Many blood tests have limited coverage; that is, a test will be covered only for certain diagnoses. If the diagnosis provided is not one that Medicare accepts as justification for the test, they won’t pay for it. Apparently, the diagnosis provided on the order for your particular test is not one that Medicare accepts.
Full Answer
What is the latest version of ICD-10 L84?
Apr 30, 2018 · We have received notification regarding changes with LCD/NCD for our area. (Knoxville,TN) We normally bill routine foot care codes 11055,11056,11057 with the diagnosis of L85.1 (callus), along with E11.49 (diabetes w/ neuro) OR I73.9 (pvd) as the secondary code and a Q modifier for the class finding. We are being informed that we can no longer ...
Why won’t Medicare pay for a blood test?
Oct 01, 2021 · L84. Corns and callosities Billable Code. L84 is a valid billable ICD-10 diagnosis code for Corns and callosities . It is found in the 2022 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2021 - Sep 30, 2022 . ↓ See below for any exclusions, inclusions or special notations.
What happens if a lab bill is denied by Medicare?
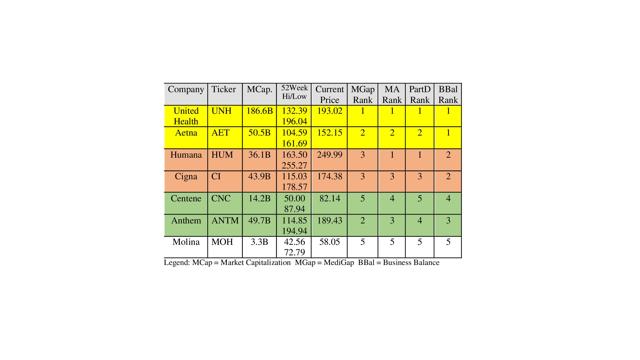
Oct 26, 2017 · Many Medigap plans, supplemental insurance that helps cover the cost of care that Medicare doesn't, will pay 80 percent of billed charges for emergency care that's deemed to be medically necessary ...
What is the ICD 10 code for urticaria L84?
Apr 04, 2017 · This is called the diagnosis. Many blood tests have limited coverage; that is, a test will be covered only for certain diagnoses. If the diagnosis provided is not one that Medicare accepts as justification for the test, they won’t pay for it. Apparently, the diagnosis provided on the order for your particular test is not one that Medicare accepts.
Does Medicare cover code Z00 00?
Coding for this initial exam is unique to Medicare. Though the diagnosis code (ICD-10 code) for the exam is Z00. 00 (general physical exam), the CPT code for the visit is NOT the wellness-exam code range used by every other insurance plan (99381-99397). Instead, it is billed with a Medicare-only code, G0438.Jan 22, 2020
Is ICD-10 covered by Medicare?
The ICD-10 transition is a mandate that applies to all parties covered by HIPAA, not just providers who bill Medicare or Medicaid.
What diagnosis codes are not covered by Medicare?
Non-Covered Diagnosis CodesBiomarkers in Cardiovascular Risk Assessment.Blood Transfusions (NCD 110.7)Blood Product Molecular Antigen Typing.BRCA1 and BRCA2 Genetic Testing.Clinical Diagnostic Laboratory Services.Computed Tomography (NCD 220.1)Genetic Testing for Lynch Syndrome.More items...•Feb 9, 2022
What ICD 10 code will cover hemoglobin a1c?
R73. 09 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM R73. 09 became effective on October 1, 2021.
How many diagnosis codes does Medicare accept?
3. You can list up to four diagnosis pointers per service line. While you can include up to 12 diagnosis codes on a single claim form, only four of those diagnosis codes can map to a specific CPT code.Sep 14, 2015
Is Quest Diagnostics covered by Medicare?
Quest Diagnostics offers many laboratory tests and screening services. Medicare covers tests performed at Quest, as long they're medically necessary and the specific facility accepts Medicare. Medicare Part B or Medicare Advantage (Part C) will cover the cost of your tests.Aug 12, 2020
What procedures are not covered by Medicare?
Some of the items and services Medicare doesn't cover include:Long-Term Care. ... Most dental care.Eye exams related to prescribing glasses.Dentures.Cosmetic surgery.Acupuncture.Hearing aids and exams for fitting them.Routine foot care.
What happens when Medicare denies a claim?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: A request for a health care service, supply, item, or drug you think Medicare should cover.
Does Medicare cover CPT code 87507?
Medicare will allow only one GIP multiplex panel (CPT code 87505, 87506, 87507 or 0097U) per day per beneficiary by the same or different provider consistent with the related LCD.
Does Medicare pay for hemoglobin A1C?
Hemoglobin A1c Tests: Your doctor might order a hemoglobin A1c lab test. This test measures how well your blood glucose has been controlled over the past 3 months. Medicare may cover this test for anyone with diabetes if it is ordered by his or her doctor.
