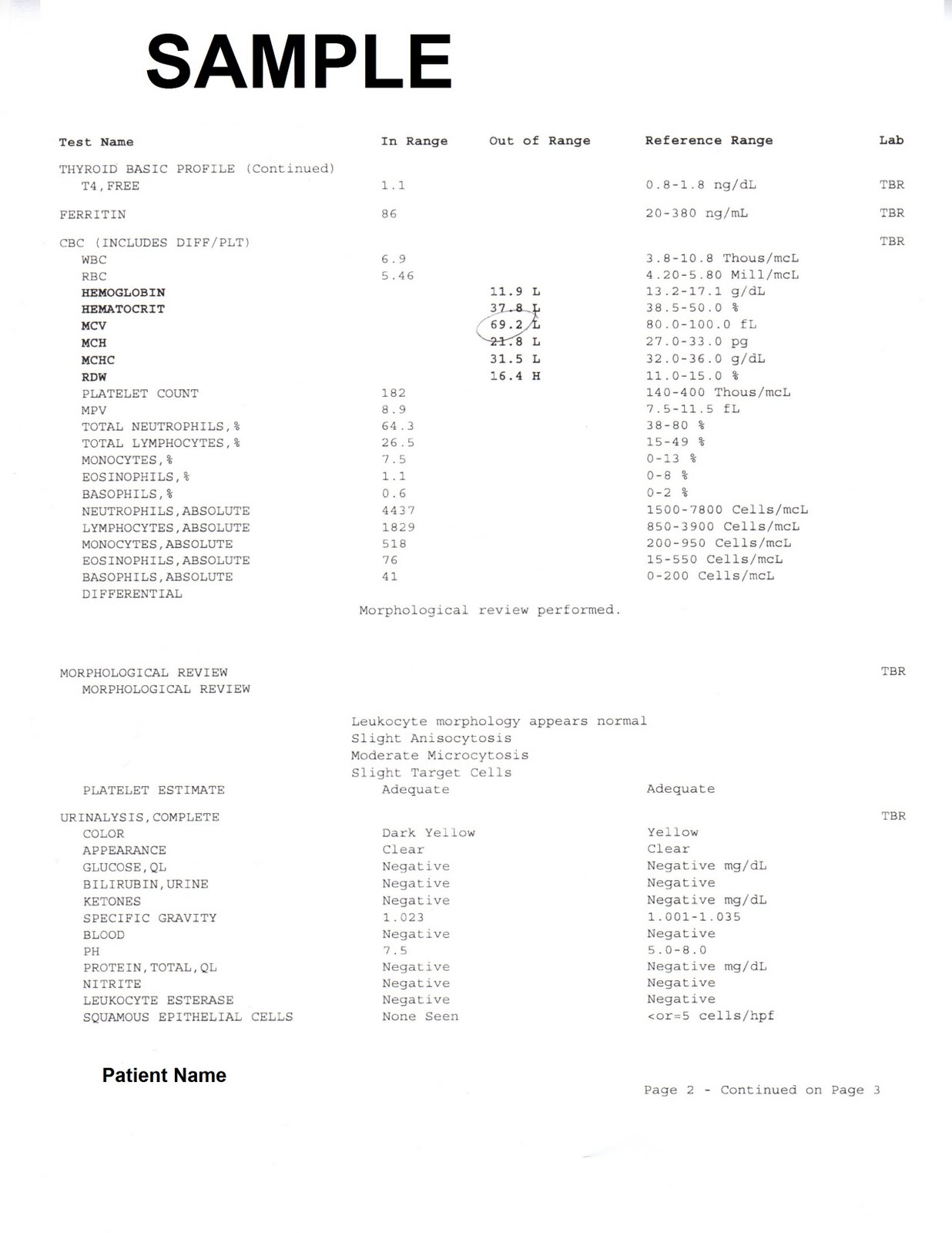
clinical diagnostic laboratory services when your doctor or practitioner orders them. You usually pay nothing for Medicare-approved clinical diagnostic laboratory services. Laboratory tests include certain blood tests, urinalysis, tests on tissue specimens, and some screening tests. A laboratory that meets Medicare requirements must provide them.
Are labs covered by Medicare?
When ordered by a physician, lab work is generally covered by Medicare Part B. Part B (Medical Insurance) helps cover medically necessary services and care in an outpatient setting, such as a doctor’s office.
What procedures are covered by Medicare?
Procedures Medicare does cover. Medicare Part A and Part B make up what is known as “Original Medicare.” Part A provides coverage for inpatient hospital services. Part B covers outpatient care and durable medical equipment (DME).
Does Medicare cover my lab test?
You usually pay nothing for Medicare-covered clinical diagnostic laboratory tests. Diagnostic laboratory tests look for changes in your health and help your doctor diagnose or rule out a suspected illness or condition. Medicare also covers some preventive tests and screenings to help prevent or find a medical problem.
