For qualifying individuals, Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
How does Medicare Part a pay for skilled nursing?
Medicare Part A will help pay for skilled nursing care for up to 100 days at a time. Called a "benefit period," these benefits reset when you've stopped receiving skilled nursing care for 60 consecutive days. Your Part A benefits work like this: Medicare Part A pays all of your costs for the first 20 days.
Does Medicare pay for nursing home care?
While Medicare benefits do help recipients with the cost of routine doctor visits, hospital bills and prescription drugs, the program is limited in its coverage of nursing home care. This is because nursing home care varies greatly in terms of scope and amenities.
What do I pay for skilled nursing facility care in 2019?
What do I pay for skilled nursing facility (SNF) care in 2019? In Original Medicare, for each benefit period, you pay: For days 1–20: You pay nothing for covered services. Medicare pays the full cost. For days 21–100: You pay up to $170.50 per day for covered services. Medicare pays all but the daily coinsurance.
Does Medicare cover 100 days at a skilled nursing facility?
Medicare covers up to 100 days at a skilled nursing facility. Medicare Part A and Part B cover skilled nursing facility stays of up to 100 days for older people who require care from people with medical skills, such as sterile bandage changes.

How many days will Medicare pay 100% of the covered costs of care in a skilled nursing care facility?
20 daysSkilled Nursing Facility (SNF) Care Medicare pays 100% of the first 20 days of a covered SNF stay. A copayment of $194.50 per day (in 2022) is required for days 21-100 if Medicare approves your stay.
Which of the three types of care in the nursing home will Medicare pay for?
Original Medicare and Medicare Advantage will pay for the cost of skilled nursing, including the custodial care provided in the skilled nursing home for a limited time, provided 1) the care is for recovery from illness or injury – not for a chronic condition and 2) it is preceded by a hospital stay of at least three ...
Does Medicare pays most of the costs associated with nursing home care?
Medicare doesn't pay anything toward the considerable cost of staying in a nursing home or other facility for long-term care.
What does Medicare Part B cover in a nursing home?
Original Medicare Part A covers inpatient hospital care, skilled nursing facility care, and hospice stays. Part B provides coverage for outpatient services, such as visits to a doctor's office, durable medical equipment, therapeutic services, and some limited prescription medication.
