You're eligible for a Medicare supplement guaranteed issue right if: You no longer live in the Medicare Advantage plan's service area. The organization offering your Medicare Advantage coverage lost certification to sell the plan.
Full Answer
Are you eligible for Medicare supplement coverage?
If you’re under 65 and have Medicare because of disability, end-stage renal disease, or amyotrophic lateral sclerosis, your eligibility for Medicare Supplement coverage may depend on the state that you live in.
What are my Medicare supplement guaranteed-issue rights?
Outside of your Medicare Supplement OEP, guaranteed-issue rights are often limited to six Medicare Supplement insurance plans: A, B, C, F, K, or L. This excludes the four additional plans, D, G M, and N, which are offered in most states during your Medicare Supplement Open Enrollment Period.
Who is eligible for Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
Do Medicare supplement insurance plans require medical underwriting?
There are two situations where you won’t be subjected to medical underwriting when applying for a Medicare Supplement insurance plan. The first situation is during your Medicare Supplement Open Enrollment Period (OEP), which lasts for six months and starts when you are both 65 or older and enrolled in Medicare Part B.
What is a qualifying reason for a Medigap guaranteed issue right?
You have a guaranteed issue right (which means an insurance company can't refuse to sell you a Medigap policy) in these situations: You're in a Medicare Advantage Plan, and your plan is leaving Medicare or stops giving care in your area, or you move out of the plan's service area.
Who would be most qualified for Medicare supplement insurance?
Who Is Eligible for a Medicare Supplement Insurance Plan?Aged 65 and older.Diagnosed with end stage renal disease (ESRD – permanent kidney failure requiring dialysis or transplant)Receiving disability benefits from the Social Security Administration or the Railroad Retirement Board.More items...
Can I be denied a Medicare Supplement plan?
For the most part, Medicare Supplement policies are guaranteed renewal. This means as long as you pay the monthly premium, you cannot be denied coverage once you enroll in a plan, regardless of any health conditions that may arise.
What is the difference between open enrollment and guaranteed issue?
Whereas in open enrollment, you can choose any Medigap plan that is offered in your state, during a guaranteed issue you can typically only choose Medigap Plans A, B, C, F, K or L that's sold in your state by any insurance company.
How long is the guaranteed issue period for Medicare Supplement?
63 daysIf you joined Medicare Advantage when you first became eligible for Medicare, but decided to switch to Original Medicare within the first 12 months, you have Medicare Supplement guaranteed issue rights for 60 days before your plan ends and 63 days after you switch.
Who has the cheapest Medicare Supplement insurance?
What's the least expensive Medicare Supplement plan? Plan K is the cheapest Medigap plan, with an average cost of $77 per month for 2022.
When can someone enroll in a Medicare Supplement without the chance for denial premium increase or exclusions due to pre-existing conditions?
Coverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded.
Is Medigap plan G guaranteed issue?
Medigap Plan G is only available as a guaranteed issue plan to people who became eligible for Medicare on or after January 1st, 2020. You may still apply for Medigap Plan G through the usual methods (link to article) if you entered Medicare before 2020, but your acceptance may not be guaranteed.
Do pre-existing conditions apply to Medicare Supplement plans?
Summary: A Medicare Supplement insurance plan may not deny coverage because of a pre-existing condition. However, a Medicare Supplement plan may deny you coverage for being under 65. A health problem you had diagnosed or treated before enrolling in a Medicare Supplement plan is a pre-existing condition.
Why is guaranteed issue beneficial?
Guaranteed Issue Life Insurance FAQ Guaranteed issue life insurance is a policy you can't be turned down for. It's appealing because there's no life insurance medical exam needed to qualify, and no health questions. The downside is that it generally has high costs and only low amounts of coverage available.
What does guaranteed issue mean and why is this potentially very beneficial?
A requirement that health plans must permit you to enroll regardless of health status, age, gender, or other factors that might predict the use of health services.
Is Plan G guaranteed issue in 2021?
First of all, Plan G is not offered as a “guaranteed issue” (no health questions) option in situations where someone is losing group coverage or Medicare Advantage plan coverage.
