Other examples of how Medicare supplement plans work with Medicare include:
- All plans include coverage for blood work at varying levels; Plan K covers it 50 percent and Plan L covers it at 75...
- If you have to endure a lengthy hospital stay, a Medicare supplement plan can save you money. For example, coinsurance...
- Medicare supplement plans don’t cover routine dental or...
Full Answer
Are Medicare supplement plans worth it?
Medicare Supplement plans work together with Original Medicare. First, Medicare pays for a percentage, usually 80 percent, of the Medicare-approved cost of your health care service. After this is paid, your supplement policy pays your portion of …
How do I pick a Medicare supplement plan?
You join a plan offered by Medicare-approved private companies that follow rules set by Medicare. Each plan can have different rules for how you get services, like needing referrals to see a specialist. Costs for monthly premiums and services you get vary depending on which plan you join. Plans must cover all emergency and urgent care, and almost all medically necessary …
What are PFFS Medicare plans and how do they work?
Medigap is Medicare Supplement Insurance that helps fill "gaps" in . Original Medicare and is sold by private companies. Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Copayments
Which Medicare supplement plan should I buy?
Dec 23, 2021 · Medicare Supplement plans, also known as Medigap, are supplement insurance plans that work with Original Medicare Part A and Part B. Simply put, they are designed to fill in the gaps found in Medicare to reduce your out-of-pocket healthcare costs. For many seniors, Medicare and Medicare Supplement insurance can be confusing or even overwhelming …

How are Medicare supplements divided?
What is the point of Medicare Supplement plan?
What are the disadvantages of a Medicare Advantage plan?
- Restrictive plans can limit covered services and medical providers.
- May have higher copays, deductibles and other out-of-pocket costs.
- Beneficiaries required to pay the Part B deductible.
- Costs of health care are not always apparent up front.
- Type of plan availability varies by region.
Are Medicare supplements based on income?
Is there a Medicare supplement that covers everything?
Why do doctors not like Medicare Advantage plans?
What is the difference between Medicare Supplement and Advantage plans?
Who is the largest Medicare Advantage provider?
Can I drop my Medicare Advantage plan and go back to original Medicare?
Can you be denied a Medicare supplement plan?
Why is my Medicare supplement so expensive?
What does a Medicare supplement plan cost?
Is Medicare Supplement the same as Medicare Advantage?
Medicare supplement plans are not the same as Medicare Advantage plans. People use Medicare Advantage plans as an alternative to Medicare parts A and B. Private companies sell and administer them, just as they do Medicare supplement plans.
Can you cancel a Medicare supplement plan if you are married?
Medicare supplement policies have “guaranteed renewable” status. This means that the company cannot cancel the policy as long as a person continues to pay their premium.
Does Medicare cover out of pocket medical expenses?
Medicare is the federal government health coverage program for adults over 65 years of age and people with certain disabilities. However, it does not cover all out-of-pocket healthcare costs. Medicare supplement plans, or Medigap policies, can help.
What is a coinsurance for Medicare?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is a copayment for Medicare?
Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs. This article explains how Medicare supplement plans work, how to find one, and how to work out which plan is best.
Do all companies have to follow Medicare regulations?
However, all companies must make sure that they follow state and federal regulations established by Medicare. Regulations state that a specific Medigap plan must provide the same level of basic coverage, regardless of which private insurer provides it.
Does Plan M cover the same people in different states?
This also means that coverage is the same across different states. For example, coverage on Plan M will be the same in California as it is in Arizona.
How does Original Medicare work?
Original Medicare covers most, but not all of the costs for approved health care services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them.
