Beneficiaries Who Don't Qualify for Medicare Part A
- Single, Never Married. Take your Notice of Award, Disapproved Claim or both to your local ID card office to update your DEERS record and get a new ID card.
- Widow/Widower. Apply for Medicare Part A under your deceased spouse’s social security number. ...
- Married/Divorced: Spouse Age 62 or Older. ...
- Married/Divorced: Spouse Younger than Age 62. ...
Full Answer
Which providers cannot enroll in Medicare?
Since Medicare is open to people aged 65 or older, if you are under 65 and do not meet other qualifying requirements, you cannot enroll in the program until you become eligible. People diagnosed with end-stage renal disease or amyotrophic lateral sclerosis can enroll in Medicare even while under 65.
Which group of people is not served by Medicare?
Who is not automatically eligible for Medicare? People who must pay a premium for Part A do not automatically get Medicare when they turn 65. They must: File an application to enroll by contacting the Social Security Administration; Enroll during a valid enrollment period; and. What are the 3 requirements for a member to be eligible for a Medicare?
Can you be penalized for not enrolling in Medicare?
If you do not qualify on your own or through your spouse’s work record but are a U.S. citizen or have been a legal resident for at least five years, you can get full Medicare benefits at age 65 or older. You just have to buy into them by: Paying premiums for Part A, the hospital insurance.
What is the penalty for not signing up for Medicare?
May 28, 2019 · As long as you meet the citizenship/legal residence requirements described above, you may be eligible for Medicare when you are younger than age 65 if one of the following circumstances applies to you: You have been receiving Social Security disability benefits for at least 24 months in a row.
See more
Feb 10, 2022 · Q: Who is not eligible for Medicare? A: Those who do not meet the listed requirements above, such as correct age and or having been eligible for Social Security or Railroad Retirement Board benefits. Q: How can I speak to someone about my eligibility? A: For questions about Medicare, you can create an online Medicare account HERE or call 1-800 …
Who is not qualified for Medicare?
receive Social Security disability benefits for at least 2 years. receive disability pension benefits from the Railroad Retirement Board. have amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig's disease. have end stage renal disease (ESRD), or kidney failure.
Can you be denied from Medicare?
Medicare can deny coverage if a person has exhausted their benefits or if they do not cover the item or service. When Medicare denies coverage, they will send a denial letter. A person can appeal the decision, and the denial letter usually includes details on how to file an appeal.Aug 20, 2020
Does everyone have to get Medicare?
Strictly speaking, Medicare is not mandatory. But very few people will have no Medicare coverage at all – ever. You may have good reasons to want to delay signing up, though.
How do I know if I qualify for Medicare?
You are eligible for Medicare if you are a citizen of the United States or have been a legal resident for at least 5 years and: You are age 65 or older and you or your spouse has worked for at least 10 years (or 40 quarters) in Medicare-covered employment.
Can you get Medicare if you never paid into Social Security?
Even if you don't qualify for Social Security, you can sign up for Medicare at 65 as long you are a U.S. citizen or lawful permanent resident.
Why do people get denied for Medicare?
Medicare may issue denial letters for various reasons. Example of these reasons include: You received services that your plan doesn't consider medically necessary. You have a Medicare Advantage (Part C) plan, and you went outside the provider network to receive care.May 18, 2020
What parts of Medicare are mandatory?
There are four parts to Medicare: A, B, C, and D. Part A is automatic and includes payments for treatment in a medical facility. Part B is automatic if you do not have other healthcare coverage, such as through an employer or spouse.
Is my spouse eligible for Medicare if she never worked?
Medicare can be available to anyone – including a non-working spouse – who is at least 65 years old and a U.S. citizen or legal resident of at least five years. You may even qualify for Medicare before 65 if you have a qualifying disability or health condition.Jan 20, 2022
Is Part D mandatory?
Is Medicare Part D Mandatory? It is not mandatory to enroll into a Medicare Part D Prescription Drug Plan.
What is considered income for Medicare?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
Do I automatically get Medicare when I turn 65?
Medicare will automatically start when you turn 65 if you've received Social Security Benefits or Railroad Retirement Benefits for at least 4 months prior to your 65th birthday. You'll automatically be enrolled in both Medicare Part A and Part B at 65 if you get benefit checks.
Who is eligible for Medicare Part B?
Eligibility for Medicare Part B You are 65 or older. You have been on Social Security Disability Insurance (SSDI) for two years. You have end-stage renal disease (ESRD).
How old do you have to be to get Medicare?
citizen or have been a legal resident for at least five years, you can get full Medicare benefits at age 65 or older. You just have to buy into them by: Paying premiums for Part A, the hospital insurance.
How long do you have to live to qualify for Medicare?
You qualify for full Medicare benefits if: You are a U.S. citizen or a permanent legal resident who has lived in the United States for at least five years and. You are receiving Social Security or railroad retirement benefits or have worked long enough to be eligible for those benefits but are not yet collecting them.
How much will Medicare premiums be in 2021?
If you have 30 to 39 credits, you pay less — $259 a month in 2021. If you continue working until you gain 40 credits, you will no longer pay these premiums. Paying the same monthly premiums for Part B, which covers doctor visits and other outpatient services, as other enrollees pay.
How many credits do you get in 2021?
Work credits are earned based on your income; the amount of income it takes to earn a credit changes each year. In 2021 you earn one work credit for every $1,470 in earnings, up to a maximum of four credits per year. If you have accrued fewer than 30 work credits, you pay the maximum premium — $471 in 2021.
How long do you have to be on disability to receive Social Security?
You have been entitled to Social Security disability benefits for at least 24 months (that need not be consecutive); or. You receive a disability pension from the Railroad Retirement Board and meet certain conditions; or.
What is Lou Gehrig's disease?
You have Lou Gehrig’s disease, also known as amyotrophic lateral sclerosis (ALS), which qualifies you immediately; or. You have permanent kidney failure requiring regular dialysis or a kidney transplant — and you or your spouse has paid Social Security taxes for a specified period, depending on your age.
How old do you have to be to get Medicare?
If you are age 65 or older, you are generally eligible to receive Medicare Part A (hospital insurance) and Medicare Part B (medical insurance) if you are a United States citizen or a permanent legal resident who has lived in the U.S. for at least five years in a row.
What happens if you refuse Medicare Part B?
If you refuse it, you don’t lose your Medicare Part B eligibility. However, you may have to wait for a valid enrollment period before you can enroll . You may also have to pay a late enrollment penalty for as long as you have Medicare Part B coverage.
How long do you have to work to pay Medicare?
You or your spouse worked long enough (40 quarters or 10 years) while paying Medicare taxes. You or your spouse had Medicare-covered government employment or retiree who has paid Medicare payroll taxes while working but has not paid into Social Security. Normally, you pay a monthly premium for Medicare Part B, no matter how many years you’ve worked.
When do you get Medicare Part A and Part B?
If you meet Medicare eligibility requirements and you have received Social Security benefits for at least four months prior to turning age 65, you will typically get Medicare Part A and Part B automatically the first day of the month you turn age 65.
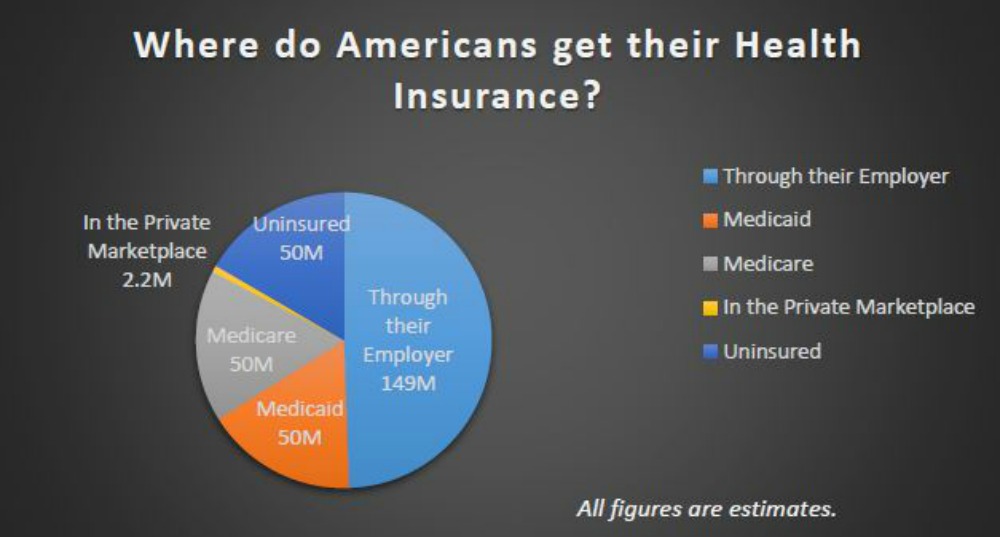
Is Medicare available to everyone?
Medicare coverage is not available to everyone. To receive benefits under this federal insurance program, you have to meet Medicare eligibility requirements. Find affordable Medicare plans in your area. Find Plans. Find Medicare plans in your area. Find Plans.
What age do you have to be to get Medicare?
You must also meet at least one of the following criteria for Medicare eligibility: Be age 65 or older and eligible for Social Security: You may be automatically enrolled in Medicare Part A (hospital insurance) when you reach age 65 and become eligible for Social Security. But, if you’re not receiving retirement benefits from Social Security or ...
What happens if you don't sign up for Medicare Part B?
Be aware that if you don’t sign up for Medicare Part B when you first become eligible, you may have to pay a 10% penalty (added to your monthly premium) for each full 12-month period you could have had it but didn’t sign up (some exceptions apply).
What is Medicare Part C?