What is the most popular Medigap plan in 2021?
Medigap Plans F and G are the most popular Medicare Supplement plans in 2021.
What is the best Medicare company to go with?
Best Medicare Supplement Insurance companiesBest for Medigap plan options: AARP/UnitedHealthcare.Best for member satisfaction: Mutual of Omaha.Best for low premiums: Aetna.Best for extra benefits: Anthem.Best for nationwide availability: Blue Cross Blue Shield.
What company has the best Medicare coverage?
List of Medicare Advantage plansCategoryCompanyRatingBest overallKaiser Permanente5.0Most popularAARP/UnitedHealthcare4.2Largest networkBlue Cross Blue Shield4.1Hassle-free prescriptionsHumana4.01 more row•Feb 16, 2022
Who is the largest Medicare provider?
Standout feature: UnitedHealthcare offers the largest Medicare Advantage network of all companies, with more than 1 million network care providers. UnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.
When Am I Eligible For Medicare Supplement Coverage?
Because Medicare Supplement policies complement your Original Medicare coverage, you must be enrolled in Part A and Part B to be eligible for this...
How Can Enrollment Periods Affect My Eligibility For Medicare Supplement Plans?
The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period—for most people, this per...
Am I Eligible For A Medicare Supplement Plan If I’M Under Age 65?
Federal law does not require insurance companies to sell Medicare Supplement policies to people under 65, but many states do have this requirement....
Am I Eligible For A Medicare Supplement Plan If I Have A Medicare Advantage Plan?
Medicare Supplement policies don’t work with Medicare Advantage plans. If you decide to switch from Original Medicare to a Medicare Advantage plan,...
Am I Eligible For A Medicare Supplement Plan If I Have Coverage Through Medicaid?
While some beneficiaries may be eligible for both Medicare and Medicaid benefits (also known as “dual eligibles”), Medicaid typically doesn’t work...
How long does Medicare Supplement open enrollment last?
How can enrollment periods affect my eligibility for Medicare Supplement plans? The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period —for most people, this period starts the month that you turn 65 and have Medicare Part B, and goes for six months.
How long do you have to wait to get Medicare Supplement?
Keep in mind that even though a Medicare Supplement insurance company cannot reject your enrollment for health reasons, the company is allowed to make you wait up to six months before covering your pre-existing conditions.
How long is a trial period for Medicare Advantage?
Trial rights allow you to join a Medicare Advantage plan for a one-year trial period if you are enrolling in Medicare Part C for the first time. If you’re not happy with the plan, you can return to Original Medicare anytime within the first 12 months.
Can you change your Medicare Supplement plan if it goes bankrupt?
For example, if your Medicare Supplement insurance company goes bankrupt or misleads you, you may be able to change Medicare Supplement plans with guaranteed issue.
Can you get Medicare Supplement if you have health issues?
This is when you can get any Medicare Supplement plan that’s available in your area, regardless of any health issues you may have. The insurance company can’t charge you more if you have health problems or deny you coverage because of pre-existing conditions.
Does Medigap cover prescriptions?
Since Medigap plans don’t include prescription drug benefits, if you’re enrolled in Original Medicare and want help with prescription drug costs, you can get this coverage by enrolling in a stand-alone Medicare Prescription Drug Plan.
Does Medicare Supplement include prescription drug coverage?
In addition, keep in mind that Medicare Supplement plans don’t include prescription drug benefits (Medicare Part D). In the past, some Medicare Supplement plans may have included this coverage, but plans sold today don’t include prescription drug benefits. If you have an older Medicare Supplement policy with prescription drug coverage, ...
How old do you have to be to get Medicare Supplement?
In most states you need to be 65 years or older; however, insurance carriers in a few states offer at least one Medicare Supplement to Medicare beneficiaries under 65 years. Anyone who is at least 65 years old and enrolled in Medicare Parts A & B is eligible for Medigap.
When do seniors have to enroll in Medicare Supplement?
Many seniors will have automatic enrollment in Part A when turning 65. In some cases, beneficiaries automatically enroll in Part B. Once you’ve acquired Original Medicare, you can use your Medicare Supplement Open Enrollment Period to select a Medicare Supplement policy. The best part, when you enroll during this period, ...
