From August 1, if the federal government has its way, Medicare will stop paying for GPs to interpret common heart tests called electrocardiograms, or ECGs. Health Minister Greg Hunt says the decision is based on safety advice from a top-level medical expert panel convened by the government to review Medicare rebates.
Full Answer
When does Medicare cover an EKG?
Within 12 months after enrolling in Medicare, you can see your doctor for a “Welcome to Medicare” visit. If your doctor orders an EKG at that time, Part B will cover it as a preventive screening. This is the only time Medicare will cover a routine screening EKG.
Does Medicare cover stress tests and electrocardiograms?
Nuclear stress tests and echocardiographic stress tests include imaging as part of the procedure. No matter what type of stress test you have, Medicare will cover the test if it’s necessary. Coverage falls under Part A if you’re an in-patient, and Part B if you’re not. Medicare Guidelines for a Diagnostic Electrocardiogram
Does Medigap pay for EKG tests?
With Medicare alone, you pay a portion of the bill for an EKG or any other outpatient procedure or doctor visit. But, if you buy a Medigap plan, Medigap can cover the gaps you’d otherwise pay. Depending on the plan you qualify for and choose, you may not owe anything for your medical care.
How much does an EKG cost without insurance?
An EKG costs about $50, according to the American Academy of Family Physicians. The Medicare reimbursement rate may be less. Medicare will pay 80 percent of its current reimbursement rate for the procedure. You can expect to pay the other 20 percent if you don’t have Medigap.

Does Medicare cover echo stress test?
An echocardiogram (echo) is a medical test that provides valuable information on the heart. Medicare usually covers the test if it is medically necessary, and if the provider accepts Medicare assignment.
Does Medicare pay for routine EKG?
Medicare covers echocardiograms if they're medically necessary. Your doctor may order an electrocardiogram, or EKG, to measure your heart's health. Medicare will also pay for one routine screening EKG during your first year on Medicare.
Is a Holter monitor covered by Medicare?
Extended wear Holter(EWH) with monitoring lengths of 3-7 days and 8+ days would be covered by Medicare starting January 2021. All US locations would have the ability to seek payment for these services.
Does Medicare cover pre op EKG?
If I order an EKG and read it, can I bill 93000 or is it bundled into the surgery? Medicare will pay for preoperative tests that are reasonable and necessary.
How much does Medicare reimburse for an EKG?
There is no reimbursement for an ECG unless signs and symptoms or other clinical reasoning exists. (I.e. an ECG as part of a routine exam is not reimbursable.) See Table 2, ICD-9 Codes. ECGs need to be performed by a physician in order to be reimbursable.
What is the average cost of a echocardiogram?
Echocardiograms, on average, can range from $1,000 to $3,000 depending on what type of echocardiogram is performed, the location you choose to have the procedure performed, and whether you add additional services. The average cost of an Echocardiogram in the U.S. is $2,275.
How much does a Holter monitor cost?
How Much Does a Holter Monitoring Cost? On MDsave, the cost of a Holter Monitoring ranges from $209 to $373. Those on high deductible health plans or without insurance can save when they buy their procedure upfront through MDsave.
What is the difference between a cardiac event monitor and a Holter monitor?
Holter monitors record continuously, usually for about 24 to 48 hours. An event monitor does not record continuously. Instead, it records when you activate it. Some event monitors will automatically start recording if an abnormal heart rhythm is detected.
Is a heart monitor considered durable medical equipment?
Note: Pulse tachometers (pulse rate monitors, heart rate monitors) do not meet Aetna's definition of covered durable medical equipment (DME) in that they are not primarily medical in nature and are normally of use in the absence of illness or injury.
Is EKG considered preventive care?
EKG services should not routinely be performed as part of a preventive exam unless the member has signs and symptoms of coronary heart disease, family history or other clinical indications at the visit that would justify the test.
Is an EKG part of an annual physical?
Part of the concern, says Christine Laine, M.D., editor in chief of Annals of Internal Medicine and a senior vice president at the American College of Physicians, is that during an annual exam, your doctor may order tests — such as blood or urine tests, or an electrocardiogram (EKG) — that aren't necessary in otherwise ...
Does Medicare pay for preoperative clearance?
Medicare will pay for all medically necessary preoperative services as described in §15047, subsections C and D.
What percentage of Medicare pays for EKG?
For an EKG in any other setting, Medicare Part B pays 80 percent of the Medicare-approved amount.
When did EKG get removed from IPPE?
As of January 2009, the EKG was removed from the list of mandated services that must be included in the IPPE benefit and makes the EKG an educational, counseling, and referral service to be discussed with the patient and, if necessary, ordered by the physician. This change alleviates physician frustration of having to perform a screening ECG when the patient just had a diagnostic EKG/ECG.
How long does it take for an EKG to be performed?