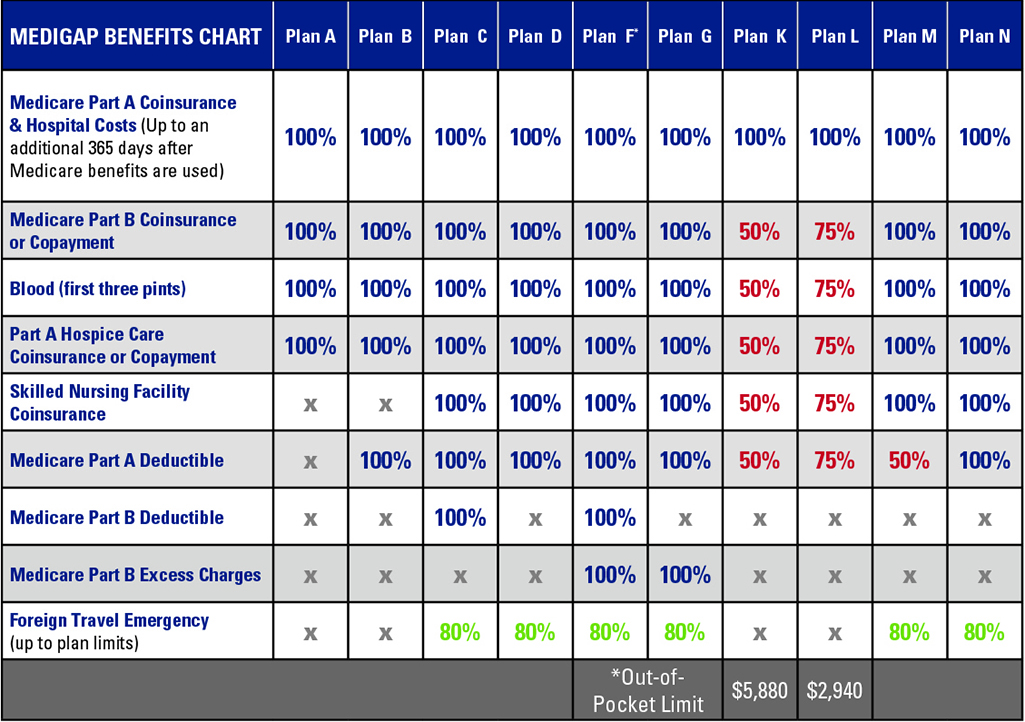
Medicare Part C (also called Medicare Advantage ) is an alternative way to get your Medicare Part A and Part B benefits. Medicare Advantage plans are available through private insurers. To be eligible for Medicare Part C, you must already be enrolled in Medicare Part A and Part B, and you must reside within the service area ...
How long does Medicare Advantage last?
The Medicare Advantage plan (Part C) Initial Coverage Election Period is generally the same as the Initial Enrollment Period for Medicare Part A and Part B (the seven-month period that starts 3 months before the month you turn 65, includes the month you turn 65, and ends 3 months after the month you turn 65).
How much is the Part B premium for 2021?
In addition, you must also pay the Part B premium each month. The standard premium is $148.50 in 2021. Also, keep in mind that individuals with a higher income may have to pay more for their Part B premium.
How long do you have to be disabled to get a disability?
Be permanently disabled and receive disability benefits for at least two years: You automatically get Part A and Part B after you get disability benefits from Social Security for 24 months or certain disability benefits from the Railroad Retirement Board (RRB) for 24 months. Have end-stage renal disease (ESRD) (permanent kidney failure ...
Is there a penalty for not signing up for Medicare Part C?
Medicare Part C is optional, and there is no penalty for not signing up. But you must have Medicare Part A and Part B to get Part C, and live in the service area of a Medicare Advantage plan. If you have Medicare Part C, you must continue paying your Part B premium even if you enroll in a Medicare Advantage plan.
What happens if you don't sign up for Medicare Part B?
Remember, if you don't sign up for Part B when you're first eligible, you may have to pay a Medicare Part B Late Enrollment PenaltyYour monthly premium for Part B may go up 10% for each full 12-month period that you could have had Part B, but didn't sign up for it. if you sign up later.
What happens if you don't get a Part A?
If you're not eligible for free Part A: You'll get a Notice of Award, Disapproved Claim or both from the Social Security Administration, based on your deceased sponsor's social security number . Take the Notice of Award, Disapproved Claim or both to your local ID card office to update your DEERS record and get a new ID card.
When do you have to be on Medicare before you can get Medicare?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
What is the income related monthly adjustment amount for Medicare?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
What happens if you don't enroll in Part A?
If an individual did not enroll in premium Part A when first eligible, they may have to pay a higher monthly premium if they decide to enroll later. The monthly premium for Part A may increase up to 10%. The individual will have to pay the higher premium for twice the number of years the individual could have had Part A, but did not sign up.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
Why does Part A end?
There are special rules for when premium-free Part A ends for people with ESRD. Premium Part A and Part B coverage can be voluntarily terminated because premium payments are required. Premium Part A and Part B coverage ends due to: Voluntary disenrollment request (coverage ends prospectively); Failure to pay premiums;