How often does Medicare pay for A1C blood test?
Diabetes: once a year, or up to twice per year if you are higher risk (the A1C test will need to be repeated after 3 months) Heart disease: cholesterol, lipids, and triglycerides screening once every 5 years.
Is diabetes screening covered by Medicare?
Diabetes screenings Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers glucose laboratory test screenings (with or without a carbohydrate challenge) if your doctor determines you're at risk for developing diabetes.
What is the ICd 10 code for corns?
L84 is a valid billable ICD-10 diagnosis code for Corns and callosities . It is found in the 2021 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2020 - Sep 30, 2021 .
What does NEC not elsewhere mean?
NEC Not elsewhere classifiable#N#This abbreviation in the Tabular List represents “other specified”. When a specific code is not available for a condition, the Tabular List includes an NEC entry under a code to identify the code as the “other specified” code.
What is a list of terms?
List of terms is included under some codes. These terms are the conditions for which that code is to be used. The terms may be synonyms of the code title, or, in the case of “other specified” codes, the terms are a list of the various conditions assigned to that code.
What does "excludes2" mean?
An Excludes2 note indicates that the condition excluded is not part of the condition it is excluded from but a patient may have both conditions at the same time. When an Excludes2 note appears under a code it is acceptable to use both the code and the excluded code together.
How long does it take to get help for opioid addiction?
Generally, between 16 and 19 days of rehab services are covered. But as more people seek help as a result of an opioid addiction epidemic that has ravaged many communities throughout the country, Medicare in most cases does not cover the cost of methadone, a commonly used medication to treat opioid dependence.
Does Medicare cover everything?
But like most forms of health insurance, the program won't cover everything. The services Medicare won't help pay for often come as a surprise and can leave people with hefty medical bills.
Does Medicare cover dental care?
Dental and Vision Care. Traditional Medicare does not cover the cost of routine dental care, including dental cleanings, oral exams, fillings and extractions. Eye glasses and contact lenses aren't covered either. Medicare will help pay for some services, however, as long as they are considered medically necessary.
Does Medicare pay for cataract surgery?
Medicare will help pay for some services, however, as long as they are considered medically necessary. For example, cataract surgery and one pair of glasses following the procedure are covered, although you must pay 20 percent of the cost, including a Part B deductible.
Does Medicare Advantage cover dental?
Many Medicare Advantage plans, which are Medicare policies administered by private insurers, may offer benefits to help cover the cost of routine dental and vision care. But Lipschutz cautions that these extra benefits, while nice to have, tend to be quite limited.
Does Medicare cover drug addiction?
Opioid Dependence. Medicare helps pay for both inpatient and outpatient detox for alcoholism and drug addiction, although there are limits to the coverage. "The inpatient stay is covered during the most acute states when medical complications are more probable," Lind says.
What is shine in Florida?
SHINE is an award-winning statewide volunteer program that provides free, unbiased, and confidential counseling and information for people on Medicare, their families and caregivers. SHINE is a program of the Florida Department of Elder Affairs and is administered in partnership with the state’s 11 Aging and Disability Resource Centers (ADRCs). In Brevard County, our ADRC is the Senior Resource Alliance, located in Orlando.
How to contact a shine counselor?
To contact a SHINE volunteer counselor for confidential and unbiased assistance , call the Elder Helpline toll-free at 1-800-963-5337, or call 321-752-8080 locally. SHINE has counseling locations throughout Brevard County. Counselors can assist you by telephone or in person.
What is Lyrica used for?
Lyrica is a common prescription medication that is used to treat pain due to nerve damage. This medication can treat pain that occurs due to a variety of diseases, including diabetes, shingles, spinal cord injury, fibromyalgia, and others. This drug can be highly beneficial for many individuals, and if you use Medicare, ...
Does Medicare cover Lyrica?
Your Medicare benefits can also cover Lyrica if you have a Medicare Advantage (MA) Plan with prescription drug coverage. These MA plans are obtained through private insurance companies, and many of them include prescription drug coverage.
What are the side effects of Lyrica?
There are two common side effects that can occur with Lyrica use: dizziness and sleepiness. On average, around 30 percent of people taking Lyrica experience dizziness and just over 20 percent experience sleepiness.
Is Lyrica a Schedule V drug?
Schedule V drugs are drugs that have only minor potential for abuse, but not as much potential as drugs listed as schedule I through schedule IV.
Does Lyrica help with pain?
Lyrica does not provide instant pain relief. Doses must begin to accumulate in the body for a therapeutic effect to become apparent. For some people, pain relief could be felt within one week of starting the medication, but it may take slightly longer for others. Pain relief may also be related to dosage.
Can you take two meds at the same time?
Also, if you happen to miss a dose, take it as soon as possible and then take the subsequent dose at the scheduled time. However, you should not take two doses at the same time to avoid any potential issues with toxicity.