Medicare covers one screening EKG in the patient’s lifetime in conjunction with the Initial Preventive Physical Exam (IPPE), referred to as the “welcome-to-Medicare” exam, which the patient must have performed within 12 months ...
What is the code for EKG?
Codes to be used for the EKG are: G0402 Initial preventive physical examination; face-to-face visit, services limited to new beneficiary during the first 12 months of Medicare enrollment.
How many leads are in a G0404?
G0404 Electrocardiogram, routine ECG with at least 12 leads; tracing only, without interpretation and report, performed as a screening for the initial preventive examination
What percentage of Medicare is responsible for heart medications?
This means that if you have Original Medicare only and don’t have a form of creditable drug coverage, you may be responsible for 100 percent of the costs related to your heart medications.
What is the purpose of echocardiogram?
Echocardiograms and electrocardiograms are both used to detect heart problems and diagnose heart disease. Echocardiograms use sound waves to produce images of the heart, which allows your doctor to see whether your heart is beating and pumping blood normally.
What percentage of Medicare Part B is covered?
Medicare Part B typically covers 80 percent of the Medicare-approved amount for covered doctor services, such as a medically necessary echocardiogram. You typically pay 20 percent after you meet your Part B deductible.
What is Medicare Advantage Plan?
Medicare Advantage plans are sold by private insurers as an alternative to Original Medicare. By law, every Medicare Advantage plan must provide the same hospital and medical benefits as Medicare Part A and Part B.
Does Medicare cover echocardiograms?
Medicare typically covers echocardiograms if they are ordered by your doctor. Medicare Advantage plans also usually cover echocardiograms when medically necessary, and many Medicare Advantage plans also cover prescription drugs. Medicare Part B may cover echocardiograms if they are ordered by a doctor to treat a medical problem.
Does Medicare cover prescription drugs?
In addition to the standard Part A and Part B benefits, most Medicare Advantage plans cover prescription drugs.
Do you need a prescription for heart disease?
Some heart problems, including cardiovascular disease, may require prescription medications to help treat or manage your condition.
When will Medicare stop paying for ECGs?
July 29, 2020 12.06 am EDT. From August 1, if the federal government has its way, Medicare will stop paying for GPs to interpret common heart tests called electrocardiograms, or ECGs. Health Minister Greg Hunt says the decision is based on safety advice from a top-level medical expert panel convened by the government to review Medicare rebates.
Who recommended Medicare funding all practitioners to take and interpret ECGs?
The taskforce’s heart committee recommended Medicare funding all practitioners to take and interpret ECGs. Dept of Health
How many pages are there in the ECG report?
The 344-page final report of the taskforce’s Cardiac Services Clinical Committee is pretty dry reading, but if you make it as far as page 200 you’ll find it acknowledges the importance of ECGs in general practice. In fact, the report explicitly proposes a new Medicare rebate to “allow all practitioners to take and interpret an ECG when clinically required”.
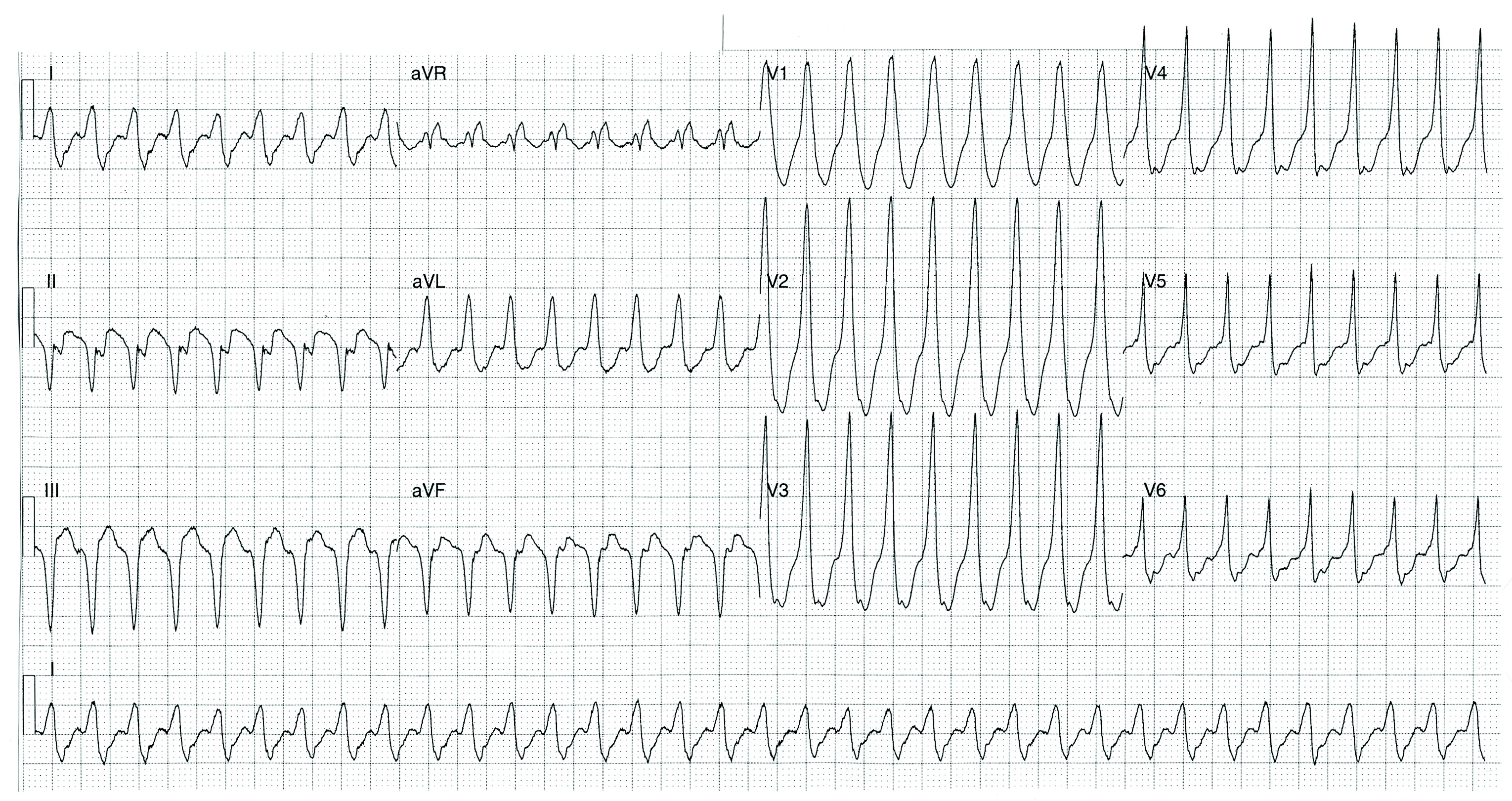
What is an ECG?
ECGs are tracings of the heart’s electrical activity. If you’ve watched a medical drama on TV and seen a flat line on a screen bounce back to a healthy wobbly line as a patient is rescued from cardiac arrest, you’ve seen an example of an ECG – it’s that wobbly line.
What is the Medicare Benefits Schedule Review Taskforce?
The taskforce (formally called the Medicare Benefits Schedule Review Taskforce) has been working to reform the Medicare schedule – that is, the list of medical services funded by Medicare. This is a fine initiative, which brings evidence and expertise to the task of modernising Medicare. Appropriately, it enjoys the bipartisan support of our major parties. It is laudable when the government follows such independent expert advice.
Do Australian general practices have to have ECGs?
ECGs are so fundamental that Australian general practices are required to demonstrate “timely access” to an ECG machine as part of their accreditation.
Who led the Medicare taskforce?
This came from a medical expert panel. It came from what’s known as the Medicare taskforce, led by Prof Bruce Robinson. It’s the highest clinical advice and it was based on safety. A Department of Health spokesperson offered a similar line to the ABC in a news article this week.
Why do you need an EKG?
An EKG might be needed because: You have symptoms that could indicate heart disease, and your doctor wants to confirm or rule out heart problems. You have heart disease, and your doctor wants to monitor your condition. Your doctor orders an EKG before you undergo surgery.
How much does an EKG cost?
An EKG costs about $50, according to the American Academy of Family Physicians. The Medicare reimbursement rate may be less. Medicare will pay 80 percent of its current reimbursement rate for the procedure. You can expect to pay the other 20 percent if you don’t have Medigap.
How to find a Medigap plan?
MedicareFAQ can help you find the Medigap plan that’s right for you. Just call us or fill out our form and we’ll get started on a free quote.
How long does Medicare cover hospitalization?
Part A has a larger deductible, but once you’ve met it, Medicare covers all your hospitalization costs for the first 60 days you’re in the hospital.
What is part B of the cardiologist?
Part B covers tests to diagnose and monitor heart disease. These tests include heart scans.
Why do doctors order stress tests?
Your doctor may order a stress test to find out how well your heart works while you exercise. Most stress tests involve walking on a treadmill or riding a stationary bike.
Do you pay less for EKG with Medicare Advantage?
Advantage plans also have doctor networks. So, you’ll pay less if you use an in-network doctor. If you have Medicare Advantage, EKG coverage follows the same rules as in Medicare. But your costs may be different. To avoid unexpected bills, make sure the doctors administering your EKG are in your plan’s network.
What is the coding code for EKG?
The billing and coding information in this article is dependent on the coverage indications, limitations and/or medical necessity described in the associated LCD Electrocardiographic (EKG or ECG) Monitoring (Holter or Real-Time Monitoring) L34636
How long can you record an electrocardiogram?
External electrocardiographic recording for greater than 48 hours and up to 7 days or for greater than 7 days up to 15 days.
What is the CPT code for Holter Monitoring Services?
1. CPT codes for Holter monitoring services (CPT codes 93224-93227) are intended for up to 48 hours of continuous recording.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Articles. CMS believes that the Internet is an effective method to share Articles that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
Why do contractors need to specify revenue codes?
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination. Complete absence of all Revenue Codes indicates that coverage is not influenced by Revenue Code and the article should be assumed to apply equally to all Revenue Codes.
What codes do not use the 26 modifier?
5. Do not use the "TC" or "26" modifier with the codes 93224-93229, 93268, 93270, 93271, or 93272, listed in the CPT/HCPCS section of the LCD.
Is CPT copyrighted?
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. American Medical Association. All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the American Medical Association (AMA).
What percentage of Medicare does an echocardiogram cost?
To be eligible for Medicare coverage, the health care provider doing the exam must accept Medicare assignment. Part B generally covers 80 percent of the Medicare-approved cost of an echocardiogram. You pay 20 percent of that final approved amount.
Why do doctors use echocardiograms?
Doctors use echocardiogram images to detect heart disease as they examine the heart valves and chambers. Every year in the United States, 20 percent of people who are enrolled in Medicare receive an echocardiogram. With heart disease the number one cause of death in the U.S. for people 65 and over, having medical insurance coverage ...
How much does an echocardiogram cost?
Without Medicare coverage or other health insurance, an echocardiogram costs anywhere from $500.00 to $3,000.00 depending on the normal variables. Generally, these exams are more costly in larger cities. Across the United States, the average price for a standard echo test is $1,500.00.
What is an echocardiogram?
One of the most valuable diagnostic tools for physicians, an echocardiogram (also called an echo test or ECG), is an ultrasound of the heart. Sound waves bounce off the heart to produce real-time images of the organ as it beats and pumps blood through its chambers and into the body. Doctors use echocardiogram images to detect heart disease as they ...
What can a doctor see in an echo?
Your doctors can see whether there is a leakage in the valves or if they are having difficulty opening. They may also be able to detect abnormalities like blood clots, fluid in the pericardium, or problems with the aorta. Using an echo test, doctors can also determine whether the heart’s muscle tissue has been damaged after a heart attack.
What are the symptoms of an echo test?
Your health care provider may order an echo test if you have any of the following symptoms: • A heartbeat that is racing, fluttering, or irregular. • Shortness of breath or trouble breathing.
What do doctors see in a heart exam?
Your doctors can see whether there is a leakage in the valves or if they are having difficulty opening.
Why do you need an echocardiogram?
If you have a shortness of breath or chest pain a doctor may suggest an echocardiogram to diagnose problems with the valves or chambers of the heart, according to the Mayo Clinic. A doctor may use an echocardiogram to find out if there are problems with the outer lining of the heart or problems with the large blood vessels that enter and exit the heart, according to the American Heart Association. An echocardiogram may also detect blood clots in the chambers of the heart and abnormal holes between the chambers of the heart.
What is the difference between an echocardiogram and an electrocardiogram?
An echocardiogram uses sound waves to create pictures of your heart’s chambers, valves, walls and blood vessels, according to the American Heart Association. This test is different from an electrocardiogram, which records the electrical signals of your heart.
How does an echocardiogram work?
During an echocardiogram, a technician passes a probe across your chest which produces sound waves that bounce off your heart and “echo” back to the probe. The soundwaves then are displayed as pictures on a video monitor. An echocardiogram is generally painless and can be done as an outpatient procedure.
What is Medicare Part B?
Medicare Part B covers diagnostic non-laboratory tests, such as echocardiograms, when your health care provider orders them as part of treating a medical problem. These tests may help your doctor diagnose or rule out a suspected illness. An echocardiogram can also help identify whether an area of your heart has been damaged by a heart attack, ...
Does Medicare pay for heart scans?
For diagnostic non-laboratory tests you generally pay 20 percent of the Medicare-approved amount. The Part B deductible also applies. Of course, your costs may be different if you’re enrolled in a Medicare Supplement or Medicare Advantage plan that may pay some or all of your heart scan copayment and deductible.
Why don't you pay copays for emergency department visits?
If your doctor admits you to the same hospital for a related condition within 3 days of your emergency department visit, you don't pay the copayment because your visit is considered part of your inpatient stay.
How much does Medicare pay for a doctor's visit?
For example, you might pay $10 or $20 for a doctor's visit or prescription drug. for each emergency department visit and a copayment for each hospital service. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid.
What does Medicare Part B cover?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. usually covers emergency department services when you have an injury, a sudden illness, or an illness that quickly gets much worse.
Does Medicare cover emergency services in foreign countries?
Medicare covers emergency services in foreign countries only in rare circumstances.
