By law, you or your legal representative generally have the right to view and/or get copies of your personal health information from these groups: Health care providers who treat you and bill Medicare for your care Health plans that pay for your care, including Medicare These types of personal health information include:
Full Answer
Who is eligible for Medicare and how does it work?
Who is eligible for Medicare? Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
Does social security or Medicare call to get information?
When enrolling in Medicare, you should be aware that neither Social Security nor Medicare calls you to get information. Should any issue arise in which Medicare or Social Security needs any information from you, they’ll ALWAYS send you a letter to notify you.
Do you receive Medicare phone calls?
Medicare beneficiaries are likely to receive phone calls once they become eligible for Medicare. You can get back to enjoying your day in peace after following any of the ways to put an end to spam calls or most of them anyway. You must be looking for a way to get on the Medicare Do Not Call list.
What are my rights as a Medicare patient?
You have the right to be treated fairly, understand the information you get, and keep your personal information safe. Treated with courtesy, dignity and respect at all times. Protected from discrimination. Every company or agency that works with Medicare must obey the law.

Can you disclose information to Medicare or CMS without consent?
Ensure that any disclosure of information is consistent with applicable provisions of 42 CFR Part 480. You cannot disclose information that explicitly identifies institutions, practitioners, or your reviewers without their consent.
Who monitors Medicare?
The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, and the Children's Health Insurance Program (CHIP). For more information, visit hhs.gov.
Does Medicare share my information?
We don't keep separate records or accounting of any social media website users or their interaction with the Medicare.gov pages on social media websites. We don't store or share this information. User information is retained by social media websites in accordance with the website's policies.
What provides information for Medicare beneficiaries?
The EDB has information on all Medicare beneficiaries, including Social Security Retirement and Disability insurance Beneficiaries, End Stage Renal Disease (ESRD) beneficiaries, and Railroad Retirement Board (RRB) beneficiaries.
Who is responsible for the oversight of the facilities?
California state governmentCalifornia state government is responsible for the regulation and oversight of health care facilities through multiple agencies, departments, boards, bureaus, and commissions.
Which is the right of individuals to keep their information from being disclosed to others?
The Privacy Act of 1974 (5 U.S.C. § 552a) protects personal information held by the federal government by preventing unauthorized disclosures of such information. Individuals also have the right to review such information, request corrections, and be informed of any disclosures.
Are Medicare records private?
Apart from you, the only people who can view or access your My Health Record are: Your healthcare providers, for example GPs, specialists, or hospital staff.
Should you give out your Medicare number?
Treat your Medicare card like it's a credit card. Don't ever give it out except to your doctor or other Medicare provider. Never give your Medicare Number in exchange for free medical equipment or any other free offer. Dishonest providers will use your numbers to get payment for services they never delivered.
Why am I getting so many calls about Medicare?
Phone calls Sometimes, they're selling phony products such as supplemental or prescription drug Medicare plans. The whole purpose of all of these calls is to obtain your personal information, whether that is your Medicare card number, your Social Security number, or banking information.
What is a Medicare beneficiary identifier?
The Medicare Beneficiary Identifier (MBI) is the new identification number that has replaced SSN-based health insurance claim numbers (HICNs) on all Medicare transactions, such as billing, claim submissions and appeals.
What are 3 rights everyone on Medicare has?
— Call your plan if you have a Medicare Advantage Plan, other Medicare health plan, or a Medicare Prescription Drug Plan. Have access to doctors, specialists, and hospitals. can understand, and participate in treatment decisions. You have the right to participate fully in all your health care decisions.
Which of the following consumers are eligible for Medicare if other eligibility requirements are met?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
Am I eligible for Medicare Part A?
Generally, you’re eligible for Medicare Part A if you’re 65 years old and have been a legal resident of the U.S. for at least five years. In fact,...
Am I eligible for Medicare Part B?
When you receive notification that you’re eligible for Medicare Part A, you’ll also be notified that you’re eligible for Part B coverage, which is...
How do I become eligible for Medicare Advantage?
If you’re eligible for Medicare benefits, you have to choose how to receive them – either through the government-run Original Medicare program, or...
When can I enroll in Medicare Part D?
To be eligible for Medicare Part D prescription drug coverage, you must have either Medicare Part A or Part B, or both. You can sign up for Medicar...
Who's eligible for Medigap?
