As part of the effort to resolve the severe shortfall in the California budget, the Legislature and Governor adopted state law that ends Medi-Cal payments of the Medicare Part B premiums for some Medi-Cal beneficiaries as of November 1.
Full Answer
What happens if you don’t pay Medicare premiums?
For example, if you get an initial bill on February 27, it will be due by March 25. If you don’t pay by that date, you’ll get a second bill from Medicare asking for that premium payment.
Are Medicare premiums taken out of Social Security benefits?
Medicare Part B premiums are normally taken out of your Social Security benefits. You can also set up your Part C and Part D premiums to be deducted from your benefits. You can pay Medicare online or by mail if your premiums aren’t automatically deducted.
Why did California end Medi-Cal premiums for Medicare Part B?
As part of the effort to resolve the severe shortfall in the California budget, the Legislature and Governor adopted state law that ends Medi-Cal payments of the Medicare Part B premiums for some Medi-Cal beneficiaries as of November 1.
Why don't I get a bill from Medicare?
Most people don't get a bill from Medicare because they get these premiums deducted automatically from their Social Security (or Railroad Retirement Board) benefit.) Your bill pays for next month's coverage (and future months if you get the bill every 3 months).
How do you qualify to get $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
Who does not pay Medicare premiums?
Who doesn't have to pay a premium for Medicare Part A? A: Most Medicare-eligible people do not have to pay premiums for Medicare Part A. If you are 65 and you or your spouse has paid Medicare taxes for at least 10 years, you don't pay a premium for Part A.
Why would you lose Medicare benefits?
Depending on the type of Medicare plan you are enrolled in, you could potentially lose your benefits for a number of reasons, such as: You no longer have a qualifying disability. You fail to pay your plan premiums. You move outside your plan's coverage area.
Who controls Medicare premiums?
The State of California participates in a buy-in agreement with the Centers for Medicare and Medicaid Services (CMS), whereby Medi-Cal automatically pays Medicare Part B premiums for all Medi-Cal beneficiaries who have Medicare Part B entitlement as reported by Social Security Administration (SSA).
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Does everyone have to pay into Medicare?
While most people do not have to pay a premium for Part A, everyone must pay for Part B if they want it. This monthly premium is deducted from your Social Security, Railroad Retirement, or Civil Service Retirement check.
Can you get kicked off Medicare?
