
- Eligibility for Medicare. The usual way to qualify for Medicare is to be 65 years of age. ...
- Eligibility for Medicaid. Eligibility for Medicaid depends on the region where a person lives, as some states have different criteria for qualification.
- Dual eligibility. To be eligible to receive both Medicare and Medicaid, a person will need to qualify for either partial-dual or full-dual coverage.
- Geographical variations. Medicaid benefits and coverage can vary widely among states. Some states may expand their Medicaid coverage beyond traditional income limits.
- Summary. A person may qualify for both Medicare and Medicaid based on their health and income level. ...
How do you become dual eligible for Medicare and Medicaid?
- Estate Recovery
- MAGI Conversion Plan
- Seniors & Medicare and Medicaid Enrollees
- Verification Plans
- Minimum Essential Coverage
- Spousal Impoverishment
- Medicaid Third Party Liability & Coordination of Benefits
- Medicaid Eligibility Quality Control Program
Does Someone on Medicaid automatically qualify for Medicare?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
What is dual eligibility for Medicare and Medicaid?
Dual eligibility for Medicare and Medicaid means that you’re enrolled in Medicare and either: receiving full Medicaid benefits; receiving assistance with Medicare premiums
Is Medicare better than Medicaid?
Ultimately, Medicare is a program meant to provide healthcare to Americans age 65 or older (as well as Americans younger than 65 with qualifying disability) while Medicaid is designed to help provide healthcare to low income Americans without any age limit. A few differences between the programs include: Equal but separate.
When can a patient have both Medicare and Medicaid?
Some Americans qualify for both Medicare and Medicaid, and when this happens, it usually means they don't have any out-of-pocket healthcare costs. Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (about 12.3 million people).
What is a partial dual eligible?
“Partial dual eligible” is a term used to describe Medicare beneficiaries who receive financial assistance for certain Medicare costs from their state Medicaid program. These individuals don't qualify for full Medicaid benefits from their state, like long-term services and supports or behavioral health services.
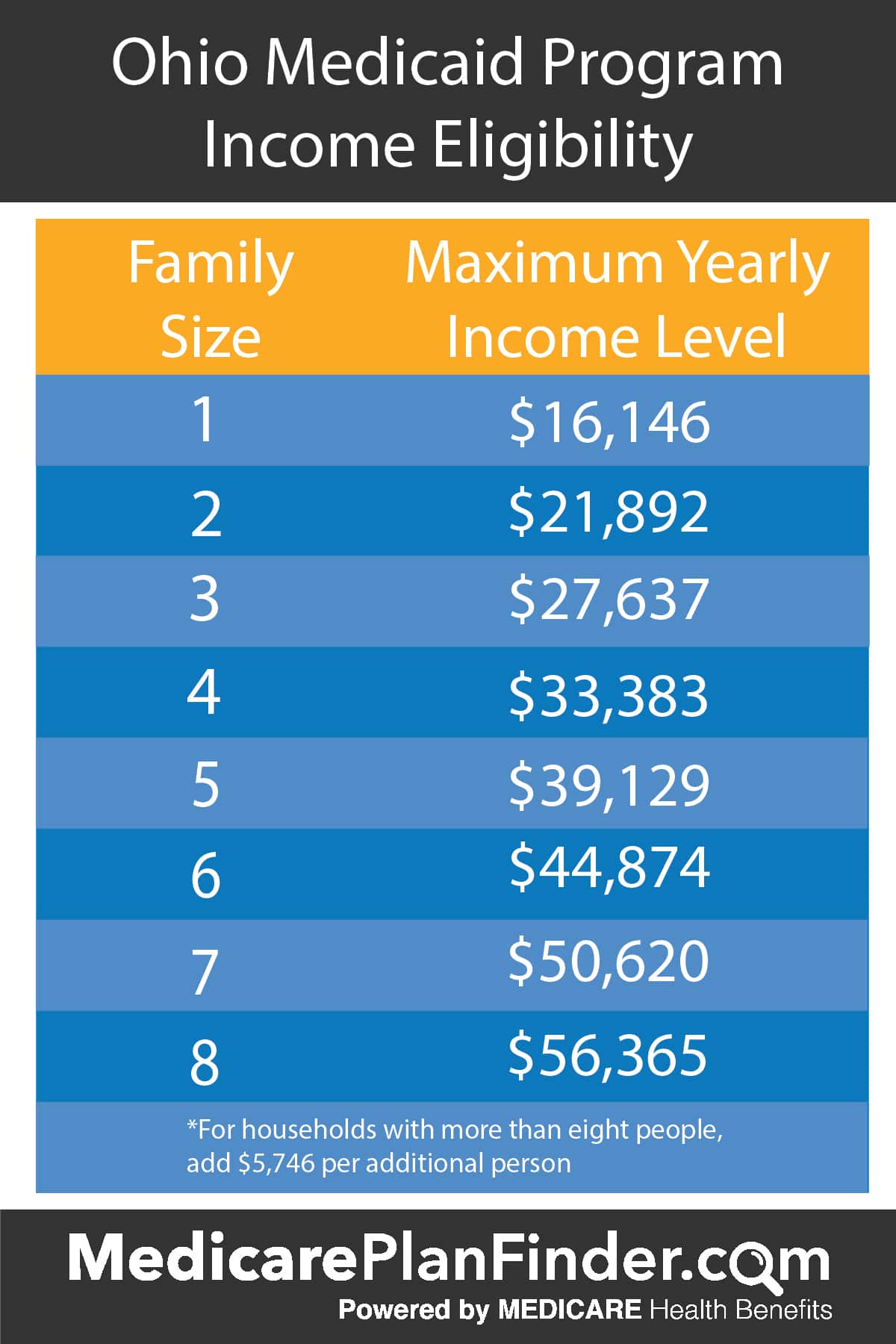
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
When the patient is covered by both Medicare and Medicaid what would be the order of reimbursement?
gov . Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
Which is a combination Medicare and Medicaid option that combines medical social?
What are dual health plans? Dual health plans are designed just for people who have both Medicaid and Medicare. They're a special type of Medicare Part C (Medicare Advantage) plan. Dual health plans combine hospital, medical and prescription drug coverage.
When a patient has Medicaid coverage in addition to other third party payer coverage Medicaid is always considered the?
