You pay your Medicare Supplement
Medigap
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
Full Answer
How does Medicare supplement insurance work with Medicare?
Medicare Supplement Insurance (Medigap) policies, sold by private companies, can help pay for some of the costs that Original Medicare doesn’t cover, like copayments, coinsurance, and deductibles. Some Medigap policies also offer coverage for services that Original Medicare doesn’t cover, like emergency medical
Who regulates Medicare supplement insurance plans?
Mar 24, 2022 · Medicare Supplement Insurance, also known as Medigap insurance, was created to fill in the “gaps” in costs left behind by Medicare Part A and Part B. Medicare Part A and Part B sometimes require you to pay deductibles, copays, and coinsurances. A Medicare Supplement policy can help you cover these costs.
How do I Pay my Medicare supplement insurance (Medigap) premium?
Summary: If you have a Medicare Supplement insurance plan, you pay your premium separately from your monthly Medicare premiums, like Medicare Part B. You pay your Medicare Supplement Insurance (Medigap) premium as directed by the insurance company that sold you the plan. Medicare Supplement insurance plans are sold by private insurance companies and may help …
What are the different Medicare supplement plans?
Sep 06, 2012 · Here's how the supplements work: Medigap, also called a Medicare Supplement, basically pays the portion of medical expenses that Medicare expects you to pay. Medicare is an "80/20" plan, meaning...

Do most people on Medicare have supplemental insurance?
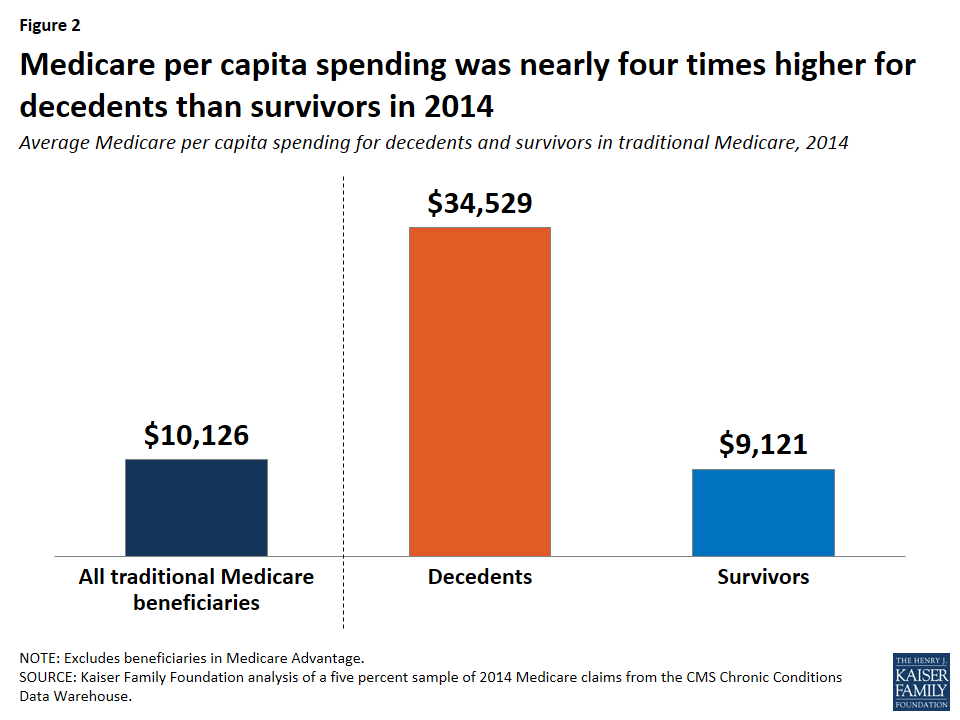
Among Medicare beneficiaries in traditional Medicare, most (83%) have supplemental coverage, either through Medigap (34%), employer-sponsored retiree health coverage (29%), or Medicaid (20%).Mar 23, 2021
Who pays for Medigap?
You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
Is Medicare supplemental insurance based on income?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
What is a supplemental insurance for patients with Medicare as their primary insurance?
A Medigap policy is health insurance sold by private insurance companies to fill the “gaps” in Original Medicare Plan coverage. Medigap policies help pay some of the health care costs that the Original Medicare Plan doesn't cover.Dec 1, 2021
What does Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
What is not covered by Medigap?
Medigap is extra health insurance that you buy from a private company to pay health care costs not covered by Original Medicare, such as co-payments, deductibles, and health care if you travel outside the U.S. Medigap policies don't cover long-term care, dental care, vision care, hearing aids, eyeglasses, and private- ...Nov 18, 2020
How much does Medicare take out of Social Security?
What are the Medicare Part B premiums for each income group? In 2021, based on the average social security benefit of $1,514, a beneficiary paid around 9.8 percent of their income for the Part B premium. Next year, that figure will increase to 10.6 percent.Nov 22, 2021
Is Social Security considered income for Medicare?
For purposes of the Medicare Prescription Drug Discount Card, we have defined “income” as money received through retirement benefits from Social Security, Railroad, the Federal or State Government, or other sources, and benefits received for a disability or as a veteran, plus any other sources of income that would be ...
