
So, if Medicare Part A and/or Part B deny a claim for medical services you had or wish to have, generally a Medicare Supplement plan won’t cover it. There might be items and services that a Medicare Supplement plan may cover that Medicare doesn’t typically approve for coverage.
Full Answer
Do you need Medicare Part B to get supplemental coverage?
If you need services Medicare doesn't cover, you'll have to pay for them yourself unless you have other insurance or a Medicare health plan that covers them. If you're not lawfully present in the U.S., Medicare won't pay for your Part A and Part B claims, and you can't enroll in a Medicare Advantage Plan or a Medicare drug plan.
Do you have to pay a premium for Medicare Part B?
Oct 01, 2021 · By paying a monthly premium for a Medicare Supplement plan, you can get financial help with: Paying for your Part A deductible and the share of inpatient care costs not covered by Part A Paying for your doctor bills for Part B services Paying the costs of hospice care not handled by Original Medicare
What doesn’t Medicare supplement insurance pay for?
Use the return envelope that came with your bill, and mail your Medicare payment coupon and payment to: Medicare Premium Collection Center. PO Box 790355. St. Louis, MO 63179-0355. Include your payment coupon with your payment so we can apply your payment to your account.
What are Medicare supplement premiums and how do they work?
So, if Medicare Part A and/or Part B deny a claim for medical services you had or wish to have, generally a Medicare Supplement plan won’t cover it. There might be items and services that a Medicare Supplement plan may cover that Medicare doesn’t typically approve for coverage. An example is emergency medical treatment outside the country (80% of costs up to plan limits).
Does Medicare Part A and B have the same number?
Your card has a Medicare Number that's unique to you — it's not your Social Security Number. This helps protect your identity. The card shows: You have Medicare Part A (listed as HOSPITAL), Part B (listed as MEDICAL), or both.
Which of the following is not covered by Medicare Part B?
But there are still some services that Part B does not pay for. If you're enrolled in the original Medicare program, these gaps in coverage include: Routine services for vision, hearing and dental care — for example, checkups, eyeglasses, hearing aids, dental extractions and dentures.
Is Medicare Part B the same as supplemental?
Part B is part of what's called Original Medicare, along with Part A. Plan B refers to Medicare supplement insurance commonly called Medigap. Part A covers hospital bills and Part B, for which a standard premium is paid, covers outpatient care, medical equipment, and other services.
Does supplemental insurance pay Part B deductible?
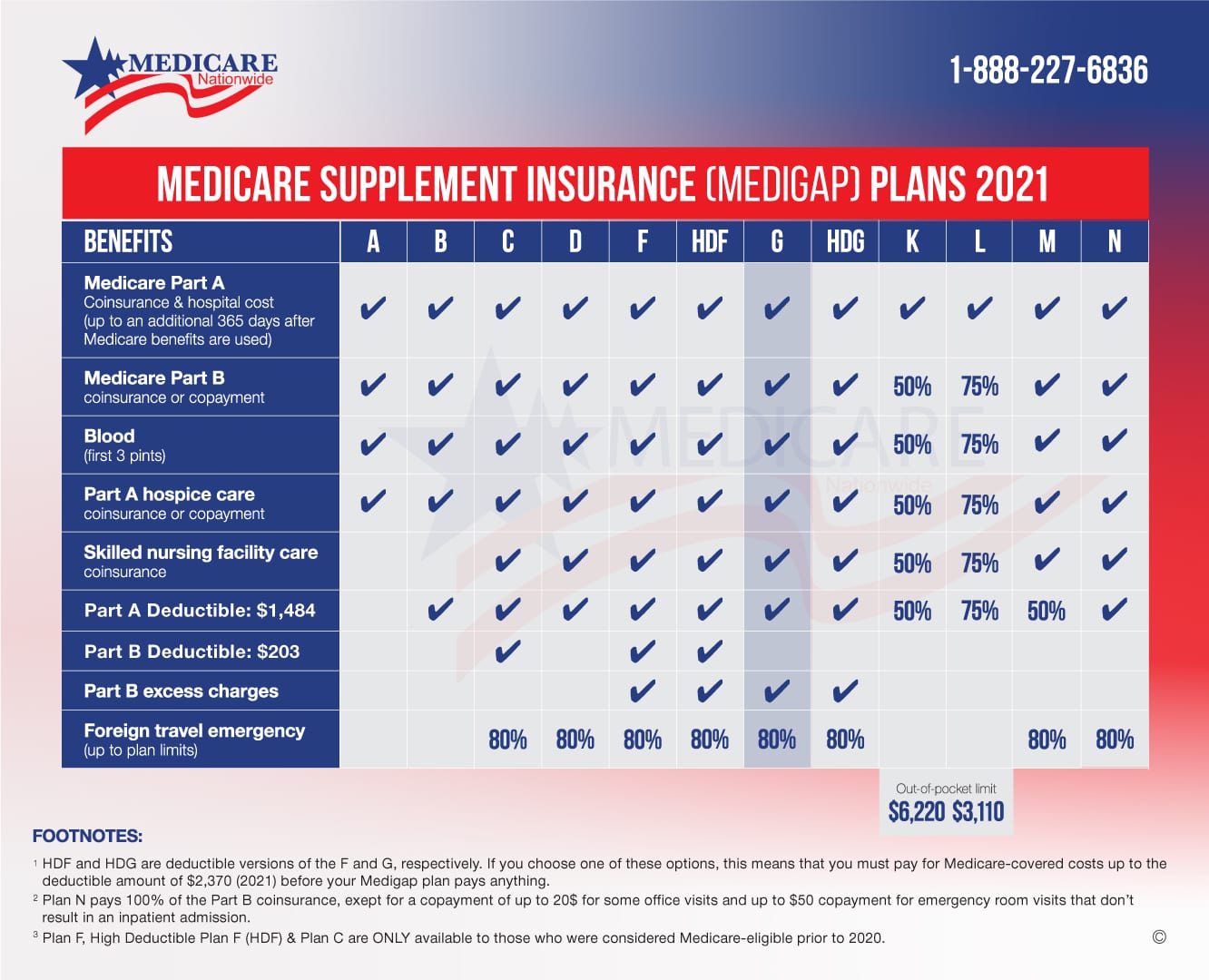
Starting January 1, 2020, Medicare Supplement insurance plans can't cover the Medicare Part B deductible. This eliminates Plan C and Plan F for new beneficiaries. However, if you already have one of these plans, you can keep it.Aug 6, 2021
Which of the following services are covered by Medicare Part B?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services.Sep 11, 2014
Which services are not covered under either Part A or B of the Medicare benefit?
Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing. Long-term supports and services can be provided at home, in the community, in assisted living, or in nursing homes.
Does Medicare Supplement Plan B Cover Part B deductible?
Medicare Supplement insurance plan B does not cover: Medicare Part B deductible. Medicare Part B excess charges. Skilled Nursing Facility care coinsurance.
Does a Medicare Supplement plan pay the Medicare Part B deductible?
(Plans C and F aren't available to people who were newly eligible for Medicare on or after January 1, 2020.) ** For Plans K and L, after you meet your out-of-pocket yearly limit and your yearly Part B deductible, the Medigap plan pays 100% of covered services for the rest of the calendar year.
What is the difference between an Advantage plan and a supplemental plan?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.Oct 1, 2021
Does Medigap cover Part B premium?
The simple answer is no – you cannot use a Medicare Supplement (Medigap) plan to pay your Medicare Part B premium. Medicare Supplement plans are offered by private insurance companies to pay some of the out-of-pocket costs not covered by Medicare Part A (hospital insurance) and Part B (medical insurance).Aug 1, 2021
Is Medigap the same as supplemental?
Are Medigap and Medicare Supplemental Insurance the same thing? En español | Yes. Medigap or Medicare Supplemental Insurance is private health insurance that supplements your Medicare coverage by helping you pay your share of health care costs. You have to buy and pay for Medigap on your own.
How much is the Medicare Part B deductible?
$233The Medicare Part B deductible is $233. Once met, you pay 20 percent of the Medicare-approved amount for most doctor services, outpatient therapy and durable medical equipment.
What is the difference between Medicare Part A and Part B?
First, we need to look at original Medicare, also known as Medicare Parts A and B. Medicare Part A helps cover costs associated with hospital care, and Medicare Part B helps cover costs for things like doctor visits and outpatient procedures. Original Medicare only covers a portion of costs associated with hospital stays and doctor visits.
What is Medicare Part B?
Home health care. Medicare Part B covers the type of care that often takes place outside a hospital or on an outpatient basis. This includes things like: Medically necessary doctor services. Preventive care services, like health screenings, flu vaccines and annual wellness visits to your doctor.
How long does Medicare cover hospitalization?
For example, with Part A, you are responsible for paying a $1,340 deductible before your benefits kick in. After that, if you have a problem that requires hospitalization for up to 60 days, Part A covers your needs. If your stay is more than 60 days , you’ll have to cover part of the price of your stay. And hospital costs can add up quickly, even with Part A chipping in.
What is Medicare Advantage Plan?
An additional way to get drug coverage is to purchase another part of Medicare, called a Medicare Advantage plan. Medicare Advantage plans are sold by private insurance companies and are also known as Medicare Part C. Medicare Advantage plans often include additional coverage, like dental, vision and hearing.
When was Medicare first signed into law?
When Medicare was originally signed into law in 1965 by President Lyndon B. Johnson, it had two complementary parts, A and B. These parts are known as Original Medicare. Part A covered procedures associated with hospital care, and Part B covered outpatient care.
Is Medicare Supplement regulated by Medicare?
By law, Medicare Supplement plans are regulated by Medicare. They vary only in cost and coverage. Medicare Supplement plans even have a few welcome additions. For example, some plans will cover your health care while traveling abroad.
Does Medicare cover everything?
But Medicare supplement plans can help pay for the part of your bills that aren't covered. Finding the coverage that fits you is a key part of navigating Medicare. Keep in mind, Medicare supplement plans might not include everything, but they give you more options to find the coverage that best matches your goals.
Does Medicare Supplement Plan cover emergency medical?
There might be items and services that a Medicare Supplement plan may cover that Medicare doesn’t typically approve for coverage. An example is emergency medical treatment outside the country (80% of costs up to plan limits). However, Medicare might need to approve the treatment even if it doesn’t pay for it.
Does Medicare Supplement Insurance cover copayments?
Summary: With most of its benefits, Medicare Supplement insurance depends on Medicare’s approval in order to help pay Medicare copayments and coinsurance. If Medicare doesn’t cover it, in most cases, neither will Medicare Supplement insurance.
Does Medicare Supplement pay for deductibles?
Medicare Supplement insurance typically helps pay for Medicare Part A and Part B coinsurance and copayments. It also may help pay Original Medicare deductibles and certain other out-of-pocket costs . Medicare Supplement insurance only works alongside Original Medicare, Part A and Part B. As the name implies, it’s a supplement – it adds ...
Does Medicare Supplement cover hospital stays?
If you have a medical service that’s not Medicare-approved, a Medicare Supplement insurance plan generally won’t cover it. For example, Medicare Supplement plans generally cover Medicare Part A coinsurance/copayments for inpatient hospital stays. Suppose you have a hospital stay for a procedure that’s not covered or approved by Medicare.
What is Medicare Supplement Insurance?
Medicare supplement insurance plans, otherwise known as Medigap policies, are designed to help with some of the cost exposure inherent in Original Medicare, such as copayments, coinsurance and deductibles. Some of these policies cover deductibles as well.
How long is the Medicare Supplement enrollment period?
When you are 65 years of age and enrolled in Medicare Part B, you enter your Medicare Supplement Initial Enrollment Period. This is a 6-month period when you have a guaranteed issue right to purchase any Medicare Supplement plan sold in your state.
What is Plan B coverage?
Plan B Coverage. Plan B is one notch above the coverage in Plan A. Basic coverage includes Part A coinsurance and hospital costs for up to 365 additional days after Original Medicare benefits have been exhausted.
Do private insurance companies have to include Medigap?
These regulations require that if a private insurance company elects to offer Medigap policies, they must include plan A in their offering because it is the standard plan for basic coverage. Plan B Coverage.
Does Medicare Advantage include Part D?
Additionally, unlike some Medicare Advantage plans, supplement plans do not include Part D. Therefore, a premium would also be due to the insurance company carrying your drug coverage. It is possible that the company in which you are enrolled for supplement insurance also offers Part D.
Does Plan B cover deductible?
Also, Plan A covers Part B coinsurance or copayments, the first three pints of blood annually, Part A hospice care coinsurance or copayments and skilled nursing facility care coinsurance. Where Plan B becomes advantageous is that it also covers the Part A deductible, which, in 2020, is projected to rise to $1,420.
How much is Part B insurance?
Most people delay Part B in this scenario. Your employer plan likely already provides good outpatient coverage. Part B costs at least $148.50/month for new enrollees in 2020.
How much does Medicare pay for outpatients?
Your healthcare providers will bill Medicare, and Part B will then pay 80% of your outpatient expenses after your small deductible. Medicare then sends the remainder of that bill to your Medigap plan to pay the other 20%. The same goes for Medicare Advantage plans.
How long do you have to enroll in Part B if you retire?
When you retire and lose your employer coverage, you’ll be given a 8-month Special Enrollment Period to enroll in Part B without any late penalty.
What happens if you opt out of Part B?
Be aware that if you opt out of Part B and then later decide to join, you will pay a Part B late penalty. You’ll also need to wait until the next General Enrollment Period to enroll, which means there could be a delay before your coverage becomes active. In my opinion, most Veterans should sign up for Part B.
Does Medigap replace Part B?
Medigap plans do not replace Part B. They pay secondary to Part B. Part B works together with your Medigap plan to provide you full coverage. This means you must be enrolled in Part B before you are even eligible to apply for a Medicare supplement.
Do you have to be enrolled in Part B for Medicaid?
When you are 65 or older and enrolled in Medicaid. All of these scenarios require you to be enrolled in Part B. Without it, you would be responsible for the first 80% of all outpatient charges. Even worse, your secondary coverage may not pay at all if you are not actively enrolled in Part B as your primary coverage.
Do you need Part B before you can enroll in Medigap?
Conclusion. To recap the important points in this article, most people need Part B at some point. When you enroll will depend on what other coverage you currently have when you turn 65. Also, Part B is not a supplement. You need Part B before you can enroll in Medigap or a Medicare Advantage plan.
What is Medicare Part B?
Some people automatically get. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. , and some people need to sign up for Part B. Learn how and when you can sign up for Part B. If you don't sign up for Part B when you're first eligible, ...
What happens if you don't get Part B?
Your Part B premium will be automatically deducted from your benefit payment if you get benefits from one of these: Social Security. Railroad Retirement Board. Office of Personnel Management. If you don’t get these benefit payments, you’ll get a bill. Most people will pay the standard premium amount.
What is the standard Part B premium for 2021?
The standard Part B premium amount in 2021 is $148.50. Most people pay the standard Part B premium amount. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA). IRMAA is an extra charge added to your premium.
How much do you pay for Medicare after you meet your deductible?
After you meet your deductible for the year, you typically pay 20% of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
How much is Part B deductible in 2021?
Part B deductible & coinsurance. In 2021, you pay $203 for your Part B. deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. . After you meet your deductible for the year, you typically pay 20% of the.
Do you pay Medicare premiums if your income is above a certain amount?
If your modified adjusted gross income is above a certain amount, you may pay an Income Related Monthly Adjustment Amount (IRMAA). Medicare uses the modified adjusted gross income reported on your IRS tax return from 2 years ago.
Can Spouses Share The Same Medicare Supplement Policy
by Christian Worstell | Published December 16, 2020 | Reviewed by John Krahnert
B Premium Can Be Limited By Social Security Cola But That Wasnt An Issue For Most Beneficiaries In 2020 Or 2021
In 2021, most enrollees pay $148.50/month for their Part B coverage, which is the standard amount. Most enrollees were also paying the standard amount in 2020 and in 2019 . But thats in contrast with 2017 and 2018, when most enrollees paid a premium that was lower than the standard premium.
What If The Working Spouse Is Not Yet 65 Years Old
A non-working spouse can receive premium-free Medicare part A as long as the other partner is at least 62 years old and has satisfied Medicares work requirements.
Higher Premiums For Enrollees With High
Since 2007, people who earn more than $85,000 have paid higher Part B premiums based on their income.
B Deductible Also Increased For 2021
Medicare B also has a deductible, which increased to $203 in 2021, up from $198 in 2020. After the deductible is met, the enrollee is generally responsible for 20% of the Medicare-approved cost for Part B services. But supplemental coverage often covers these coinsurance charges.
If My Wife And I File A Joint Tax Return Will We Both Be Required To Pay Higher Premiums For Medicare
Both my wife and I collect Social Security. I am still working full time and I earn military retirement pay. My wife works 1 day per week and has very low income. I am 67 and already on Medicare. My wife will turn 65 in may 2020.
Employers Often Bear Costs
But many employers do pay the lion’s share of the cost to add family members, even though they’re not required to do so. In 2020, the average total premiums for family coverage under employer-sponsored plans was $21,342, and employers paid an average of nearly 74% of that total cost.