For individuals who have Medicaid in addition to one or more commercial policy, Medicaid is, again, always the secondary payer.
How do you know if you qualify for Medicaid?
To find out whether you're eligible to receive Medicaid benefits, contact your state Medicaid office. Visit the the Centers for Medicare & Medicaid Services to get the phone number for your state Medicaid office.
Who is qualified for Medicaid?
Medicaid beneficiaries generally must be residents of the state in which they are receiving Medicaid. They must be either citizens of the United States or certain qualified non-citizens, such as lawful permanent residents. In addition, some eligibility groups are limited by age, or by pregnancy or parenting status.
Does Social Security count as income for Medi-Cal?
Most Social Security disability and retirement income does count as income for purposes of Medicaid eligibility. The income figure used to decide whether you are eligible for Medicaid is known as modified adjusted gross income, or MAGI.
When a patient is covered through Medicare and Medicaid which coverage is primary?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors' visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
What does a dual eligible patient mean quizlet?
An individual who is covered by both Medicare and Medicaid is called an. Dual Eligible.
Do I need Medicare Part B if I have Medicaid?
Once you become dual-eligible, most – if not all – of your healthcare costs will be covered. Thus, you are not eligible to enroll in a Medicare Supplement plan. Medicaid covers your Medicare Part A premium (if applicable) and the standard Medicare Part B premium for all eligible enrollees.
How are my health care costs reimbursed if I have Medicare and Medicaid?
When dual eligible beneficiaries have healthcare expenses, Medicare pays first and Medicaid pays last. But this is not the case for things Medicare...
How do I know if I should be dual eligible?
Beneficiaries can find out if they’re eligible for Medicaid by contacting their Medicaid office. An Internet search for Medicaid offices in a benef...
What is the income range for beneficiaries who are dual eligibles?
Generally, beneficiaries earning less than 135 percent of the federal poverty level are eligible for the MSP if they also have limited savings (alt...
Can I select an insurance plan for my Medicare and Medicaid benefits?
If you are dual eligible, you are can enroll in a dual eligible special needs plan (D-SNP) that covers both Medicare and Medicaid benefits. These p...
What is dual eligible Medicare?
Individuals who qualify for both Medicare and Medicaid are known as “dual eligible” and are likely to have most of their healthcare needs covered in some form.
What percentage of Medicare beneficiaries are dual eligible?
Dual eligible individuals account for about 20 percent of Medicare beneficiaries, and are classified into two separate categories.