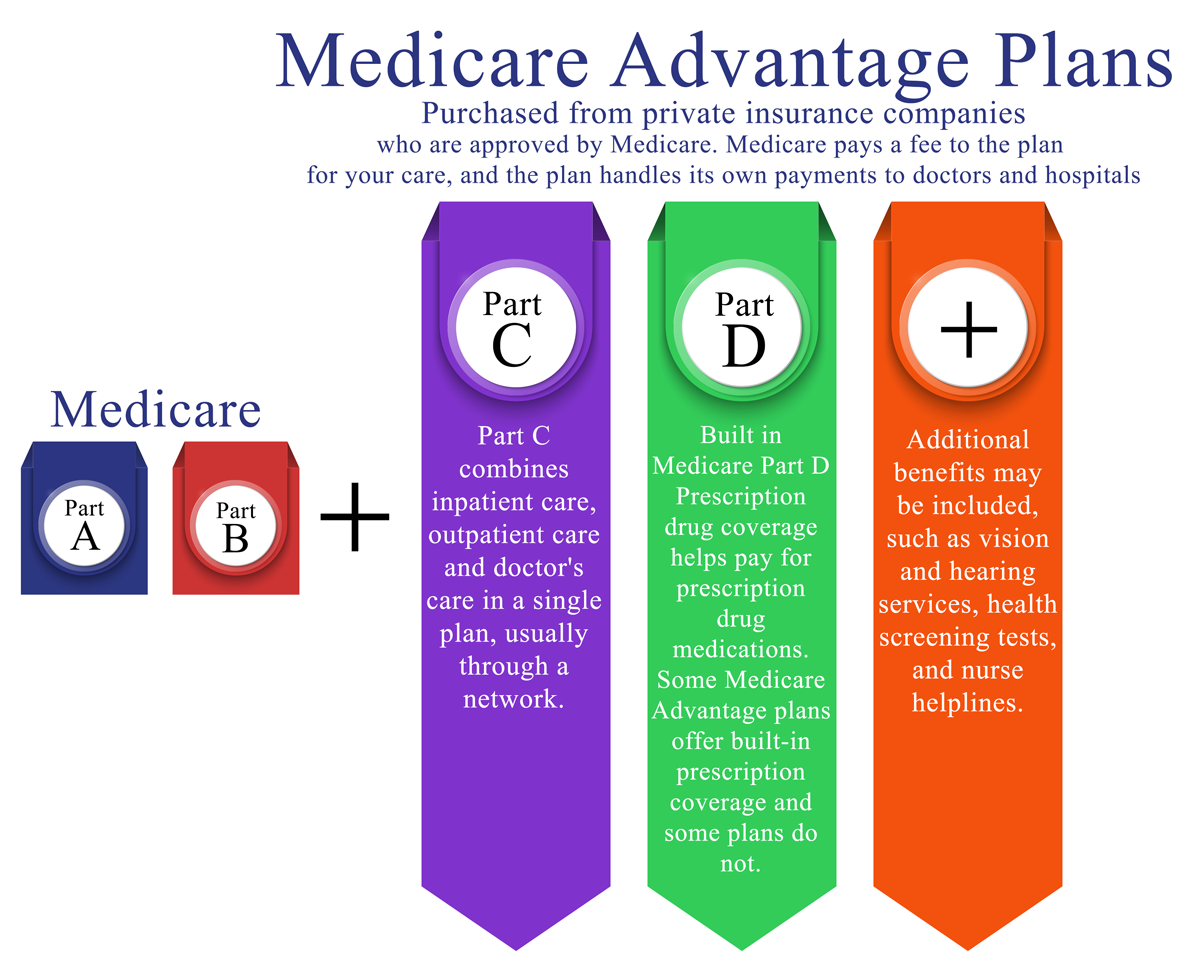
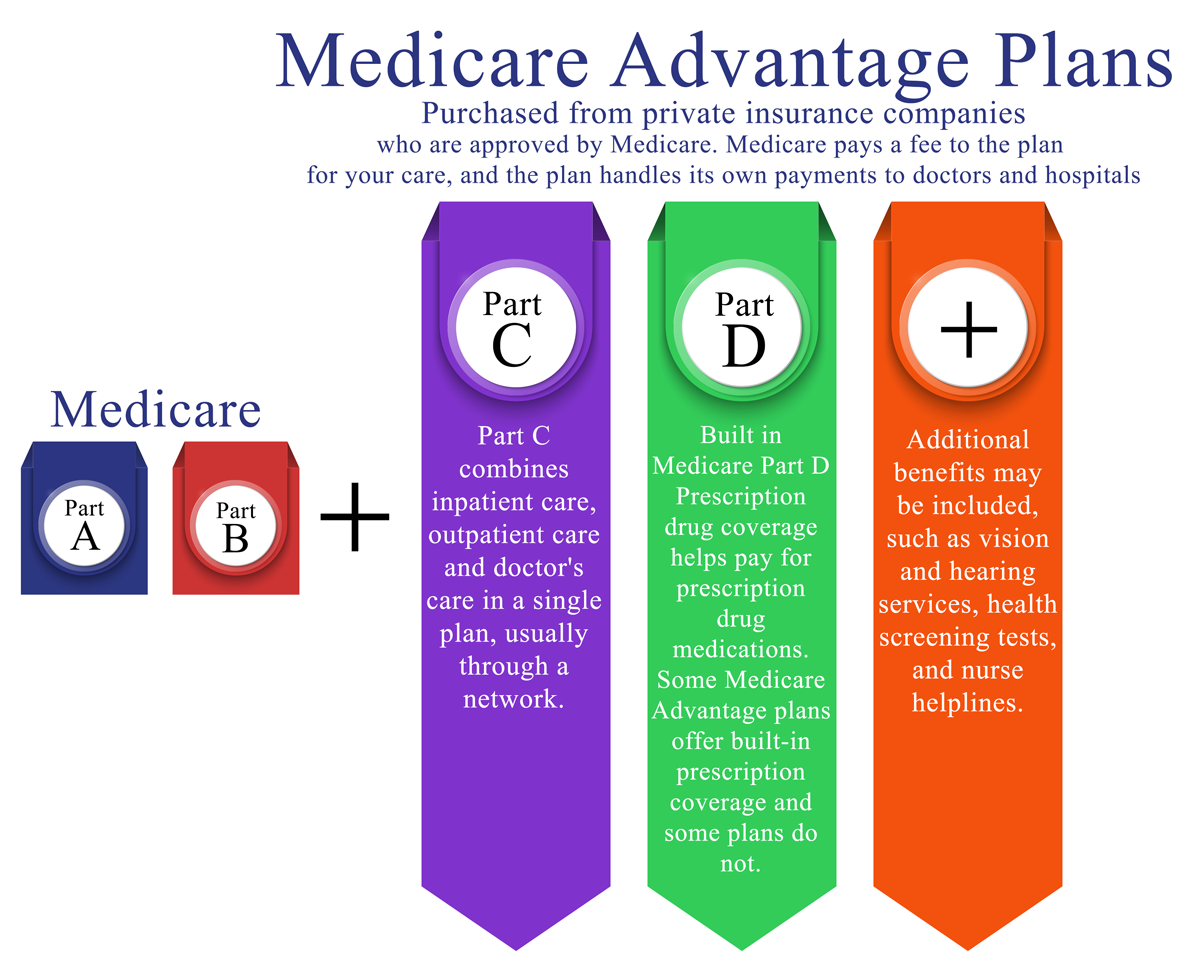
How does Medicare Advantage work?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
Does Medicare Supplement Insurance cover Part B?
A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible. Because of this, Plans C and F aren’t available to people newly eligible for Medicare on or after January 1, 2020.
Does Medicare pay its share of the approved amount?
Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
Does Medicare pay for all of the costs?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Copayments. Coinsurance. Deductibles.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. for covered health care costs.
What is a Medicare premium?
premium. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person.
What are Medicare Supplement Plans?
Medicare Supplement plans, also known as Medigap, are supplement insurance plans that work with Original Medicare Part A and Part B.
Who Regulates Medicare Supplement Plans?
Although Medicare Supplements (Medigap) plans are sold by private insurance companies, the federal government (CMS) regulates each plan’s design in terms of coverages offered.
How Does Medicare Supplement Plans Work?
While there are 10 Medigap plans to choose from in all but three states, each plan, although different from the next, works in the same manner. Medicare would pay its share and then the Medicare Supplement Plan would pay its share.
Which Medicare Supplement Plans Provide the Best Coverage?
Having multiple Medigap plans to choose from enables the policy shopper to select a plan that will best meet their individual needs and their individual budget. It’s also important to keep in mind that the Medigap Plan you select will have a monthly premium charge over and above your Medicare Part B premium.
What are High-Deductible Medicare Supplement Plans?