Most beneficiaries can only lose their Medicare coverage if they fail to pay their premiums. There are two scenarios in which you can join Medicare: You qualify because of a disability, or because you turn 65.
Can you be dropped from Medicare?
Medicare Advantage plans can't drop you because of a medical condition. You may be dropped from a Medicare Advantage plan if it becomes unavailable or if it no longer services your area. You may also be dropped from a Medicare Advantage plan if you don't make your payments within an agreed-upon grace period.
How Long Will Medicare last?
A report from Medicare's trustees in April 2020 estimated that the program's Part A trust fund, which subsidizes hospital and other inpatient care, would begin to run out of money in 2026.
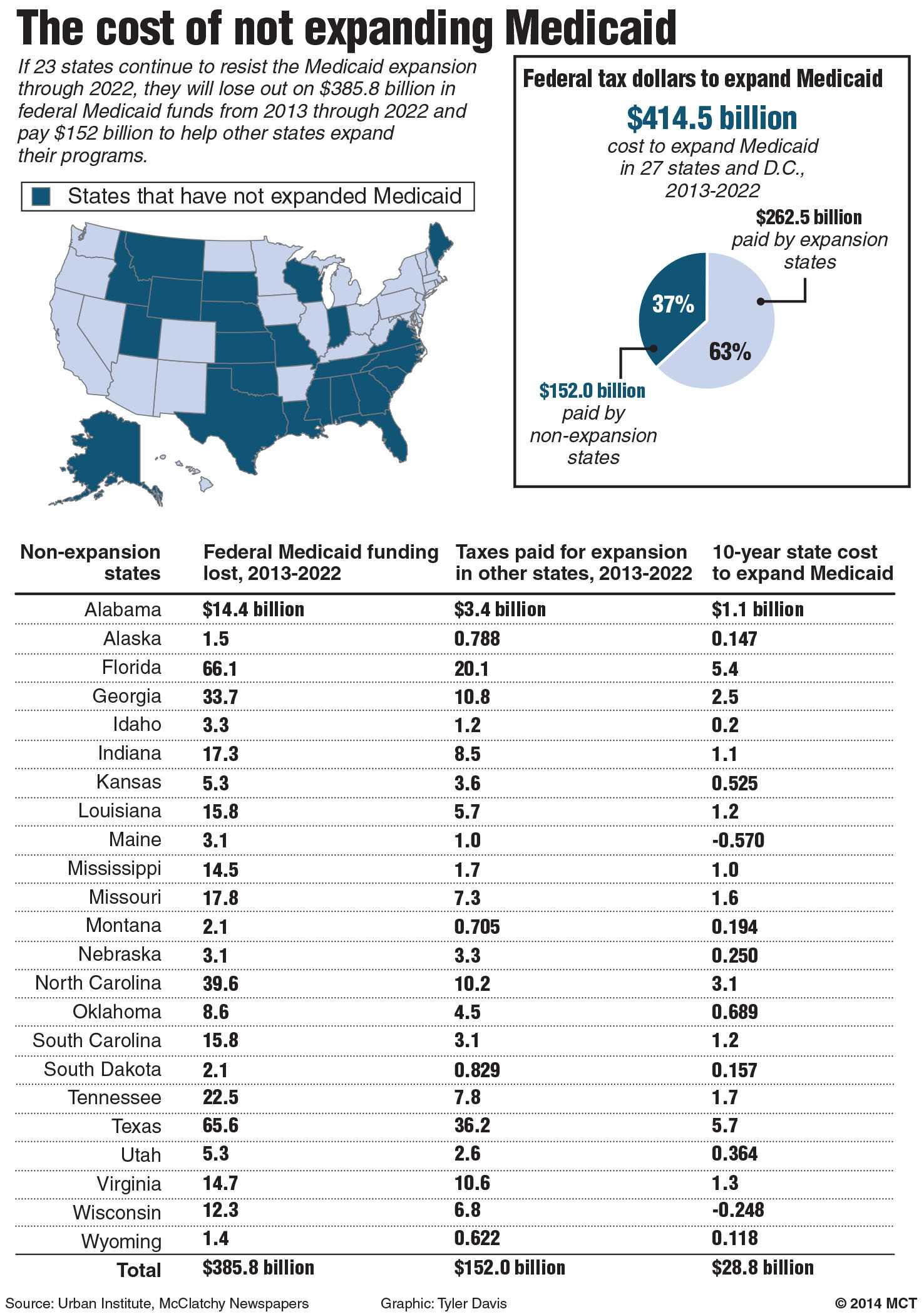
Do states contribute to Medicare?
Medicare is federally administered and covers older or disabled Americans, while Medicaid operates at the state level and covers low-income families and some single adults. Funding for Medicare is done through payroll taxes and premiums paid by recipients. Medicaid is funded by the federal government and each state.
Is Medicare state or federal?
federalMedicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
How does the government pay for Medicare?
Medicare is funded primarily from general revenues (43 percent), payroll taxes (36 percent), and beneficiary premiums (15 percent) (Figure 7). Part A is financed primarily through a 2.9 percent tax on earnings paid by employers and employees (1.45 percent each) (accounting for 88 percent of Part A revenue).
How much does a CWD cost?
People who qualify for the CWD program pay a monthly premium for their full Medi-Cal benefits ranging from $20-$250 for an individual and $30-$375 for a couple. For most people who qualify for the CWD program, paying the monthly premium every month and getting full Medi-Cal benefits is better than having to meet their SOC every month ...
When did the Part B premium stop?
It expands the policy change made in November 2008 when the state stopped paying the Part B premium for people with SOCs over $500. The recent change took effect April 1, 2011; for those affected, the Part B premium will be deducted from their Social Security checks beginning in May 2011.
Does California pay Medicare Part B?
State Stops Paying Medicare Part B Premiums for Beneficiaries with Any Share of Cost Medi- Cal. Medi-Cal is no longer paying the Medicare Part B premium for any Medicare beneficiaries who have Medi-Cal with a Share of Cost (SOC), unless they meet their SOC in a given month.
Does Medi-Cal pay Part B?
Medi-Cal is no longer paying the Medicare Part B premium for any Medicare beneficiaries who have Medi-Cal with a Share of Cost (SOC), unless they meet their SOC in a given month.