What is the average cost of a Medicare supplement plan?
The average cost of a Medicare supplemental insurance plan, or Medigap, is about $150 a month, according to industry experts. These supplemental insurance plans help fill gaps in Original Medicare (Part A and Part B) coverage.
What is the difference between Medicare Advantage and Medicare Supplement?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.Oct 1, 2021
What is true about Medicare supplement insurance plans?
Medicare supplement plans don't work like most health insurance plans. They don't actually cover any health benefits. Instead, these plans cover the costs you're responsible for with Original Medicare.Aug 26, 2018
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
Who regulates Medicare Supplement Insurance?
Medicare Supplement Insurance plans are tightly regulated by the Centers for Medicare and Medicaid Services (CMS), a government agency. CMS determines what each letter plan will cover, and it requires each insurance company to offer the plan as is, without modifications.
How much does Medicare pay for a doctor's visit?
Here’s an example with numbers: if the doctor’s visit had a Medicare-approved cost of $100, Medicare would pay $80, your Medigap would pay $15, and you would only have to pay $5.
What is a Medigap plan?
Also called Medigap because it covers “gaps” in costs after Medicare Parts A and B pay their share. Medigap Plans C and F, which cover the Medicare Part B deductible, are being discontinued in 2020. Sign up for Medigap during Open Enrollment to lock in the best premium for your plan. Our Approach.
What is covered by Plan A?
Plan A also covers 100% of coinsurances or copayments for hospice care services, 100% of Medicare Part B coinsurances or copayments for medical outpatient services, and 100% of the cost of the first three pints of blood you are administered during a procedure.
How much is Medicare Part B deductible?
For 2019, the deductible for Medicare Part B is $185. After the deductible, you’ll pay 20% of most medical expenses.
What happens if you don't enroll in Medicare?
If you don’t enroll in Part A (inpatient hospital services) when you initially qualify, you may find yourself saddled with a 10% late enrollment penalty on your Part A premium. Says the Medicare website, “You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.”
What does Medicare Part B cover?
Both plans also cover Medicare Part B coinsurances and copays, the first three pints of blood, Part A hospice care coinsurances or copays, skilled nursing facility care coinsurances, and the Part A deductible, but not at 100% like other plans. Plan K covers these benefits at 50% and Plan L covers them at 75%.
What factors affect Medicare Supplement insurance?
Several factors can influence your Medicare Supplement insurance plan costs. The first factor is what your plan covers. In general, the more benefits a Medicare Supplement plan has, the more it’s likely to cost. All Medicare Supplement insurance policies available in most states are standardized with lettered names (A, B, C*, D, F*, G, K, L, M, ...
Why does Medicare premium go up?
This is called attained-age-rated. With all three ways, premiums may go up because of inflation and other factors. A third factor influencing your Medicare Supplement insurance plan cost is whether or not you were subjected to medical underwriting.
What is community rated Medicare?
The first way doesn’t take age into account when setting the price of the plan. This is called community rated or “no-age-rated.”. The second way bases the premium on the age you are when you buy the Medicare Supplement insurance plan. This is called issue-age rated or “entry age-rated.”.
Do you pay Medicare Supplement Insurance premiums separately?
Summary: If you have a Medicare Supplement insurance plan, you pay your premium separately from your monthly Medicare premiums, like Medicare Part B. You pay your Medicare Supplement Insurance (Medigap) premium as directed by the insurance company that sold you the plan. Medicare Supplement insurance plans are sold by private insurance companies ...
Medicare supplement plan explained
First things first, before we dig deeper into the costs associated with the Medicare Supplement plan, let’s make sure we’re on the same page with what this plan is.
Why should you get Medicare supplement insurance?
Medicare supplement insurance plans bring plenty of benefits to people aged 65 or those with disabilities. And, it all comes down to efficiently tackling increasing healthcare costs. So, if you’re wondering whether or not Medicare Supplement Plans are worth it, find out that the answer is, “Absolutely!”
How much does Medigap policy cost on average?
Now, let’s get to the main question that probably everybody interested in getting Medigap has on their minds, “what is the average cost of supplemental insurance from MedicareWire ?”. The average Medicare Supplement policy premium cost $154.50 per month in 2022.
What is Medicare Supplement?
Medicare supplement insurance helps fill in the ‘gaps’ that original Medicare misses. Supplemental Medicare plans are sold by private insurance companies.Such plans can assist with copays, coinsurance, and deductibles. Some plans also help cover medical care when you’re abroad.
What does a supplemental health plan cover?
They may also cover medical services that your usual health service plan doesn’t cover at all, including dental and vision fees. Other supplemental plans may provide a cash benefit paid out over a certain time frame or provide it in one lump sum. This cash may be used for: Covering lost wages.
What is a Medigap plan?
Medigap plans are a supplemental insurance option for those already enrolled in original Medicare who are seeking extra financial coverage. When you participate in a Medigap plan, you’ll receive coverage for specific costs like deductibles, coinsurance, and copayments.
What insurance plans are not medigap?