What is the 100 day rule for Medicare?
Medicare pays for post care for 100 days per hospital case (stay). You must be ADMITTED into the hospital and stay for three midnights to qualify for the 100 days of paid insurance. Medicare pays 100% of the bill for the first 20 days.
What are the two levels of care in nursing homes?
Federal regulation for Medicaid providers specifies two levels of care, SNF and ICF, with standards for each level set by States within Federal guidelines.
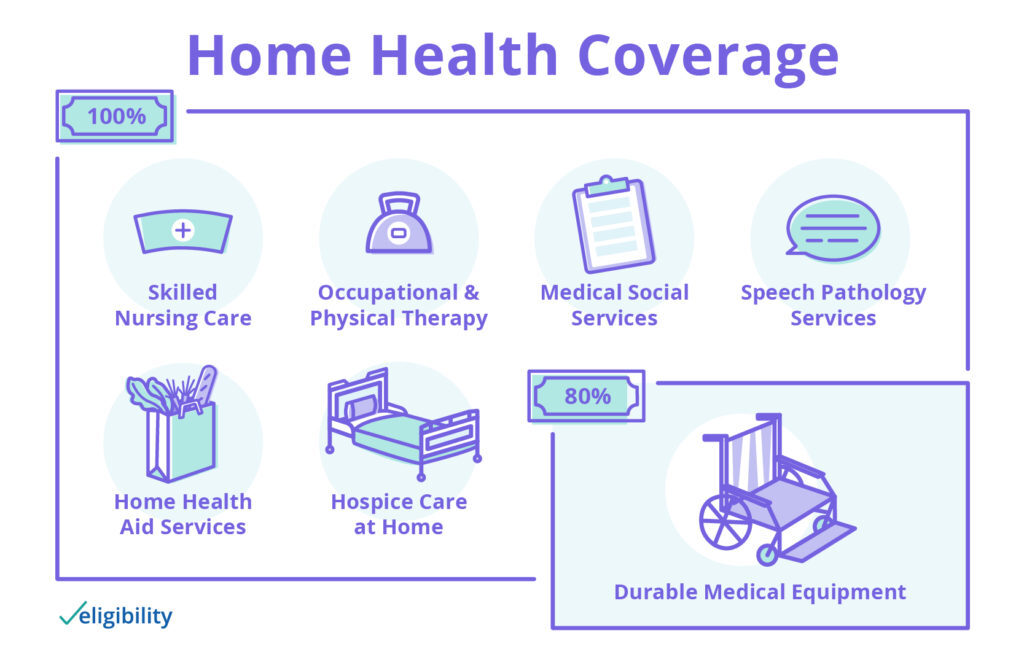
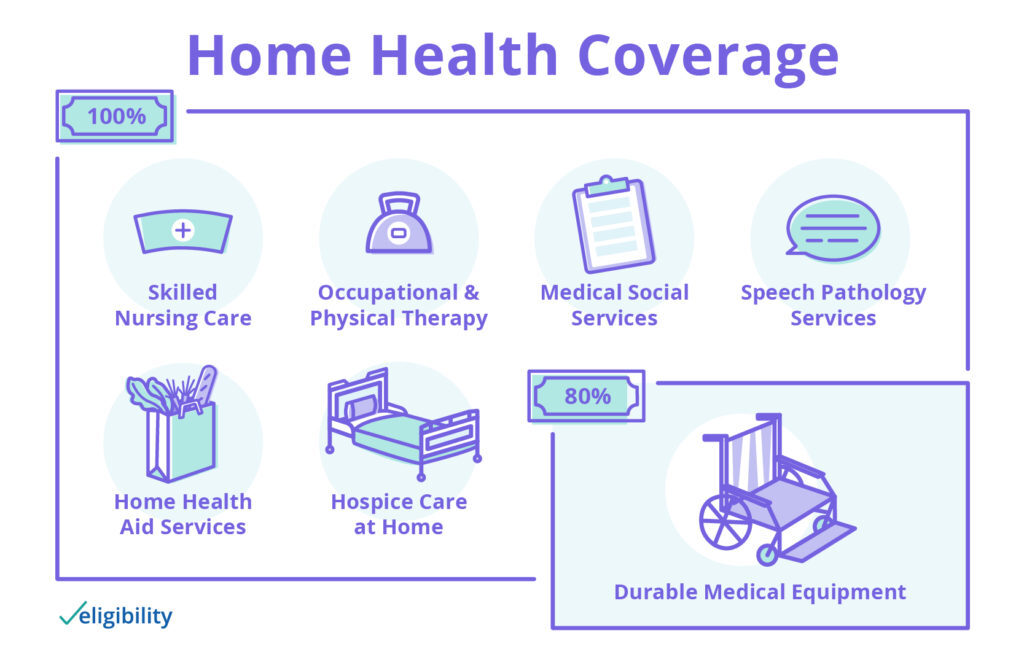
How Long Will Medicare pay for home health care?
To be covered, the services must be ordered by a doctor, and one of the more than 11,000 home health agencies nationwide that Medicare has certified must provide the care. Under these circumstances, Medicare can pay the full cost of home health care for up to 60 days at a time.
How much does it cost to cover a nursing home?
You can use your personal money and savings to pay for nursing home care. Some insurance companies let you use your life insurance policy to pay for long-term care. Contact your insurance provider for more information on what your private insurance covers.
How long does Medicare pay for skilled nursing?
Medicare Part A will help pay for skilled nursing care for up to 100 days at a time. Called a "benefit period," these benefits reset when you've stopped receiving skilled nursing care for 60 consecutive days. Your Part A benefits work like this: Medicare Part A pays all of your costs for the first 20 days.
What is Medicare Supplement?
A Medicare Supplement (Medigap) plan can help pay for your skilled nursing facility care costs, such as Medicare deductibles and coinsurance.
What is Medicare Part A?
Prescription drugs. Social services. Medical equipment and supplies. Counseling on your diet. Transportation via ambulance. Medicare Part A also covers intermittent skilled nursing care at home, but it is restrictive.
How does Medicare Part A work?
Your Part A benefits work like this: Medicare Part A pays all of your costs for the first 20 days. You pay nothing. For days 21-100, you are responsible for a daily $176 coinsurance in 2020. If you require skilled nursing care longer than 100 consecutive days, you are responsible for all costs.
How much is Part B coinsurance?
Your coinsurance will increase if you go beyond day 90. Part B coinsurance (20% of the Medicare-approved amount for most doctor services)
How many resources are there for senior care?
