Some of the general requirements you must meet to qualify for Medicaid include: 6 3
- Immigration or citizenship status: You must be either a U.S. ...
- Residency: You must be a resident of the state for whose Medicaid program you’re applying.
- Age: You must meet the program’s age requirements.
- Social Security number: The law mandates a Social Security number or proof of application from anyone applying for Medicaid.
Who really pays for Medicaid?
Who Really Pays For Health Care Might Surprise You
- Before Obamacare we had a free-market health-care system. Government has been part of the business of medicine at least since the 1940s, when Washington began appropriating billions to build private ...
- I fully paid for Medicare through taxes deducted from my salary. ...
- Premiums from my paycheck fund my company health plan. Probably not entirely. ...
What's the income level requirement to qualify for Medicaid?
What’s the Income Level Requirement to Qualify for Medicaid?
| Family Size | 100% | 120% | 140% | 150% |
| 1 | $11,770 | $14,124 | $16,478 | $17,655 |
| 2 | $15,930 | $19,116 | $22,302 | $23,895 |
| 3 | $20,090 | $24,108 | $28,126 | $30,135 |
| 4 | $24,250 | $29,100 | $33,950 | $36,375 |
What is the earnings limit for Medicaid?
Regular Medicaid Income Limit. Single, Divorced: $995 or $885, depending on address; Married, both spouses: $1234 or $1125, depending on address; Married, one spouse: $1234 or $1125, depending on address; Nursing Home Care Income Limit. Single, Divorced: less than nursing home expenses; Married, both spouses: less than nursing home expenses
What assets are allowed on Medicaid?
These include the following:
- Personal possessions, such as clothing, furniture, and jewelry
- One motor vehicle, regardless of value, as long as it is used for transportation of the applicant or a household member. ...
- The applicant's principal residence, provided it is in the same state in which the individual is applying for coverage. ...

What is the criteria for Medicare?
Be age 65 or older; Be a U.S. resident; AND. Be either a U.S. citizen, OR. Be an alien who has been lawfully admitted for permanent residence and has been residing in the United States for 5 continuous years prior to the month of filing an application for Medicare.
Do you automatically get Medicare with Social Security?
You automatically get Medicare because you're getting benefits from Social Security (or the Railroad Retirement Board). Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
How much does Social Security take out for Medicare each month?
In 2021, based on the average social security benefit of $1,514, a beneficiary paid around 9.8 percent of their income for the Part B premium. Next year, that figure will increase to 10.6 percent.
Do you automatically get a Medicare card when you turn 65?
You should receive your Medicare card in the mail three months before your 65th birthday. If you are NOT receiving benefits from Social Security or the RRB at least four months before you turn 65, you will need to sign up with Social Security to get Parts A and B.
How old do you have to be to get Medicare?
If you are age 65 or older, you are generally eligible to receive Medicare Part A (hospital insurance) and Medicare Part B (medical insurance) if you are a United States citizen or a permanent legal resident who has lived in the U.S. for at least five years in a row.
How long do you have to work to pay Medicare?
You or your spouse worked long enough (40 quarters or 10 years) while paying Medicare taxes. You or your spouse had Medicare-covered government employment or retiree who has paid Medicare payroll taxes while working but has not paid into Social Security. Normally, you pay a monthly premium for Medicare Part B, no matter how many years you’ve worked.
What happens if you refuse Medicare Part B?
If you refuse it, you don’t lose your Medicare Part B eligibility. However, you may have to wait for a valid enrollment period before you can enroll . You may also have to pay a late enrollment penalty for as long as you have Medicare Part B coverage.
When do you get Medicare Part A and Part B?
If you meet Medicare eligibility requirements and you have received Social Security benefits for at least four months prior to turning age 65, you will typically get Medicare Part A and Part B automatically the first day of the month you turn age 65.
Is Medicare available to everyone?