SPOTLIGHT & RELEASES
States pay Medicare Part B premiums each month for over 10 million individuals and Part A premium for over 700,000 individuals.
Related Training & Materials
Frequently Asked Questions (FAQs) about Medicare Part A and B "Buy-in" (PDF): The main policy questions, & responses, submitted to CMS to date on the updated Manual for State Payment of Medicare Premiums released on September 8, 2020.
How long does it take to pay Medicare premiums after disenrollment?
If your request is approved, you’ll have to pay your outstanding premiums within three months of disenrollment to resume coverage. If you’re disenrolled from Medicare Advantage, you’ll be automatically enrolled in Original Medicare. During this time, you may lose drug coverage.
What happens if you fail to make your Medicare payment?
Only once you fail to make your payment by the end of your grace period do you risk disenrollment from your plan. In some cases, you’ll be given the option to contact your plan administrator if you’re behind on payments due to an underlying financial difficulty.
How long do you have to pay Medicare Part B?
All told, you’ll have a three-month period to pay an initial Medicare Part B bill. If you don’t, you’ll receive a termination notice informing you that you no longer have coverage. Now if you manage to pay what you owe in premiums within 30 days of that termination notice, you’ll get to continue receiving coverage under Part B.
What happens if you don't pay Medicare?
What happens when you don’t pay your Medicare premiums? A. Failing to pay your Medicare premiums puts you at risk of losing coverage, but that won’t happen without warning. Though Medicare Part A – which covers hospital care – is free for most enrollees, Parts B and D – which cover physician/outpatient/preventive care and prescription drugs, ...
What happens if you miss a premium payment?
But if you opt to pay your premiums manually, you’ll need to make sure to stay on top of them. If you miss a payment, you’ll risk having your coverage dropped – but you’ll be warned of that possibility first.
How long is the grace period for Part C and D?
All Part C and D plans must have a grace period that’s at least two months in length, and some plans have a longer grace period. If you fail to make a premium payment, your plan must send you a written notice of non-payment and tell you when your grace period ends.
When is Medicare Part B due?
Your Medicare Part B payments are due by the 25th of the month following the date of your initial bill. For example, if you get an initial bill on February 27, it will be due by March 25. If you don’t pay by that date, you’ll get a second bill from Medicare asking for that premium payment.
What is extra help for Medicare?
Medicare offers “ Extra Help ” for Medicare enrollees who can’t afford their Part D prescription drug coverage. In 2020, if you’re a single person earning less than $1,615 per month ($2,175 for a couple), with financial resources that don’t exceed $14,610 ($29,160 for a couple), you may be eligible for “Extra Help.”.
How many types of MSPs are there?
There are four different types of MSPs, and they provide varying benefits. Two of the MSPs only help to pay Medicare Part B premiums (but not Part A premiums or Medicare cost sharing), and one MSP helps disabled working individuals pay their Part A premiums.
What is the income limit for Medicare Part A?
The income limits are higher (up to $4,339/month for an individual, and $5,833 for a couple in 2020), but the asset limit is lower, at $4,000 for an individual and $6,000 for a couple.
Why do people apply for MSP?
Medicare urges beneficiaries to apply for MSP benefits if there’s any chance they might be eligible, even if they initially think that their income or resources are too high to qualify. This is particularly important given that states can have more lenient eligibility rules than the federal guidelines.
How much can a single person earn in 2020?
A single person can qualify in 2020 with an income up to $1,296 per month ($1,744/month for a couple). Qualified Individual Program (QI). Helps to pay premiums for Part B. A single person can qualify in 2020 with an income up to $1,456 per month ($1,960/month for a couple). Qualified Disabled and Working Individuals Program (QDWI).
Is Medicare a dual program?
Medicare-Medicaid dual eligibility. People who are eligible for MSPs are covered by Medicare, but receive assistance with premiums (and in some cases, cost-sharing) from the Medicaid program. But some low-income Medicare enrollees are eligible for full Medicaid benefits, in addition to Medicare. About 20 percent of Medicare beneficiaries are dually ...
Does Medicare cover long term care?
Medicare does not cover custodial long-term care, but Medicaid does, if the person has a low income and few assets. Almost two-thirds of the people living in American nursing homes are covered by Medicaid (almost all of them are also covered by Medicare).