If you’re enrolled in both Medicare Part A and Part B, and don’t have Medicare Advantage or Medicaid benefits, then you’re eligible to apply for a...
How long do you have to enroll in Medicare?
However, the law only allows for enrollment in Medicare Part B (Medical Insurance), and premium-Part A (Hospital Insurance), at limited times: 1 Initial Enrollment Period – a 7-month period when someone is first eligible for Medicare. For those eligible due to age, this period begins 3 months before they turn 65, includes the month they turn 65, and ends 3 months after they turn 65. For those eligible due to disability, this period begins three months before their 25th month of disability payments, includes the 25th month, and ends 3 months after. By law, coverage start dates vary depending on which month the person enrolls and can be delayed up to 3 months. 2 General Enrollment Period – January 1 through March 31 each year with coverage starting July 1 3 Special Enrollment Period (SEP) – an opportunity to enroll in Medicare outside the Initial Enrollment Period or General Enrollment Period for people who didn’t enroll in Medicare when first eligible because they or their spouse are still working and have employer-sponsored Group Health Plan coverage based on that employment. Coverage usually starts the month after the person enrolls, but can be delayed up to 3 months in limited circumstances.#N#People who are eligible for Medicare based on disability may be eligible for a Special Enrollment Period based on their or their spouse’s current employment. They may be eligible based on a spouse or family member’s current employment if the employer has 100 or more employees.
How long is the initial enrollment period for Medicare?
Initial Enrollment Period – a 7-month period when someone is first eligible for Medicare. For those eligible due to age, this period begins 3 months before they turn 65, includes the month they turn 65, and ends 3 months after they turn 65. For those eligible due to disability, this period begins three months before their 25th month ...
What is a SEP in Medicare?
Special Enrollment Period (SEP) – an opportunity to enroll in Medicare outside the Initial Enrollment Period or General Enrollment Period for people who didn’t enroll in Medicare when first eligible because they or their spouse are still working and have employer-sponsored Group Health Plan coverage based on that employment.
How long do you have to wait to get Medicare if you have ALS?
People under 65 are eligible if they have received Social Security Disability Insurance (SSDI) or certain Railroad Retirement Board (RRB) disability benefits for at least 24 months. If they have amyotrophic lateral sclerosis (ALS), there’s no waiting period for Medicare.
Does COBRA count as current employment?
But, there are special rules that they need to know. For example, employer coverage for retirees or through COBRA doesn’t count as current employment , so these individuals don’t qualify for a SEP to enroll in Medicare later. A different set of rules apply if the person has Medicare based on disability or ESRD. 5.
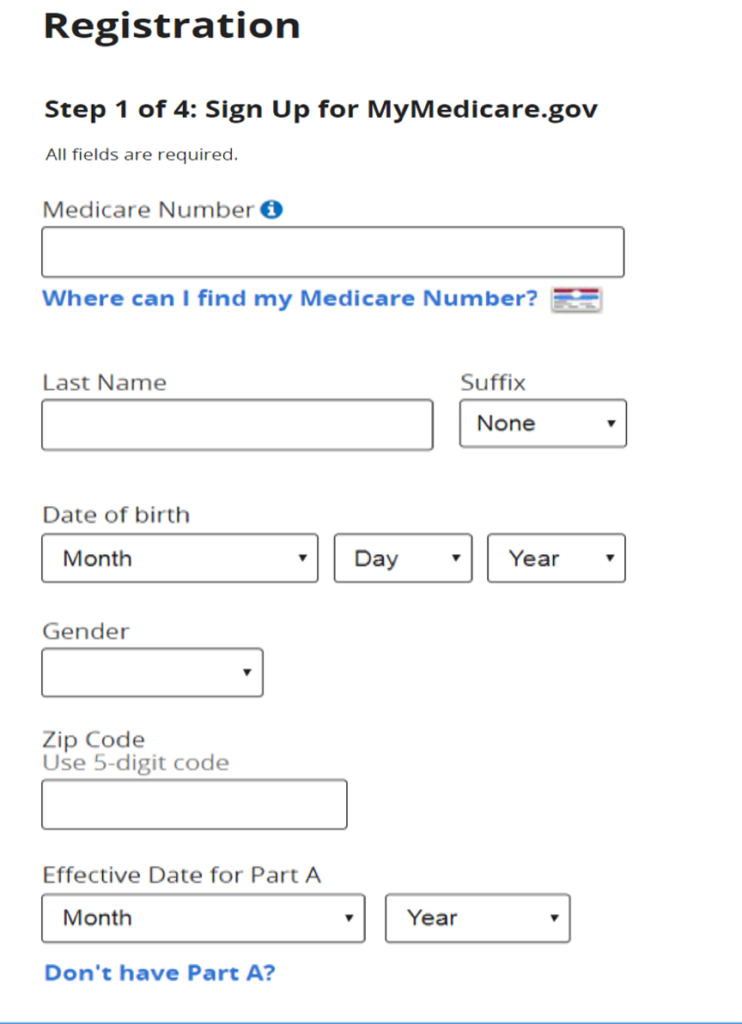
Medicare Eligibility & Enrollment
There are a few different ways you can qualify for Medicare. The most common way that people qualify is through the Medicare eligibility age requirement. If you are 65 or older, then you qualify for Original Medicare. Original Medicare consists of Medicare Part A and Medicare Part B. This includes both hospital insurance and medical insurance.