Medicare coverage is not available to everyone. To receive benefits under this federal insurance program, you have to meet Medicare eligibility requirements. Find affordable Medicare plans in your area. Find Plans. Find Medicare plans in your area. Find Plans.
Medicare Eligibility: Age 65
As of 2021, approximately 54 million that meet the Medicare requirements, are age 65 and older. In fact, a little over 10,000 people are turning 65 each day until 2030.
Medicare Eligibility: Under Age 65
In 2021, Kaiser reported that approximately 9 million of the 63 million Medicare beneficiaries were under 65 and met the Medicare qualifications to get Part A and Part B benefits.
Medicare Eligibility: Medicare Part A (Hospital Benefits)
Your Medicare Part A benefits will start on the 1 st day of the month and after you meet the Medicare requirements (Turning 65, Under 65 collecting Social Security Disability Benefits for 24 months or are diagnosed with End Stage Renal Disease or Lou Gehrig’s Disease).
Medicare Eligibility: Medicare Part B (Physician Services)
The Medicare requirements to be eligible for Medicare Part B are the same as the Part A requirements. And, like Part A, your Part B benefits always start on the 1 st of the month.
Medicare Eligibility: Medicare Part C (Medicare Advantage)
There is no Medicare age requirement to be eligible to enroll in a Medicare Advantage plan. However, to be Medicare eligible to enroll in a Medicare Advantage plan you must be eligible for and/or enrolled in Original Medicare Part A and Part B.
Medicare Eligibility: Medicare Part D (Medicare Drug Coverage)
To be eligible for Medicare Part D you only need to be eligible for and/or enrolled in Medicare Part A. You do not need to be eligible or enrolled in Medicare Part B to obtain your Medicare Part D drug coverage.
Eligibility for Medicare Supplement (Medigap Plan Eligibility)
To meet the Medicare requirements to enroll in a Medicare Supplement Plan, you must have and or be enrolled in both Medicare Part A and Medicare Part B.
What is the Medicare Part B deductible for 2021?
In 2021, the Medicare Part B deductible is $203. After you reach this deductible, you pay 20% of the Medicare-approved amount for most care.
How much is Medicare Part B deductible?
The most common monthly Part B premium is $148.50. If you have a high income, you'll pay more. In 2021, the Medicare Part B deductible is $203.
Is Medicare free?
By and large, Medicare is not considered free. Because you have been contributing to your Medicare services through taxes throughout your life, you will have contributed money to Medicare regardless of the current cost of your copayments or premiums. However, it's possible to receive assistance for your Medicare Part A and Part B premiums, copays, ...
How old do you have to be to get Medicare?
Generally, you can get Medicare if one of these conditions applies: You are at least 65 years old. You are disabled and receive Social Security Disability Insurance (SSDI) or Railroad Retirement disability payments. You have End-Stage Renal Disease, or ESRD.
How much is Medicare Advantage?
There is no premium for Part A, but there is for Part B. In 2019, that was set at a standard of $135.50 or higher, depending on income level. In addition to any premiums that are ...
What is inpatient care?
Inpatient care if you are hospitalized. Skilled nursing care in a nursing facility. Nursing home care (not custodial or long-term) Hospice care. Home health care, which may include part-time nursing care, physical therapy, or more. This coverage is mandated by federal and state laws as well as by coverage decisions made by Medicare ...
What are the benefits of Medicare Part B?
Medicare Part B builds on the benefits of Part A by providing the following coverages: 1 Doctor visits 2 Lab tests 3 Ambulance services 4 Durable medical equipment, like blood sugar monitors, crutches, or wheelchairs 5 Mental health care, including inpatient and outpatient services and partial hospitalization 6 Some limited outpatient prescription drugs, including those you would get in a hospital or outpatient setting as opposed to those you’d give yourself. This includes flu shots and other vaccinations, as well as transplant drugs, and those for end-stage renal disease.
Is there a single way to sign up for Medicare Advantage?