Finding Help With Senior Care - This comprehensive list of resources offers 300+ resources for finding help with senior care through private and government organizations and programs.
Does Medicare cover skilled nursing?
Medicare Part A also covers intermittent skilled nursing care at home, but it is restrictive.
What is SNF in Medicare?
Skilled nursing facility (SNF) care. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Care like intravenous injections that can only be given by a registered nurse or doctor. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services.
What services does Medicare cover?
Medicare-covered services include, but aren't limited to: Semi-private room (a room you share with other patients) Meals. Skilled nursing care. Physical therapy (if needed to meet your health goal) Occupational therapy (if needed to meet your health goal)
What is a benefit period?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF.
What is skilled nursing?
Skilled care is nursing and therapy care that can only be safely and effectively performed by, or under the supervision of, professionals or technical personnel. It’s health care given when you need skilled nursing or skilled therapy to treat, manage, and observe your condition, and evaluate your care.
How many days do you have to stay in a hospital to qualify for SNF?
Time that you spend in a hospital as an outpatient before you're admitted doesn't count toward the 3 inpatient days you need to have a qualifying hospital stay for SNF benefit purposes. Observation services aren't covered as part of the inpatient stay.
When does the SNF benefit period end?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. You must pay the inpatient hospital deductible for each benefit period.
How long do you have to be in the hospital to get SNF?
You must enter the SNF within a short time (generally 30 days) of leaving the hospital and require skilled services related to your hospital stay. After you leave the SNF, if you re-enter the same or another SNF within 30 days, you don't need another 3-day qualifying hospital stay to get additional SNF benefits.
How long does Medicare cover nursing home care?
What parts of nursing home care does Medicare cover? Medicare covers up to 100 days at a skilled nursing facility. Medicare Part A and Part B cover skilled nursing facility stays of up to 100 days for older people who require care from people with medical skills, such as sterile bandage changes.
How much does a nursing home cost?
On average, annual costs for nursing homes fall between $90,000 and $110,000, depending on whether you have a private or semi-private room. This can burn through your personal funds surprisingly quickly. It’s best to pair your personal funds with other financial aid to help you afford nursing home care.
What is covered by Medicare Advantage?
Some of the specific things covered by Medicare include: A semiprivate room. Meals. Skilled nursing care. Physical and occupational therapy. Medical social services. Medications. Medical supplies and equipment. However, if you have a Medicare Advantage Plan, it’s possible that the plan covers nursing home care.
How many days do you have to be in hospital to qualify for Medicare?
Having days left in your benefit period. Having a qualifying hospital stay of three inpatient days. Your doctor determining that you need daily skilled care.
Does Medicare cover dementia care?
Does Medicare cover nursing home care for dementia? Medicare only ever covers the first 100 days in a nursing home, so nursing home coverage is not significantly different for people with dementia. Medicaid can help cover memory care units and nursing home stays beyond 100 days, though. Can older people rely on Medicare to cover nursing home costs? ...
Does Medicare cover nursing home room and board?
It also doesn’t cover room and board for any long-term nursing home stay, including hospice care or the cost of a private room. Lastly, Medicare won’t cover your skilled nursing facility stay if it’s not in an approved facility, so it’s important to know what institutions it has approved in your area.
Does long term care insurance cover nursing home care?
Similar to regular health insurance, long-term care insurance has you pay a premium in exchange for financial assistance should you ever need long-term care. This insurance can help prevent you from emptying your savings if you suddenly find yourself needing nursing home care. However, it’s important to note that these policies often have a daily or lifetime cap for the amount paid out. When you apply, you can choose an amount of coverage that works for you.
How long do you have to stay in a nursing home to qualify for Medicare?
En español | To qualify for Medicare’s nursing home coverage, you must first have stayed in the hospital for at least three consecutive days as an admitted patient (not counting the day you leave). You must also need intravenous injections, physical therapy or other care from a skilled professional provider.
What is covered by nursing home insurance?
Nursing home coverage also includes a room you share with other patients, meals, medications, medical supplies and ambulance services to medical care that the facility doesn’t provide.
Does Medicare cover nursing home care?
It’s important to remember that Medicare does not cover nursing home care indefinitely and does not cover nonmedical or custodial care. Return to Medicare Q&A Tool main page >>.
How long does Medicare cover skilled nursing?
Traditional Medicare covers the first 100 days of skilled nursing with variable levels of coverage. For the first 20 days, Medicare will pay the qualified skilled nursing expenses in full ...