Medicare Advantage Plan Eligibility
Medicare Advantage plans were formerly known as Medicare Part C. These plans are managed and administered by private insurance companies. These providers can set many of their own rules for each plan, although each plan must have at least the same minimum coverage as that provided by Medicare.
Medicare Part D Eligibility
Medicare Part D provides prescription drug coverage, and like Medicare Advantage plans, these Medicare prescription drug plans are administered by private insurance companies who contract with Medicare. Remember that Original Medicare only provides basic health coverage — both inpatient and outpatient services.
When You Can Start Receiving Medicare Part A & B Benefits
We have already outlined who is eligible for Medicare, so when can you start receiving the benefits? If you qualify based on age, then you can start receiving benefits the month of your 65th birthday. The time that your benefits actually start depends on when you enroll. We will discuss Medicare enrollment periods more in the next section.
Medicare Enrollment Periods
Medicare has a few different enrollment periods, and the time at which you sign up can affect your monthly premium amounts. You can check Medicare.gov for more specific information on Medicare enrollment periods. However, there are a few basic details that you need to know about them. First is the initial enrollment period.
Medicare Eligibility For People Under 65
We have already touched briefly on qualifying for Medicare when you are under 65, but we will discuss the details again here. If you are under 65, you can qualify for Medicare if you receive Social Security disability benefits. You will be automatically enrolled in coverage after you receive benefits for 24 months.
The Bottom Line
Medicare benefits are available to U.S. citizens age 65 and older and younger individuals with disabilities. The program is funded through Medicare taxes and managed by the Social Security Administration. If you meet the eligibility requirements, then applying for coverage is not difficult.
Medicare eligibility: Key takeaways
Generally, you’re eligible for Medicare Part A if you’re 65 and have been a U.S. resident for at least five years.
Am I eligible for Medicare Part A?
Generally, you’re eligible for Medicare Part A if you’re 65 years old and have been a legal resident of the U.S. for at least five years. In fact, the government will automatically enroll you in Medicare Part A at no cost when you reach 65 as long as you’re already collecting Social Security or Railroad Retirement benefits.
Am I eligible for Medicare Part B?
When you receive notification that you’re eligible for Medicare Part A, you’ll also be notified that you’re eligible for Part B coverage, which is optional and has a premium for all enrollees.
How do I become eligible for Medicare Advantage?
If you’re eligible for Medicare benefits, you have to choose how to receive them – either through the government-run Original Medicare program, or through Medicare Advantage.
When can I enroll in Medicare Part D?
To be eligible for Medicare Part D prescription drug coverage, you must have either Medicare Part A or Part B, or both. You can sign up for Medicare Part D at the same time that you enroll in Medicare Part A and B.
Who's eligible for Medigap?
If you’re enrolled in both Medicare Part A and Part B, and don’t have Medicare Advantage or Medicaid benefits, then you’re eligible to apply for a Medigap policy.
What is Medicare for people 65 and older?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
How long do you have to live to qualify for Medicare?
You qualify for full Medicare benefits if: You are a U.S. citizen or a permanent legal resident who has lived in the United States for at least five years and. You are receiving Social Security or railroad retirement benefits or have worked long enough to be eligible for those benefits but are not yet collecting them.
How old do you have to be to get Medicare?
citizen or have been a legal resident for at least five years, you can get full Medicare benefits at age 65 or older. You just have to buy into them by: Paying premiums for Part A, the hospital insurance.