Every Medicare Advantage plan has its own requirements and processes, and thus there’s no single way to sign up. Your first task is to find out what coverage plans are accessible in your area and compare the benefits of the plans with the benefits you’d have in Original Medicare.
Does Medicare cover kidney transplants?
Many Medicare Advantage plans will not cover you if you have permanent kidney failure that requires regular dialysis, or if you’ve had a kidney transplant. You’ll need to talk to a membership coordinator at the company you’re interested in working with to see if they will cover you, if you are in this situation.
Does Medicare Advantage cover hospice?
The only part of the Original Medicare coverage that is not necessarily covered by Medicare Advantage is hospice care, but don’t worry: even if you’re with Medicare Advantage, you can still access the Original Medicare hospice coverage.
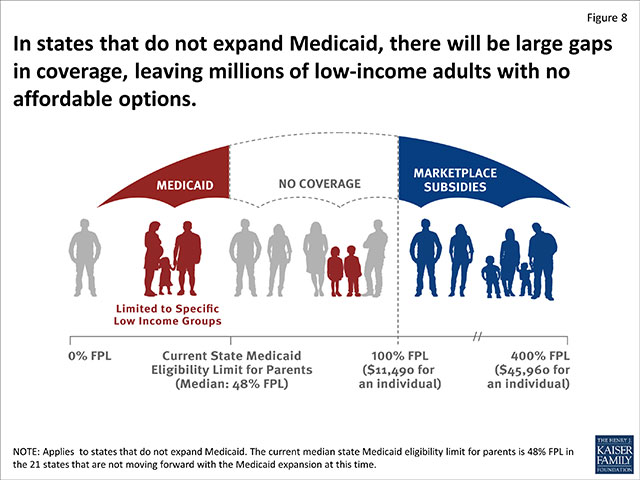
What if I don't qualify for medicaid?
If you don't qualify for Medicaid, we'll tell you if you qualify for financial help to buy a Marketplace health plan instead. (But unless you qualify to enroll with a Special Enrollment Period, you'll have to wait until the next Open Enrollment Period.)
Can I buy a private health plan through the Marketplace?
You may be able to buy a private health plan through the Marketplace instead for the 2018 plan year in the fall. You may qualify for savings based on your income through a premium tax credit and savings on out-of-pocket costs. If you don't qualify for either Marketplace or Medicaid savings, you still have options. Learn more here.
Can I qualify for medicaid based on my income?
No matter your state, you may qualify for Medicaid based on your income, household size, disability, family status, and other factors. But if your state has expanded Medicaid coverage, you can qualify based on your income alone. Enter your household size and state.
What is dual eligible for Medicare?
Eligibility for the Medicare Savings Programs, through which Medicaid pays Medicare premiums, deductibles, and/or coinsurance costs for beneficiaries eligible for both programs (often referred to as dual eligibles) is determined using SSI methodologies..
How many people are covered by medicaid?
Medicaid is a joint federal and state program that, together with the Children’s Health Insurance Program (CHIP), provides health coverage to over 72.5 million Americans, including children, pregnant women, parents, seniors, and individuals with disabilities. Medicaid is the single largest source of health coverage in the United States.
What is Medicaid Spousal Impoverishment?
Spousal Impoverishment : Protects the spouse of a Medicaid applicant or beneficiary who needs coverage for long-term services and supports (LTSS), in either an institution or a home or other community-based setting, from becoming impoverished in order for the spouse in need of LTSS to attain Medicaid coverage for such services.
What is MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents, and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid. MAGI replaced the former process for calculating Medicaid eligibility, ...
What is Medicaid coverage?
Medicaid is the single largest source of health coverage in the United States. To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, ...
How long does medicaid last?
Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
Does Medicaid require income?
Certain Medicaid eligibility groups do not require a determination of income by the Medicaid agency. This coverage may be based on enrollment in another program, such as SSI or the breast and cervical cancer treatment and prevention program.