What is skilled nursing?
Skilled nursing is generally care provided to a person by nursing staff. This may sound redundant but it's important to clearly understand it. Such care may be the maintenance of IV's or physical therapy. In general, it's the next care level down from that provided under a direct doctor's supervision. In order to receive benefits under Medicare for skilled nursing, the practitioners and/or facility must be Medicare approved so make sure this is the case before proceeding especially with home based care. One note, skilled nursing is generally given to help you recover from a given situation (say following a surgery) or prevent a health condition from getting worse. It is generally considered short term based (up to 100 days with Medicare) and is not intended for custodial care. Custodial care is designed to help a person with everyday issues such as bathing, clothing, getting in/out of bed and the like if that's the only care that is needed. Custodial care falls under the heading of Long Term Care which is not covered under Medicare and requires other preparations such as purchasing a Long Term Care policy. Let's look at what Medicare considers to be "short term" when dealing with skilled nursing care.
Is long term care covered by Medicare?
Custodial care falls under the heading of Long Term Care which is not covered under Medicare and requires other preparations such as purchasing a Long Term Care policy. Let's look at what Medicare considers to be "short term" when dealing with skilled nursing care.
Do skilled nursing facilities need to be approved by Medicare?
In order to receive benefits under Medicare for skilled nursing, the practitioners and/or facility must be Medicare approved so make sure this is the case before proceeding especially with home based care.
Does Medicare extend days past 100?
A Medicare supplement does not extend your total # of days past the 100 mentioned which is important to understand for longer term care issues (again, Long Term Care comes into light here). Skilled nursing is increasingly a common way for facilities to reduce costs and free up bed space as a midway level of care.
How many nursing homes accept medicaid?
It is estimated that between 80% and 90% of nursing homes accept Medicaid depending on one’s state of residence. Search for Medicaid nursing homes here. While 80% to 90% sounds high, these percentages are very misleading. Nursing homes may accept Medicaid, but may have a limited number of “Medicaid beds”. “Medicaid beds” are rooms (or more likely shared rooms) that are available to persons whose care will be paid for by Medicaid. Nursing homes prefer residents that are “private pay” (meaning the family pays the cost out-of-pocket) over residents for whom Medicaid pays the bill. The reason for this is because private pay residents pay approximately 25% more for nursing home care than Medicaid pays. In 2021, the nationwide average private payer pays $255 per day for nursing home care while Medicaid pays approximately $206 per day.
How many states have Medicaid eligibility for nursing home care?
Medicaid Eligibility for Nursing Home Care. To be eligible for nursing home care, all 50 states have financial eligibility criteria and level of care criteria. The financial eligibility criteria consist of income limits and countable assets limits. These limits change annually, change with marital status, and change depending on one’s state ...
How to apply for medicaid for nursing home?
First, the applicant applies for Medicaid, which they can do online or at any state Medicaid office.
Why do nursing homes prefer private pay?
The reason for this is because private pay residents pay approximately 25% more for nursing home care than Medicaid pays.
How much will Medicaid pay in 2021?
In 2021, the nationwide average private payer pays $255 per day for nursing home care while Medicaid pays approximately $206 per day. Being Medicaid eligible and finding a Medicaid nursing home is often not enough to move a loved one in. Read about how to get into a nursing home .
What is a short term nursing home?
Short-term nursing homes are commonly called convalescent homes and these are meant for rehabilitation not long term care. Be aware that different states may use different names for their Medicaid programs. In California, it is called Medi-Cal. Other examples include Tennessee (TennCare), Massachusetts (MassHealth), and Connecticut (HUSKY Health).
Do you have to give Medicaid to a married couple?
Note for Married Couples – While a single nursing home Medicaid beneficiary must give Medicaid almost all their income for nursing home care, this is not always the case for married couples in which only one spouse needs Medicaid-funded nursing home care. There are Spousal Protection Laws, which protect income and assets for the non-applicant spouse to prevent spousal impoverishment. The Minimum Monthly Maintenance Needs Allowance permits applicant spouses to transfer a portion, or in some cases, all, of their monthly income to their non-applicant spouses to ensure they have sufficient income on which to live. (Up to $3,259.50 / month in 2021).There is also a Community Spouse Resource Allowance that protects a larger amount of a couple’s joint assets for non-applicant spouses. (Up to $130,380 in 2021).