Insurance Plans That Aren’t Medigap. It’s easy to confuse some insurance plans for Medigap. Some insurance plans that are not Medigap include: Medcaid. Medicare Advantage Plans (like an HMO, PPO, or Private Fee-for-Service Plan) Medicare Prescription Drug Plans. Employer or union plans, such as the Federal Employees .
What is supplemental insurance?
Supplemental insurance refers to additional or extra insurance that helps to cover the services and out-of-pocket expenses that an individual’s primary Medicare insurance doesn’t cover. Some supplemental insurance plans will cover the out-of-pocket cost-sharing that comes with your health insurance plan, such as deductibles, coinsurance, ...
How many Medigap plans are there?
There are 10 Medigap plans available for purchase: A, B, C, D, F, G, K, L, M, and N. Some Medigap plans cannot be purchased by new Medicare members. These include policies C, F, E, H, I, and J. But, if you already have one of these policies, you can keep it.
What are some examples of supplemental health insurance?
Food, medication, and other unexpected costs you have due to an illness or injury. Examples of supplemental health insurance include: Dental insurance. Critical illness insurance. Vision insurance plans. Disability insurance. Travel insurance for health care coverage when you are outside your health insurance system. Long-term care insurance.
Can you spend down your medical expenses on medicaid?
On the other hand, in medically needy states, Medicaid applicants are able to “spend down” their “excess” income on medical expenses. Once one has spent their income down to the Medicaid income limit, he / she is eligible for Medicaid for the rest of the spend down period.
Is Medicare the primary or secondary payer?
When one has original Medicare and MediGap, original Medicare is the primary payer, meaning that original Medicare pays the portion of the bills for which it owes first. The remaining portion of the bill is then sent to MediGap, who is the secondary payer.
Do you need a medicaid supplement policy?
Essentially, Medicaid takes the place of a MediGap policy. Therefore, there is no need for Medicaid beneficiaries to have a Medicare supplement insurance policy. However, in the rare case that a Medicaid beneficiary does have a MediGap policy, original Medicare is the primary payer, MediGap, the secondary payer, and Medicaid, the final payer.
Is Medicare Supplement Insurance necessary?
However, for persons who qualify for Medicaid, Medicare supplement insurance is not necessary. This is because original Medicare will continue to be the primary payer, while Medicaid will be the secondary payer. Essentially, Medicaid takes the place of a MediGap policy. Therefore, there is no need for Medicaid beneficiaries to have ...
Can you have Medigap if you have medicaid?
It is not advised that persons eligible for Medicaid maintain a MediGap health insurance policy. This is because Medicare supplement insurance helps to cover the costs that original Medicare does not, such as deductibles, coinsurance, and copayments.
Can you deposit excess income into a medicaid trust?
In income cap states (approximately half of the states), Medicaid applicants can deposit their “excess” income (the income over Medicaid’s income limit) into a Qualified Income Trust (also called a Miller Trust) in order to meet Medicaid’s income limit.
Is it illegal to sell medicaid?
That said, it is actually illegal (in most cases) for insurance companies to sell Medicaid beneficiaries a Medicare supplement insurance policy. For persons who have income over Medicaid’s income limit, there are other ways for one to meet Medicaid’s income limit.
How does Medicare reimbursement work?
A Medicare premium reimbursement is a fantastic way for active employees to get refunds of their premiums. Often, premiums may cost less than group insurance at your workplace. If you prefer Medicare to your group coverage, you may be eligible to get premium reimbursements.
Who is responsible for paying your insurance premiums?
As a beneficiary, YOU are responsible for paying your premiums. Employers can reimburse any Part B and Part D premiums for employees who are actively working. This requires the company’s payment plan to integrate with the group insurance plan.
What is ICHRA insurance?
Individual Coverage Health Reimbursement Arrangement (ICHRA) To be eligible for an Individual Coverage Health Reimbursement Arrangement, you’ll need Part A and Part B, or Part C. You can use the ICHRA to reimburse premiums for Medicare and Medigap as well as other costs. Employers have more choice in which medical costs are eligible ...
What is a health reimbursement arrangement?
A Health Reimbursement Arrangement is a system covered by Section 105. This arrangement allows your employer to reimburse you for your premiums. Some HRAs at employers that provide group coverage require that your employer’s payment plan ties in with the group health plan. Contact a human resources representative at your organization ...
What does MEC mean for Medicare?
This type of arrangement can help reimburse employees for their Medicare premiums. If an employee holds minimum essential coverage (MEC), they can get assistance in paying for virtually all Medicare costs, including Medigap premiums.
Can my employer pay my Medicare premiums in 2021?
Updated on July 13, 2021. While your employer can’t pay your Medicare premiums in the true sense, you’ll be glad to know that they may reimburse you for your premium costs! To compensate you, your employer will need to create a Section 105 Medical Reimbursement Plan. We’re here to help you understand your options for reimbursement ...
Is a Section 105 reimbursement taxable?
Some Section 105 plans may only permit refunds on healthcare costs and premiums. This compensation isn’t taxable. If the Section 105 plan reimburses with cash for any remaining benefits, both the money and reimbursements are taxable.answer.