Are labs covered under Medicare Part B?
Medicare benefits for lab work A physician's order for outpatient services and care, including lab work, is covered by Part B (Medical Insurance) as long as you see a Medicare-approved doctor that accepts the Medicare assignment and orders the appropriate test for diagnosis, treatment or monitoring.
How often does Medicare pay for a full blood workup?
For people watching their cholesterol, routine screening blood tests are important. Medicare Part B generally covers a screening blood test for cholesterol once every five years. You pay nothing for the test if your doctor accepts Medicare assignment and takes Medicare's payment as payment in full.
What blood tests are covered under preventive care?
Blood pressure, diabetes, and cholesterol tests. Many cancer screenings, including mammograms and colonoscopies. Counseling on such topics as quitting smoking, losing weight, eating healthfully, treating depression, and reducing alcohol use.
Does Medicare cover vitamin D blood test?
For Medicare beneficiaries, screening tests are governed by statute. Vitamin D testing may not be used for routine screening. Once a beneficiary has been shown to be vitamin D deficient, further testing is medically necessary only to ensure adequate replacement has been accomplished.
What is included in Medicare Part A?
In general, Part A covers:Inpatient care in a hospital.Skilled nursing facility care.Nursing home care (inpatient care in a skilled nursing facility that's not custodial or long-term care)Hospice care.Home health care.
Does Medicare pay for complete blood count?
The blood test must be deemed medically necessary in order to be covered by Medicare. Original Medicare (Medicare Part A and Part B) does not cover routine blood work as part of a general physical examination or screening.
What is the Medicare Part A for a skilled nursing facility?
If you’re formally admitted to a hospital or skilled nursing facility, your services will usually be covered by Medicare Part A (Hospital Insurance). While in a hospital, you will likely need to receive lab testing in order to stabilize, diagnose or treat a condition.
What is the first line of testing for disease?
More often than not, the first line of screening for signs of disease or infection may include lab work using blood samples or other bodily fluids.
Is lab work covered by Medicare?
When ordered by a physician, lab work is generally covered by Medicare Part B. Part B (Medical Insurance) helps cover medically necessary services and care in an outpatient setting, such as a doctor’s office. In order to be covered by Part B, you will need to visit a Medicare-approved physician who accepts assignment and orders ...
Does Medicare cover lab work?
Because of this, lab work that is sought out on your own will likely not be covered.
Does Medicare Supplement cover deductibles?
If you have Original Medicare and have purchased a Medicare Supplement (Medigap) policy, your policy may help cover the costs that Original Medicare does not , such as deductibles, copayments, or coinsurance.
Does Medicare Part A count against deductible?
You will likely be responsible for your annual deductible under Part A and Part B for most lab work services. Any type of medical billing to your Medicare coverage plan may count against your deductible. Medicare Part A and Part B both have different deductible amounts that may change annually.
What is Medicare Part A?
Medicare Part A offers coverage for medically necessary blood tests. Tests can be ordered by a physician for inpatient hospital, skilled nursing, hospice, home health, and other related covered services. Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines.
How often does Medicare cover mammograms?
once a year if you meet criteria. *Medicare covers diagnostic mammograms more often if your doctor orders them. You are responsible for the 20 percent coinsurance cost. Other nonlaboratory diagnostic screenings Medicare covers include X-rays, PET scans, MRI, EKG, and CT scans.
What is the purpose of blood test?
Blood tests are an important diagnostic tool doctors use to screen for risk factors and monitor health conditions. A blood test is generally a simple procedure to measure how your body is functioning and find any early warning signs. Medicare covers many types of blood tests. Trusted Source.
How much is Medicare Part B 2021?
You have to meet your annual deductible for this coverage as well. In 2021, the deductible is $203 for most people. Remember, you also have to pay your monthly Part B premium, which is $148.50 in 2021 for most beneficiaries.
Does Medicare cover 20 percent coinsurance?
You have to pay your 20 percent coinsurance as well as your deductible and any copays. Remember to go to providers that accept assignment to avoid charges Medicare won’t cover. Helpful links and tools. Medicare offers a tool you can use to check which tests are covered.
Does Medicare cover ABN?
Medicare offers a tool you can use to check which tests are covered. You can also go here to look through the list of covered tests from Medicare. You can look through lists of codes and items Medicare does not cover. Before signing an ABN, ask about the cost of the test and shop around.
Does Medicare Advantage cover blood work?
Medicare Advantage, or Part C, plans also cover blood tests. These plans may also cover additional tests not covered by original Medicare (parts A and B). Each Medicare Advantage plan offers different benefits, so check with your plan about specific blood tests. Also consider going to in-network doctors and labs to get the maximum benefits.
Does Medicare Cover LabCorp or Quest?
Medicare covers medically necessary lab tests from LabCorp and Quest. These are two large laboratories that provide outpatient laboratory testing.
What Screening Laboratory Tests Does Medicare Cover?
Medicare covers several laboratory tests, providing a doctor deems the test medically necessary. This means a doctor is screening or looking for a particular condition.
How Often Does Medicare Pay for Blood Work?
Medicare pays for medically necessary blood work a doctor orders, as well as screening laboratory testing. Medicare may limit how often you can have these tests and the amount they pay. Examples include:
How Much Does Medicare Pay for Blood Work?
Providing the test is medically necessary and covered under Medicare, you will pay nothing for Medicare-approved services once you have met your Part B deductible. For 2022, the Part B deductible is $233.
Does Medicare Part B Cover Lab Tests?
Medicare Part B will cover medically necessary laboratory tests, provided your doctor orders the test, and a Medicare-approved lab runs the test. Part B is the Medicare portion that covers medical services, including doctor’s visits.
How often does Medicare cover fecal occult blood test?
Fecal occult blood test. Medicare covers a fecal occult blood test once every 12 months for people aged 50 years or above. The test checks for blood in the stool that a person cannot see with the naked eye. If the result is positive, it may indicate that some part of the digestive tract is bleeding.
How often does Medicare cover a Pap?
Pap test. Medicare generally covers Pap tests every 2 years for females , though some situations may require more frequent tests. For example, if a person had an abnormal Pap test in the previous 3 years and is of child-bearing age or at high risk of certain cancers, Medicare covers a Pap test once per year.
What is Medicare Advantage?
Medicare Advantage, or Medicare Part C, offers an alternative to Medicare parts A, B, and D. Medicare Advantage consists of Medicare-approved, private insurance companies that must follow the guidelines and rules of Medicare. Like parts A and B, Medicare Advantage plans cover the costs of blood work and other tests.
What is a coinsurance for Medicare?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is a urinalysis test?
A urinalysis checks the acidity, color, and appearance of urine. It also measures substances not normally found in urine, such as blood and bacteria. This test helps a doctor diagnose urinary tract infections, diabetes, and kidney infections.
What is the BMP test?
The blood chemistry test, also called a Basic Metabolic Panel (BMP), usually measures components of the fluid portion of the blood. These measurements give doctors information about how the muscles, bones, and certain organs, such as the kidneys, are working.
What is a complete blood count?
A complete blood count helps detect clotting problems, immune system disorders, blood cancers, and blood disorders such as anemia. It measures: red blood cells, which transport oxygen to all parts of the body. white blood cells, which fight infections. platelets, which are the fragments that enable the blood to clot.
What is a laboratory in Medicare?
Under the final rule, in response to comments, a laboratory (as defined by CMS’s Clinical Laboratory Improvement Amendments of 1988 (CLIA) regulations), using its National Provider Identifier (NPI), is considered an applicable laboratory if more than 50 percent of its total Medicare revenues are received under the CLFS and PFS.
When will Medicare start paying for labs?
Private payor rates for laboratory tests from applicable laboratories will be the basis for the revised Medicare payment rates for most laboratory tests on the CLFS beginning in January 2018.
What is the Medicare 216A?
Section 216 (a) of the Protecting Access to Medicare Act of 2014 (PAMA) added section 1834A to the Social Security Act (the Act), which requires revisions to the payment methodology for clinical diagnostic laboratory tests paid under the Clinical Laboratory Fee Schedule (CLFS). Under the final rule, reporting entities will be required to report private payor payment rates for laboratory tests and the corresponding volumes of tests. Private payor rates for laboratory tests from applicable laboratories will be the basis for the revised Medicare payment rates for most laboratory tests on the CLFS beginning in January 2018.
What is an ADLT test?
The statute defines an ADLT as a laboratory test that is covered under Medicare Part B and is offered and furnished only by a single laboratory, that is not sold for use by a laboratory other than the original developing laboratory (or a successor owner), and that meets one of the following criteria:
How much does Medicare pay for CDLTs?
The CLFS provides payment for approximately 1,300 CDLTs, and Medicare pays approximately $7 billion per year for these tests.
How long is the CMS data collection period?
In the final rule, CMS responded to public comments by adopting a 6-month data collection period. The first data collection period will be from January 1 through June 30, 2016. The first data reporting period (that is, the period during which data from the collection period will be submitted to CMS) will be from January 1, 2017 through March 31, 2017. All subsequent data collection and reporting periods for CDLTs, except for ADLTs, will follow this same data collection and reporting schedule, every three years. Reporting of private payor rates for ADLTs will occur on the same schedule except it will be on an annual basis.
What is the HCPCS code?
Healthcare Common Procedure Coding System (HCPCS) codes are created by the American Medical Association (AMA) and CMS. The AMA creates Current Procedural Terminology (CPT) codes that are used primarily to identify medical services and procedures furnished by physicians, suppliers, and other health care professionals.