There are two high-deductible Medicare Supplement Plans available. High deductible Plan F and Plan G both have a regular version and a “high-deductible” version. Since the policyholder is agreeing to accept more out-of-pocket expenses for their annual healthcare expenses, the insurance company offers the plan at a lower monthly premium.
Do Medicare Advantage and Medicare Supplement work together?
Medicare Advantage and Medicare supplement plans do not work together – you have to choose one or the other. If you choose the original Medicare option, Medicare supplement plans are important because these plans add an extra element, or boost, to your main coverage by paying for gaps for stand-alone prescription drug plans, ...
Why is Medicare Supplement important?
If you choose the original Medicare option, Medicare supplement plans are important because these plans add an extra element, or boost, to your main coverage by paying for gaps for stand-alone prescription drug plans, employer group health coverage and other retiree benefits. Original Medicare will pay first, followed by the payment by ...
What are the benefits of Medicare?
There are up to 10 standardized plans available – labeled A, B, C, D, F, G, K, L, M and N – that cover anywhere from four to nine of these benefits: 1 Medicare Part A coinsurance for hospital costs (up to an additional 365 days after Medicare benefits are used) 2 Medicare Part B coinsurance, copayment 3 First three pints of blood for a medical procedure 4 Part A hospice care coinsurance or copayment 5 Skilled nursing facility care coinsurance 6 Part A deductible 7 Part B deductible 8 Part B excess charges 9 Foreign travel emergencies
How many Medicare supplement plans are there?
How Medicare supplement insurance plans work with Medicare plans. There are up to 10 standardized plans available – labeled A, B, C, D, F, G, K, L, M and N – that cover anywhere from four to nine of these benefits:
How long does Medicare cover hospital coinsurance?