What is Medicare for seniors?
Medicare is a health insurance program that is designed to help seniors and certain qualifying disabled individuals pay for their health care costs.
How much money do I need to qualify for SSI in 2021?
To qualify for SSI, you must be under a specified income limit (As of 2021: $794 per month for an individual or child, and $1,191 for a couple) and your assets must be considered limited (As of 2021: $2,000 for an individual or child, $3,000 for a couple).
Can dual eligible individuals receive Medicare?
Dual eligible individuals may wish to receive healthcare coverage through Original Medicare Parts A and B. If so decided, the beneficiary would receive Part A and Part B coverage directly with Medicaid serving as a “wrap around” coverage that pays for services that Original Medicare does not cover.
Is Medicare a government program?
While both Medicare and Medicaid are government-regulated health insurance programs, the groups of people they are designed to cover and the level of coverage provided can vary quite dramatically.
Does medicaid cover dental care?
Medicaid typically provides coverage for doctor’s visits, hospital days, long-term healthcare services, preventative care, mental health services, and prescription medication. Children covered under Medicaid may also receive vision and dental coverage. You can find out if you are eligible for Medicaid right here.
What is dual eligible Medicare?
Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (12.1 million people). Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits. Full-benefit dual eligibles have comprehensive Medicaid coverage, ...
How much does a single beneficiary get for Medicaid?
This equates to $17,226 annually for single beneficiaries and $23,274 for married couples. Beneficiaries qualify for full Medicaid benefits if their incomes and assets are even lower (but the exact amounts vary by state).
What is a dual eligible special needs plan?
If you are dual eligible, you are can enroll in a dual eligible special needs plan (D-SNP) that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid don’t over individually, including over-the-counter items, hearing aids, and vision or dental care. Beneficiaries who are dual eligible can ...
Does Medicare pay for long term care?
But this is not the case for things Medicare doesn’t cover, like long-term care. If Medicaid is covering a beneficiary’s long-term care, Medicare will still be the primary payer for any Medicare-covered services – like skilled nursing care or physical therapy.
Is Medicare the same as Medicaid?
The federal government oversees Medicare eligi bility – meaning it is the same in each state. But states set their own eligibility rules for Medicaid and the MSPs (within federal guidelines) – and income limits for these programs vary widely.
Do seniors qualify for medicaid?
Many seniors who live in nursing homes are dual eligible: they qualify for Medicare based on their age, and Medicaid because of their financial circumstances.
Can you switch Medicare Advantage and Original Medicare?
Beneficiaries who are dual eligible can change between Original Medicare and Medicare Advantage or switch Part D plans at each quarter.
How old do you have to be to get medicare?
You’re eligible for Medicare if you’re over the age of 65 or on disability for at least 24 months. Although, you apply for Medicare online at the Social Security Administration website.
How long does it take for medicaid to approve?
Approval time for Medicaid can take up to 60 days. Benefits are for US citizens; but, children of illegal immigrants can qualify. If you get Social Security supplemental benefits, you’ll qualify for Medicaid. Also, Medicaid has benefits Medicare doesn’t; this includes vision, dental, and long-term custodial care.
What is FBDE in Medicare?
Full-Benefit Dual-Eligible (FBDE) individuals are eligible for Medicare as well as full Medicaid benefits through their state. This entitles them to coverage of the following through Medicare Savings Programs: Part A and B premiums, deductibles, coinsurance, and copays.
Is Medicare free for low income people?
With Medicare, think “care” for those 65+ or those with disabilities. Then, Medicaid is “aid” to those with a low income. Medicaid is free. Medicare is not free.
Does medicaid cover Medicare?
Criteria for Medicaid can differ between states. Medicaid pays the part that Medicare doesn’t cover with partial dual-eligibility. Further, Medicaid will cover your Part B premiums, and if applicable, Part A. Beneficiaries who qualify for both are dual-eligible.
Can you collect Medicare and Medicaid?
You can collect both; this is dual-eligibility. Medicare will pay out before Medicaid. Your Medicaid will act like Medigap.
Is Medicare a federal or state program?
But, just because you have one, doesn’t mean you’ll automatically have the other. Medicare is a federal program, while Medicaid is a state program.
What is dual eligible for medicaid?
If you have both Medicare and Medicaid coverage, then your status is called dual-eligible or Medicare dual eligible.
What is medicaid for people over 65?
