Who regulates Medicare supplement insurance plans?
Medicare Supplement Insurance plans are tightly regulated by the Centers for Medicare and Medicaid Services (CMS), a government agency. CMS determines what each letter plan will cover, and it requires each insurance company to offer the plan as is, without modifications.
Who are the companies that offer Medicare supplement insurance?
The following companies are our partners in Medicare Supplement Insurance: United Medicare Advisors, MedicarePlan.com, Mayberry Advisors, GoMedicare, and CoverRight. Medicare Supplement Insurance plans are tightly regulated by the Centers for Medicare and Medicaid Services (CMS), a government agency.
What is Medicare supplement insurance?
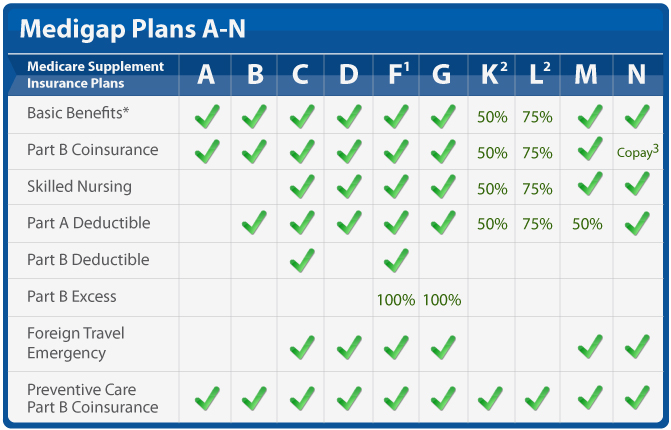
1 Medicare Supplement Insurance helps you manage out-of-pocket costs for covered services 2 Also called Medigap because it covers “gaps” in costs after Medicare Parts A and B pay their share 3 Medigap Plans C and F, which cover the Medicare Part B deductible, are being discontinued in 2020 Plus d'articles...
What Medicare supplement insurance plans does Medico sell?
Medico sells Medicare Supplement Insurance in 25 states and offers several popular Medigap plans, such as Plan A, Plan F, Plan G and Plan N. Medico offers a number of plan discounts for things like automatic premium withdrawal, being a non-smoker or living with another person over the age of 18.

Who is the largest Medicare supplement insurance company?
UnitedHealthCareAARP/United Health Group has the largest number of Medicare Supplement customers in the country, covering 43 million people in all 50 states and most U.S. territories. AARP licenses its name to insurer UnitedHealthCare, which helps make these policies so popular.
What is the common name for supplement Medicare insurance?
Medigap policiesservices and supplies. Medicare Supplement Insurance policies, sold by private companies, can help pay your share of some of the health care costs that Original Medicare doesn't cover, like copayments, coinsurance, and deductibles. Medicare Supplement Insurance policies are also called Medigap policies.
Are Medicare supplements regulated by state and federal government?
The California Department of Insurance (CDI) regulates Medicare Supplement policies underwritten by licensed insurance companies. The CDI assists consumers in resolving complaints and disputes concerning premium rates, claims handling, and many other problems with agents or companies.
Who has the cheapest Medicare supplement insurance?
What's the least expensive Medicare Supplement plan? Plan K is the cheapest Medigap plan, with an average cost of $77 per month for 2022.
What is the difference between a Medigap plan and a supplemental plan?
Summary: Medicare Supplement and Medigap are different names for the same type of health insurance plan – you can use either name. Medicare Supplement and Medigap are different names for the same type of health insurance plan – you can use either name.
What is the difference between Medigap and Medicare supplemental plans?
When you buy a Medicare Supplement insurance plan, you are still enrolled in Original Medicare, Part A and Part B. Medicare pays for your health-care bills primarily, while the Medigap plan simply covers certain cost-sharing expenses required by Medicare, such as copayments or deductibles.
What states do not offer Medicare Supplement plans?
Medigap plans are standardized across most states, meaning they offer the same benefits. The exceptions are Wisconsin, Minnesota and Massachusetts. Plans in those states may have options that differ from Medigap plans in other states.
What is the difference between a Medicare Advantage plan and a Medicare Supplement?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
Do you have to renew Medicare Supplement every year?
Medicare Supplement (Medigap) Plans: You do not have to do anything annually to renew them, and there is no annual open enrollment period for Medicare Supplement plans. They have the benefit of being “guaranteed renewable”. It will continue indefinitely unless you don't pay the premium.
What are the top 3 most popular Medicare Supplement plans in 2021?
Three Popular Medicare Supplement PlansBlue Cross Blue Shield. According to Blue Cross Blue Shield (BCBS), Plans F and N are available in most areas. ... AARP United Healthcare. The United Healthcare Medicare Supplement plan is also very popular. ... Humana.
How do I choose a Medicare Supplement plan?
Follow the steps below to purchase your Medigap plan:Enroll in Medicare Part A and Part B. ... Find which insurance companies in your state are licensed to sell Medigap plans by visiting Medicare.gov.Compare costs between companies. ... Select a Medigap plan that works best for you and purchase your policy.
What does Medicare supplemental cost?
Medicare Supplement Plans have premiums that cost anywhere from around $70/month to around $270/month. Typically, plans with higher monthly premiums will have lower deductibles. Plans with lower monthly premiums typically have higher deductibles.
What is a Medicare Supplement Plan?
A Medicare Supplement Plan, also called a Medigap plan, is a plan sold by private companies, separate from Medicare. Medicare Supplement plans pay for the costs, or “gaps,” in coverage that are not paid for by Original Medicare. These can include prescriptions, doctor visits, vision and dental care, and more.
How is Medicare Supplement Plan cost determined?
The cost of a Medicare Supplement plan is determined by the individual insurance company that sells it. When researching different companies, be sure to ask how they price their policies. 10 Learning which factors they base their pricing on will help you determine both the costs for you today and what to expect in the future if your health situation changes.
What is the Cigna app?
For those who are digitally inclined, Cigna offers three different apps through Google Play and the App store. The Cigna Envoy app helps customers access health benefits and resources specifically, while myCigna stores all your Cigna details, from your ID card information and account balances to cost comparisons for drugs and medical procedures. The Cigna Wellbeing app helps encourage healthy behaviors.
Why is AARP the best Medicare supplement?
We chose AARP as best for its set pricing for Medicare Supplement coverage because it doesn’t charge more as you grow older. This is especially helpful if you are still covered under your employer's insurance and may require coverage after the age of 65.
How long do you have to switch back to Medicare Advantage?
If you’re unhappy with your Advantage plan and switch back to a Medicare Original Plan (which you can do within 12 months of enrolling in the Medicare Advantage plan), you then become eligible for Medicare Supplement insurance.
When is the best time to buy a Medicare Supplement?
The best time to buy a Medicare Supplement policy is during your Initial Medicare Open Enrollment Period. This is a one-time only, six-month span when federal law allows you to sign up for any Medicare Supplement policy you want that is sold in your state. Preexisting conditions are accepted during this time period, and you can't be denied a Medicare Supplement policy or charged more due to past or present health problems. Make sure you know when your Open Enrollment Period starts. 12
What to do if you have a gap in Medicare?
If you’re experiencing a gap in coverage from Medicare, then you may need to choose supplemental coverage . Explore your options when it comes to finding out what coverage you’re lacking and if things like prescriptions, doctor visits, vision, and dental care are covered or if you need help paying for them. If you’re not fully covered, then consider purchasing supplemental insurance.
Does Medicare Supplement Insurance sell insurance?
The American Association for Medicare Supplement Insurance does NOT sell any insurance products.
Do AAMSI agents screen?
It's your choice who you contact (if anyone). To cover costs Insurance agents pay AAMSI a nominal fee to be listed on the directory and AAMSI does not screen or vet agents prior to them being posted.
Who sells Medicare Supplement Insurance?
Medicare Supplement Insurance plans (also called Medigap) are sold by dozens of private insurance companies all over the U.S. When shopping for coverage, it’s important to find the right plan for your unique needs and also to find the right insurance company. Different companies may sell Medigap plans that have different prices and terms, ...
When will Medicare Supplement Plan F be available?
Medicare Supplement Plan F and Plan C are not available for sale to Medicare beneficiaries who became eligible for Medicare on or after Jan. 1, 2020.
What is the number 13 Cigna?
Cigna. Cigna is ranked number 13 on the Fortune 500 list. 2. Depending on your location, the Medicare Supplement Insurance plans you may be able to apply for from Cigna* may include: Plan G. Plan N.
What states have Medigap plans?
Their costs and the availability of the types of plans, however, may vary. Medigap plans in Massachusetts, Minnesota and Wisconsin are standardized differently than they are in every other state. Learn more about Medigap plans in your state.
What is a BCBS?
Blue Cross Blue Shield (BCBS) is among the leading health insurance carriers in the U.S., and BCBS companies were the very first to work in conjunction with Medicare. There are now 36 different locally operated BCBS companies administering coverage in all 50 states.
Does Aetna offer Medigap?
Aetna offers a diverse portfolio of insurance products that includes Medigap plans. Over 1 million people trust Aetna for their Medicare Supplement Insurance. 3. Aetna offers several different types of Medigap plans. Plan availability may vary based on your location.
Is Wellcare the same as Medigap?
It’s important to keep in mind that although each company’s plan selection and pricing may differ, the coverage included in each type of Medigap plan remains the same, no matter where you purchase it.
Does Medicare pay for retirees?
Read 5 things you need to know about how retiree insurance works with Medicare. If you're retired, have Medicare and have group health plan coverage from a former employer, generally Medicare pays first. Your retiree coverage pays second.
Does Medicare Supplement Insurance cover health care?
Read about Medigap (Medicare Supplement Insurance), which helps pay some of the health care costs that Original Medicare doesn't cover.
Who regulates Medicare Supplement Insurance?
Medicare Supplement Insurance plans are tightly regulated by the Centers for Medicare and Medicaid Services (CMS), a government agency. CMS determines what each letter plan will cover, and it requires each insurance company to offer the plan as is, without modifications.
What is Medicare subsidized by?
In the simplest terms, Medicare is a health insurance plan subsidized by the federal government. It was originally created to help Social Security beneficiaries receive healthcare services, but it’s now been expanded to cover everyone who is:
What is a Medigap plan?
Also called Medigap because it covers “gaps” in costs after Medicare Parts A and B pay their share. Medigap Plans C and F, which cover the Medicare Part B deductible, are being discontinued in 2020. Sign up for Medigap during Open Enrollment to lock in the best premium for your plan. Our Approach.
What is covered by Plan A?
Plan A also covers 100% of coinsurances or copayments for hospice care services, 100% of Medicare Part B coinsurances or copayments for medical outpatient services, and 100% of the cost of the first three pints of blood you are administered during a procedure.
How much does Medicare pay for a doctor's visit?
Here’s an example with numbers: if the doctor’s visit had a Medicare-approved cost of $100, Medicare would pay $80, your Medigap would pay $15, and you would only have to pay $5.
What happens if you don't enroll in Medicare?
If you don’t enroll in Part A (inpatient hospital services) when you initially qualify, you may find yourself saddled with a 10% late enrollment penalty on your Part A premium. Says the Medicare website, “You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.”
How long do you have to be on Medicare if you have a disability?
If you have a disability and you’re receiving disability benefits from the Social Security Administration, you’ll automatically be enrolled in Parts A and B of Medicare once you’ve been receiving benefits for 24 months.
Why are Medicare Supplement plans selected?
The Medicare Supplement plan companies were selected, first and foremost, because they are able to show financial stability from information on their website, combined with third-party ratings such as those from AM Best—a reliable third party that provides credit ratings and financial data for the insurance industry.
Why was Medico selected?
Medico was selected primarily because of the cost-effectiveness of its Medicare Supplement policies (due to its many discounts offered) in combination with its financial rating (an A- rating from AM Best) and stability in offering insurance products since the 1930s.
What is Cigna insurance?
Cigna began in 1792 as the Insurance Company of North America and was the first-ever Marine insurer in the U.S. Today, Cigna, an 'A' (Excellent) rated company by AM Best, offers Medicare Supplement plans, as well as life, accident, and health insurance 9 .
What is Mutual of Omaha?
Mutual of Omaha’s United World Life, founded in 1983, is quickly becoming a leader in the Medigap insurance industry. The company offers a wide range of products, including many Medicare supplement plans.
How long does it take for Medicare to process a claim?
In fact, the company claims that it pays 98% of all Medicare claims within 12 hours. According to Insurance.com, it takes the average insurance company 30 days to process claims. 5 As far as its financial strength, the company has an A+ rating with AM Best. 6.
Why is it so difficult to estimate the average cost of Medicare?
Note that it is difficult to estimate an average cost for a Medicare plan because there are so many variables that can dramatically impact the cost. Whether the company offers insurance rates based on age/gender or not, there are several types of policies, including:
What is additional premium discount?
Additional premium discounts are offered when you pay your premiums via automatic bank payments from your checking or savings account.
What is Medicare Supplement Plan?
A Medicare Supplement Plan (also called a Medigap plan) can help pay Medicare Part A and Part B costs, such as deductibles, copayments, and coinsurance. If you’re eligible for a Medicare Supplement Plan, enrollment is a good idea, as these plans take much of the worry out of escalating medical costs by having no cap on the coverage they offer.
How old do you have to be to get Medicare Supplement?
You must be age 65 or older (in several states, some Plans are offered to those under 65 who are on disability). You must reside in the state in which ...
How long do you have to wait to buy a Medigap policy?
Under certain circumstances, there is a waiting period of up to six-months for pre-existing conditions for Medigap policies purchased during the OEP.
When does Medigap OEP start?
If you delay Part B coverage, your Medigap OEP will be the six-month period beginning on the first day of the month you enroll in Part B. Example 1: If you turn 65 on May 1 and your Part B begins May 1, your Medigap OEP begins May 1 and runs through October 31. Example 2: If you turn 65 on May 1, 2020 but wait until your Employer Group Coverage ...
When do you join a Medicare Advantage Plan?
You joined a Medicare Advantage Plan when you first became eligible for Medicare and disenrolled within 12 months, or your previous Medigap policy, Medicare Advantage Plan, or PACE program ends its coverage or committed fraud. If you have a Medicare Advantage Plan, Medicare SELECT policy, or PACE program and you move out of the plan’s service area, ...
When is the best time to buy a Medigap policy?
The best time to buy a Medigap policy is during your Medigap Open Enrollment Period. OEP is the six-month period that begins on the first day of the month in which you’re 65, or older, and enrolled in Medicare Part B. If you delay Part B coverage, your Medigap OEP will be the six-month period beginning on the first day of ...
What is SEP medical underwriting?
Included in the SEP category is the SEP for relocation to the U.S. from a foreign country.
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
How many people did Medicare cover in 2017?
programs offered by each state. In 2017, Medicare covered over 58 million people. Total expenditures in 2017 were $705.9 billion. This money comes from the Medicare Trust Funds.
What is covered by Part A?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents.
What is the CMS?
The Centers for Medicare & Medicaid Services ( CMS) is the federal agency that runs the Medicare Program. CMS is a branch of the. Department Of Health And Human Services (Hhs) The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, ...
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. and. Medicare Drug Coverage (Part D) Optional benefits for prescription drugs available to all people with Medicare for an additional charge.
Does Medicare cover home health?
Medicare only covers home health care on a limited basis as ordered by your doctor. , and. hospice. A special way of caring for people who are terminally ill. Hospice care involves a team-oriented approach that addresses the medical, physical, social, emotional, and spiritual needs of the patient.