Medicare Part A coinsurance for hospital costs (up to an additional 365 days after Medicare benefits are used) Keep in mind, all 10 Medicare supplement plans cover the coinsurance and 100 percent of hospital costs for Medicare Part A, but after that, plans differ in what they cover. For example, only Medicare supplement plans C and F cover ...
Does Medicare cover blood work?
For example, only Medicare supplement plans C and F cover the deductible of Part B. Other examples of how Medicare supplement plans work with Medicare include: All plans include coverage for blood work at varying levels; Plan K covers it 50 percent and Plan L covers it at 75 percent. The remaining eight plans fully cover blood work at 100 percent.
Do you have to leave Medicare first?
If you have a Medicare Advantage Plan, you must leave it first before your new Medicare supplement (Medigap) policy begins; apply for the Medigap plan first before you leave your other plan. Buy a Medigap policy from an insurance company licensed in your state to sell them.
What is Medicare Supplemental Insurance?
Medicare supplemental insurance — or Medigap — plans are policies that private insurance companies sell to people with traditional Medicare. These policies help reduce Medicare’s out-of-pocket costs. Examples of out-of-pocket costs include copayments, deductibles, and costs for blood transfusions. Learning the amounts of these costs can help ...
What does Medigap cover?
Medigap policies cover the following out-of-pocket costs for people with traditional Medicare: coinsurance. copayments. deductibles. The Centers for Medicare & Medicaid Services mandate that Medigap policies must provide the same level of coverage, regardless of which company is administering them. Medigap policies range from A to N.
Does Medigap cover dental?
It is important to note that Medigap plans do not cover some elements of care. Examples include long-term care, dental care, eyeglasses, private-duty nursing, and hearing aids. Also, several states have Medicare waivers, including Massachusetts, Minnesota, and Wisconsin.
Can every private insurance company sell every Medigap plan?
This will help the person make the best decision, according to their healthcare needs. However, policy changes mean that not every private insurer can sell every Medigap plan. For example, as of January 1, 2020, private insurance companies can no longer offer Plans C and F to newly enrolled people.
Can you sell every Medigap plan?
However, policy changes mean that not every private insurer can sell every Medigap plan. For example, as of January 1, 2020, private insurance companies can no longer offer Plans C and F to newly enrolled people. If a person enrolled in one of these plans before January 1, 2020, they can typically keep it.
What is a coinsurance for Medicare?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
Does Medicare cover out of pocket costs?
Private insurance companies sell and administer Medicare supplemental insurance, or Medigap. They partially cover traditional Medicare’s out-of-pocket costs. If a person has Medicare Advantage, they cannot also have a Medigap plan. Medigap policies cover the following out-of-pocket costs for people with traditional Medicare: coinsurance.
How does Medicare Supplement insurance work?
A Medicare Supplement insurance plan will have a monthly premium cost that you pay to the private insurance company that you purchased the plan through. You’ll pay your monthly Medigap policy premium separately of any Medicare premiums. Costs can vary widely for Medicare Supplement plans because they are offered through private insurance companies, ...
What is Medicare Supplement?
Medicare Supplement insurance plans are private insurance plans that are offered to help bridge the gap between the coverage you need and what is offered through Medicare. While Medicare pays for a large percentage of the healthcare services and supplies you may need, it does not offer complete coverage, so Medicare Supplement insurance plans can ...
Why is Medicare Supplement Insurance called Medigap?
Medicare Supplement insurance plans are often referred to as Medigap policies, because they can help fill the gap between Medicare and healthcare needs. Many people use Medigap policies to help cover the costs of associated healthcare expenses, such as coinsurance payments, copays and deductibles.
Does Medicare cover hospital coinsurance?
Medicare.gov offers an in-depth look at the precise coverage of each plan, but in general, Medigap policies will either fully cover, partially cover, or not cover the following services and supplies: Part A coinsurance and hospital costs up to an additional 365 days after Medicare benefits are used up.
How long after Medicare benefits are used up can you get a coinsurance?
Part A coinsurance and hospital costs up to an additional 365 days after Medicare benefits are used up. Part B coinsurance or copayment. The first three pints of blood. Part A hospice care coinsurance or copayment. Skilled nursing facility care coinsurance. Part A deductible.
What happens when you buy a Medicare Supplement?
When you purchase a Medicare Supplement insurance plan, your Medigap policy will serve as a secondary source of insurance. That means that Medicare will be used first to pay for any Medicare-approved costs for any healthcare supplies and services. After Medicare has been applied, then your Medigap policy will be charged.
Does Medicare charge for Medigap?
After Medicare has been applied, then your Medigap policy will be charged. In most cases, there is nothing additional you need to do in order to submit a claim to your Medigap plan, as most doctors and healthcare facilities will automatically bill your Medigap plan.