Medicaid is for people whose incomes are close to the federal poverty line. Today, Medicaid provides extra help paying doctor bills, hospital bills, and prescriptions for millions of Americans aged 65 and over. If you fall into this category, then you’ll want to take a close look at your Medicaid eligibility.
What is QMB in medicaid?
Qualifying Medicaid Beneficiary (QMB) Only. This is for people who are not eligible to receive full Medicaid benefits. Medicaid will pay the recipient’s Medicare Part A premiums (if any). It will also pay their Medicare Part B premium for them.
What is the maximum amount of money you can make on Medicare in 2021?
QI is another category in which Medicaid will only pay your Medicare Part B premium. In 2021, the maximum monthly income is $1,469 for an individual and $1,980 for a couple. For 2021, QI recipients, the maximum asset level allowed is $7,970 for an individual and $11,960 for couples.
What is the maximum income for Medicare Part B 2021?
If you’re an SLMB recipient, Medicaid will pay your Medicare Part B premium. In 2021, the maximum monthly income is $1,308 for an individual and $1,762 for a couple. For 2021, the maximum asset level is $7,970 for an individual and $11,960 for a couple.
How much is Medicare Part B in 2021?
Everybody must pay a Medicare Part B premium of $148.50 monthly in 2021, regardless of income. Can’t afford it? If you qualify for Medicaid, it may pay the premium for you.
Does Medicare help with deductibles?
Besides, there may be extra help with Medicare insurance deductibles and copayments. If you’re a QMB recipient, you chose the Medicare insurance that you like. Then, Medicaid helps with your deductibles and copayments. You will want to have good Medicare insurance, like a Medicare Advantage (Medicare Part C) plan, ...
Why is it important to have both Medicare and Medicaid?
Receiving both Medicare and Medicaid can help decrease healthcare costs for those who are often most in need of treatment.
How old do you have to be to qualify for Medicare?
Eligibility for Medicare. The usual way to qualify for Medicare is to be 65 years of age. A person can receive premium-free Part A (hospital coverage) benefits if they or their spouse is 65 or older and has paid sufficient Medicare taxes through previous employment.
How many people are dually eligible for medicaid?
If a person qualifies for both, the government refers to them as dually eligible. An estimated 12 million people in the United States are dually eligible for Medicare and Medicaid, according to Medicaid.gov. In this article, we discuss eligibility for Medicare and Medicaid, as well as what to know about each program.
What is Medicare Part B?
They can also qualify for Medicare Part B, which is medical coverage for doctor visits and many other medical-related expenses.
What is the age limit for Medicare?
Medicare. Medicare is an insurance plan for people at or over the age of 65 and for others with qualifying medical concerns. A person must meet eligibility criteria based on their work history or that of their spouse. They can qualify for premium-free hospital coverage and pay a premium for medical and prescription drug coverage.
How often does medicaid change?
Medicaid standards can change every year. If a person was unsuccessful in a prior application, they might qualify at a later date. One of the most important factors for Medicaid eligibility is where a person falls on the Federal Poverty Level (FPL).
What is Medicaid insurance?
Medicaid is a health insurance program providing financial assistance to individuals and families with a low income or limited financial resources. The federal government sets rules and regulations regarding Medicaid, and individual states are responsible for operating Medicaid programs.
What is a qualified Medicare beneficiary?
Qualified Medicare Beneficiary: This is the highest level of coverage, meaning beneficiaries receive help with Part A and Part B premiums, co-insurance, co-payments and deductibles.
What is a qualified disabled working individual?
Qualified Disabled Working Individual: As the name suggests, this is for those who are disabled but still working. Beneficiaries receive help with Part A premiums.
Is Medicare the same as Medicaid?
Eligibility for Medicare is set at a federal level, which means the standards are the same nationwide. In contrast, Medicaid is administered by individual states. There are federal mandates to cover certain groups, such as those who have an income that is below 133% of the federal poverty level. Outside of those mandates, however, each state can set its own requirements for Medicaid.
Can seniors get Medicaid?
In addition to Medicaid, many seniors may be eligible for other assistance, depending on the state they reside in. For example, many states offer a Home and Community Based Services waiver that provides support with all or part of the cost of assisted living or other long-term care. These waivers can help seniors who require support beyond the hospital stays, prescriptions and other services covered by Medicare.
Is Medicare a separate program?