What insurance does Medicare offer to people under 65?
The policy that is usually available to Medicare beneficiaries under 65 is Medigap Plan A. Insurance companies know that beneficiaries under 65, receiving Medicare are likely on disability. Those on disability are a higher risk for claims because they need more ...
How old do you have to be to get medicare in 2021?
You also must be enrolled in Part A and Part B. In most states you need to be 65 years or older; however, insurance carriers in a few states offer at least one Medicare Supplement ...
How long does Medigap coverage last?
The best part, when you enroll during this period, there’s no medical underwriting. This only happens once in a beneficiary’s lifetime and lasts for 6 months. Those new to Medicare have the best opportunity when it comes to Medigap eligibility. Taking advantage of top-quality coverage at the lowest price is the opportunity every beneficiary has ...
What happens if you have a supplement secondary to Medicare?
If you have an employer-sponsored supplement secondary to Medicare, and that policy ends; you’ll reap the benefits of Guaranteed Issue rights.
Can Medicare Advantage plan beneficiaries switch to Medigap?
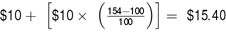
Medicare Advantage plan beneficiaries can switch to Medigap if they increased the copayments or premium by 15 percent or more, stopped offering the plan, ends their relationship with your provider, or reduced benefits.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
When will Medicare plan C and F be available?
However, if you were eligible for Medicare before January 1, 2020 but not yet enrolled, you may be able to buy Plan C or Plan F.
What happens if a Medigap insurance company goes bankrupt?
Your Medigap insurance company goes bankrupt and you lose your coverage, or your Medigap policy coverage otherwise ends through no fault of your own.
How long does Medigap coverage last?
No later than 63 calendar days after your coverage ends. note: Your rights may last for an extra 12 months under certain circumstances. Your Medigap insurance company goes bankrupt and you lose your coverage, or your Medigap policy coverage otherwise ends through no fault of your own. You have the right to buy:
What is a guaranteed issue?
Guaranteed Issue Rights (Also Called "Medigap Protections") Rights you have in certain situations when insurance companies are required by law to sell or offer you a Medigap policy . In these situations, an insurance company can't deny you a Medigap policy, or place conditions on a Medigap policy, ...
How long before Medicare coverage ends?
As early as 60 calendar days before the date your coverage will end. No later than 63 calendar days after your coverage ends. Call the Medicare SELECT insurer for more information about your options. Find the phone number for the Medicare SELECT company.
How long after Medicare coverage ends can you start Medigap?
No later than 63 calendar days after your coverage ends. Medigap coverage can't start until your Medicare Advantage Plan coverage ends. You have Original Medicare and an employer group health plan (including retiree or COBRA coverage) or union coverage that pays after Medicare pays and that plan is ending.
What is Medicare Supplement?
A Medicare Supplement gives you predictable out of pocket costs once you are on Medicare and limits, or eliminates, your exposure to potentially high medical costs. But, if you don’t sign up for one when you are eligible to do so, you may have difficulty getting a plan at a later time. Because of this, it’s important to understand ...
What is guaranteed issue for Medicare?
A different type of eligibility for Medicare Supplement coverage is called Medicare Supplement guaranteed issue. Guaranteed issue periods have the same basic implications as the Medigap open enrollment period, in that you cannot be turned down for coverage or made to pay more based on your health. However, there are some additional considerations.
How long do you have to be in Medicare before you can enroll?
Additionally, most insurance companies allow you to enroll in a Medigap plan up to 6 months before your Medicare coverage starts. When you do that, the coverage does not start ...
How long is Medicare Supplement Open Enrollment?
What is Medicare Supplement Open Enrollment? Open enrollment, as it pertains to Medicare Supplement plans, is a 6 month period that begins the first day of the month that you are both 65 or older and enrolled in Medicare Part B (see page 14 of the “Choosing a Medigap” booklet ).
What is 65Medicare.org?
65Medicare.org is a leading, independent Medicare insurance agency for people turning 65 and going on Medicare. If you have any questions about this information, you can contact us online or call us at 877.506.3378.
What are insurance companies asking about?
Generally speaking, most insurance companies are asking about the last 2-3 years and asking about things like cancer, heart attacks, stroke, insulin-dependent diabetes, COPD, multiple hospitalizations, and known/upcoming medical tests/procedures.
Can you get a Medigap plan in your state?
If you are in your open enrollment period, that means that you can get any Medigap plan that is sold in your state without any pre-existing conditions restrictions or exclusions. Insurance companies cannot refuse to sell you any Medigap policy that they offer, and they cannot charge you more based on your health.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
Does Medicare cover prescription drugs?
Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage. If you want prescription drug coverage, you can join a Medicare Prescription Drug Plan (Part D). If you buy Medigap and a Medicare drug plan from the same company, you may need to make 2 separate premium payments. Contact the company to find out how to pay your premiums.
Does Medigap cover everything?
Medigap policies don't cover everything. Medigap policies generally don't cover. long-term care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
When did Medicare start providing prescription drugs?
Since January 1, 2006, everyone with Medicare, regardless of income, health status, or prescription drug usage has had access to prescription drug coverage. For more information, you may wish to visit the Prescription Drug Coverage site.
How long do you have to be on disability to receive Social Security?
You have been entitled to Social Security or Railroad Retirement Board disability benefits for 24 months. ( Note: If you have Lou Gehrig's disease, your Medicare benefits begin the first month you get disability benefits.)
How long do you have to buy Medicare Supplement?
Also keep in mind that in most situations you must buy your Medicare Supplement insurance plan within 63 calendar days of your previous coverage ending. Calendar days include weekends, so don’t put off your application too long. When your guaranteed-issue period expires, then you may be subjected to medical underwriting when applying for a Medicare Supplement insurance plan.
How long does Medicare Supplement Open Enrollment Period last?
The first situation is during your Medicare Supplement Open Enrollment Period (OEP), which lasts for six months and starts when you are both 65 or older and enrolled in Medicare Part B. The second situation is if you have guaranteed-issue rights.
How long after Medicare coverage ends can you buy it?
What you can do with guaranteed issue: As early as 60 calendar days before the date your coverage will end but no later than 63 days after your coverage ends, you have the right to buy any Medicare Supplement insurance plan listed above that is sold in your state by any insurance company.
What are guaranteed issue rights?
What are Guaranteed-Issue Rights? Guaranteed-issue rights may protect you from medical underwriting. Health insurance companies often use your health history and data on pre-existing conditions* to make determinations about whether or not they will cover you and how much they will charge you for coverage.
How old do you have to be to get Medicare?
If you are age 65 or older, you are generally eligible to receive Medicare Part A (hospital insurance) and Medicare Part B (medical insurance) if you are a United States citizen or a permanent legal resident who has lived in the U.S. for at least five years in a row.
When do you get Medicare Part A and Part B?
If you meet Medicare eligibility requirements and you have received Social Security benefits for at least four months prior to turning age 65, you will typically get Medicare Part A and Part B automatically the first day of the month you turn age 65.
What happens if you refuse Medicare Part B?
If you refuse it, you don’t lose your Medicare Part B eligibility. However, you may have to wait for a valid enrollment period before you can enroll . You may also have to pay a late enrollment penalty for as long as you have Medicare Part B coverage.
How long do you have to work to pay Medicare?
You or your spouse worked long enough (40 quarters or 10 years) while paying Medicare taxes. You or your spouse had Medicare-covered government employment or retiree who has paid Medicare payroll taxes while working but has not paid into Social Security. Normally, you pay a monthly premium for Medicare Part B, no matter how many years you’ve worked.
Is Medicare available to everyone?
Medicare coverage is not available to everyone. To receive benefits under this federal insurance program, you have to meet Medicare eligibility requirements. Find affordable Medicare plans in your area. Find Plans. Find Medicare plans in your area. Find Plans.
Do you pay Medicare Part B monthly?
Normally, you pay a monthly premium for Medicare Part B, no matter how many years you’ve worked. Read more about the Part A and Part B premiums.