How long do you have to be on disability to receive Social Security?
You have been entitled to Social Security disability benefits for at least 24 months (that need not be consecutive); or. You receive a disability pension from the Railroad Retirement Board and meet certain conditions; or.
What is Medicare card?
The Medicare card is used to identify the individual as being entitled and also serves as a source of information required to process Medicare claims or bills. It displays the beneficiary's name, Medicare number, and effective date of entitlement to hospital insurance and/or medical insurance. The Social Security Administration's Social Security Office assists in replacing a lost or destroyed Medicare cards.
Who is eligible for HI?
Individuals of any age with end stage renal disease (ESRD) who receive dialysis on a regular basis or a kidney transplant are eligible for HI (and are deemed enrolled for Supplementary Medical Insurance (SMI) unless such coverage is refused) if they file an application. They must also meet certain work requirements for insured status under the social security or railroad retirement programs, or be entitled to monthly social security benefits or an annuity under the Railroad Retirement Act, or be the spouse or dependent child of an insured or entitled person.
How long does premium hospital insurance last?
Persons may enroll for premium hospital insurance by filing a request during the IEP which begins the third month before the month of first eligibility and lasts for 7 months. The individual's IEP for premium hospital insurance is in most cases the same 7-month period as the IEP for SMI.
How do I qualify for premium free HI?
To be eligible for premium-free HI, an individual must be "insured" based on his or her own earnings or those of a spouse, parent, or child. To be insured, the worker must have a specific number of quarters of coverage (QCs); the exact number required is dependent upon whether the person is filing for HI on the basis of age, disability, or end stage renal disease. QCs are earned through payment of payroll taxes under the Federal Insurance Contributions Act (FICA) during the person's working years. QCs earned by an individual who pays the full FICA tax are usable to insure the person for both monthly social security benefits and HI.
What is hospital insurance?
Hospital insurance (HI), as well as supplementary medical insurance (SMI), is available to three basic groups of "insured individuals"- the aged, the disabled, and those with end stage renal disease. Following is an explanation of how an individual becomes "insured" as well as an explanation of the eligibility requirements for each group.
How long is the grace period for SMI?
grace period has been provided for payment of premiums by those who are billed directly. The period extends for 90 days after the month in which the bill is mailed. If the premiums are not received in that prescribed time, entitlement terminates at the end of the grace period. This 90-day grace period for paying overdue SMI premiums and continuing SMI coverage may be extended by CMS for good cause for up to an additional 90 days. Good cause, for example, is found if the enrollee was mentally or physically incapable of paying his or her premiums timely, or had some reasonable basis to believe that payment had been made, or the failure to pay was due to administrative error.
What to do if you think Medicare is calling you?
If you think the call is from Medicare, hang up and call them back at the national number. Then, if it was one of them, they can help you. However, if Medicare isn’t attempting to reach you, then you avoid a spammer trying to steal your information. Telemarketing calls attempt to commit fraud and theft.
How to report a fraudulent call to Medicare?
How to Report a Medicare Call. You can report a fraudulent call from someone claiming they worked for Medicare by going to the FTC Complaint Assistant. You can help protect yourself from fraudulent activities by never offering credit card or personal information to anyone.
Is a robocall the same as a doctor's appointment?
Not all robocalls are the same. Often, doctors’ offices will use a robocall to remind you of a doctor’s appointment. Keep this in mind when listening to a robocall. Not all robocalls are harmful, but about 40% of them are spam, and that’s why making reports is essential.
Can you get information from Medicare if you have Social Security?
When enrolling in Medicare, you should be aware that neither Social Security nor Medicare calls you to get information. Should any issue arise in which Medicare or Social Security needs any information from you, they’ll ALWAYS send you a letter to notify you. If you’re getting too many spam phone calls, you might want to get on ...
Will Medicare call you?
Medicare will never call you! Medicare may need information from you or may need to reach you; but, they’ll NEVER call. You’ll get a letter that will notify you of the necessary information that Medicare needs. Long story short, if the calls you’re receiving claim to be from Medicare, it’s a spam call.
Can Medicare call you asking for bank information?
In either of these scenarios or similar situations, do not give out your personal information. Medicare will never call you asking for bank information or credit card numbers.
Can you share your Medicare number with a stranger?
You should never share your Medicare Identifier or Social Security number with a stranger. If you get calls from someone claiming to be Medicare, get a name and phone number, and call Medicare to make a report.