Medicare and Medicaid are two separate programs, each with different eligibility requirements. Individuals must enroll on Medicare and Medicaid separately. All seniors who are eligible for retirement Social Security benefits are entitled to Medicare. In addition, many people who are living with a disability will be able to claim Medicaid.
What are the eligibility requirements for Medicaid?
The eligibility requirements vary from state to state, but generally states consider your annual income and financial assets when determining whether you are eligible for full Medicaid.
Who pays for medicaid?
Medicaid is funded by both the federal and state governments. While there are some national eligibility and benefit requirements, each state has its own Medicaid eligibility standards and decides which optional services it will cover and how much it is willing to pay for health care that Medicare doesn’t cover.
How much is Medicare Part B?
The premium for Medicare Part B, which covers doctor visits and other outpatient services. That monthly premium will be $135.50 in 2019.
What is QDWI in Medicare?
The Qualified Disabled and Working Individuals (QDWI) program only helps pay for Medicare Part A (hospital insurance) premiums. This program is designed for individuals with disabilities, under age 65, who are currently working and lost their premium-free Part A benefit when they began to work.
What is the maximum income for Medicare?
For 2018, the limits for those programs are $7,560 for a single person and $11,340 for a married person living with a spouse and no dependents. As with full Medicaid, some states have higher resource thresholds.
What is excluded from the $2,000 asset test?
Excluded from the $2,000 asset test are such things as your home, one car, some burial expenses, some life insurance and household and personal items. States generally look back at an applicant’s assets for five years to make sure they haven’t divested themselves of those resources just to qualify for Medicaid.
Does Medicare cover deductibles?
The Medicare Part D premium, deductibles and copays for prescription drugs. Coverage for those costs is available through the Extra Help program, which Medicaid and Medicare Savings Program enrollees automatically qualify for. Nursing home care and home- and community-based long-term services and supports. In some states, Medicaid will cover ...
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is not covered by Medicare?
Offers benefits not normally covered by Medicare, like nursing home care and personal care services
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare cover health care?
If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
What is dual eligible for Medicare?
Eligibility for the Medicare Savings Programs, through which Medicaid pays Medicare premiums, deductibles, and/or coinsurance costs for beneficiaries eligible for both programs (often referred to as dual eligibles) is determined using SSI methodologies..
How many people are covered by medicaid?
Medicaid is a joint federal and state program that, together with the Children’s Health Insurance Program (CHIP), provides health coverage to over 72.5 million Americans, including children, pregnant women, parents, seniors, and individuals with disabilities. Medicaid is the single largest source of health coverage in the United States.
What is MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents, and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid. MAGI replaced the former process for calculating Medicaid eligibility, ...
What is the Medicaid age limit?
The Affordable Care Act of 2010 created the opportunity for states to expand Medicaid to cover nearly all low-income Americans under age 65 . Eligibility for children was extended to at least 133% of the federal poverty level (FPL) in every state (most states cover children to higher income levels), and states were given the option to extend eligibility to adults with income at or below 133% of the FPL. Most states have chosen to expand coverage to adults, and those that have not yet expanded may choose to do so at any time. See if your state has expanded Medicaid coverage to low-income adults.
What is Medicaid coverage?
Medicaid is the single largest source of health coverage in the United States. To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, ...
How long does medicaid last?
Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
Does Medicaid require income?
Certain Medicaid eligibility groups do not require a determination of income by the Medicaid agency. This coverage may be based on enrollment in another program, such as SSI or the breast and cervical cancer treatment and prevention program.

What Is The Difference Between Medicare and Medicaid?
Is It Possible to Be Eligible For Both Medicare and Medicaid?
- It may come as a surprise to many, but the answer to this question is yes: it is indeed possible to qualify for both Medicare and Medicaid simultaneously. This status is known as dual eligibility, and may give you access to more comprehensive benefits than you otherwise would have. If you are a dual eligible individual, you are likely to have most ...
Full-Benefit Dual Eligibility
- Full-benefit dual eligibles are individuals who have access to comprehensive Medicaid coverage and are also enrolled in Medicare coverage. Remember that Medicaid eligibility requirements vary by state, so it is important to refer to your state’s guidelines before exploring your possible benefits under dual eligibility. Generally, however, people who qualify for full dual eligible covera…
Partial-Benefit Dual Eligibility
- Typically, those who are considered partial-benefit dual eligibles do not receive full Medicaid coverage and usually fall into one of the following Medicare Savings Program (MSP)categories: