If you receive dialysis at a Medicare-approved facility as an outpatient, Medicare Part B will cover 80 percent of the Medicare-approved cost, including doctor’s fees. You will be responsible for the other 20 percent of the cost of dialysis.
Is dialysis covered by Medicare?
Reimbursement for dialysis services If your Medicare Part A or Part B applies, you’ll pay 20% of Medicare-approved costs for covered services related to dialysis, which include self-dialysis procedures as well. Another 80% will be paid by Medicare.
Will Medicare pay for dialysis?
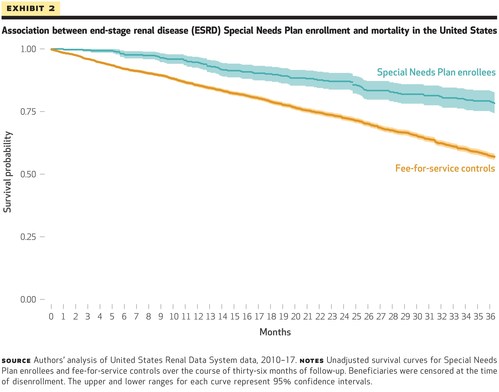
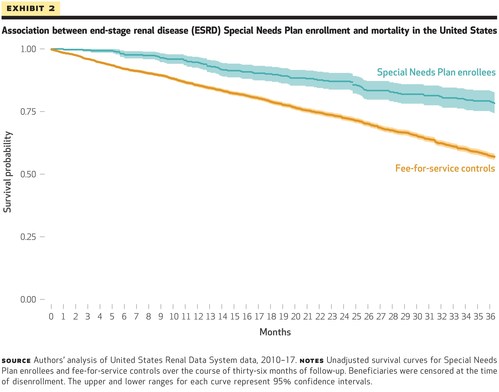
These services and models are part of a growing list of home-based medical care models that also includes in-home primary or palliative care, in-home dialysis, and paramedicine. Some are covered through traditional Medicare, and others are available only through Medicare Advantage plans.
What is the average cost of dialysis?
[318 Pages Report] According to a recent research study published by Future Market Insights, the global dialysis equipment market is projected to register a CAGR of 4.8% and will likely reach a valuation of US$ 23.6 Bn by 2028 end.
Does Medicare cover transportation to dialysis?
While Medicare does not cover transportation to dialysis, it generally provides coverage for certain treatments, medications and kidney transplant procedures. Transplant services covered by Medicare Part A include: Transplant services included by Medicare Part B include:
How Much Does Medicare pay per dialysis treatment?
Medicare costs for dialysis treatment and supplies If you have Original Medicare, you'll continue to pay 20% of the Medicare-approved amount for all covered outpatient dialysis-related services, including those related to self-dialysis. Medicare will pay the remaining 80%.
Is there a copay for dialysis?
Part B covers dialysis overseen in a Medicare-approved outpatient dialysis facility. You will typically pay a 20% coinsurance for the cost of each session, which includes equipment, supplies, lab tests, and most dialysis medications.
What is included in the Medicare dialysis bundle?
The ESRD PPS is a “dialysis bundled payment” made to a dialysis facility on behalf Medicare beneficiaries for their treatment. The “Dialysis Bundle” includes the dialysis treatment, laboratory tests, supplies, all injectable drugs, biologicals and their oral equivalent, and services provided for the dialysis treatment.
How frequently are dialysis services usually billed?
The rule of thumb is that for any month that the patient is a home dialysis patient for even a single day, they are a home patient for the entire month. So, for the example given the practice should bill all four months as a home patient using the age-based home dialysis codes (CPT codes 90963-90966).
How much is a session of dialysis?
Although federal health insurance covers the majority of dialysis costs, 20% still falls to the patient. For patients without health insurance, dialysis is an even bigger expense. One dialysis treatment generally costs around $500 or more.
How much is a dialysis treatment out of pocket?
For patients not covered by health insurance, a single hemodialysis treatment typically costs up to $500 or more -- or, about $72,000 or more per year for the typical three treatments per week. Injectable medications and vitamins can add hundreds of dollars to the cost, depending on what is prescribed.
What benefits are dialysis patients entitled to?
The Social Security Administration (SSA) offers two types of disability benefit programs that you may be eligible for. Social Security disability benefits for kidney dialysis patients are available. To qualify for disability, you need to meet the SSA's Blue Book listing for dialysis.
How long is a dialysis session?
Often, you'll visit a special center for dialysis about three times a week. Each session lasts three to four hours. Or, you may be able to do dialysis right at home three times a week or even daily. Home sessions are shorter, about 2 to 3 hours, and they're easier for your body to tolerate.
Can kidneys start working again after dialysis?
Acute kidney failure requires immediate treatment. The good news is that acute kidney failure can often be reversed. The kidneys usually start working again within several weeks to months after the underlying cause has been treated. Dialysis is needed until then.
What physician services are included in the codes during a dialysis month?
ESRD-related services by a physician or other qualified health care professional include establishment of a dialyzing cycle, outpatient evaluation and management of the dialysis visits, telephone calls, and patient management during the dialysis provided during a full month.
What is a code dialysis?
The Current Procedural Terminology (CPT) code range for Dialysis Services and Procedures 90935-90999 is a medical code set maintained by the American Medical Association.
What is the bill type for dialysis claims?
Dialysis. Dialysis facilities must bill on a UB-04 claim form using an outpatient bill type. Reimbursement is based on the revenue codes billed to define the type of dialysis treatment rendered.
Does Medicare Pay for Dialysis Patients Who Receive Home Dialysis Treatment?
Yes. Medicare will typically cover your home dialysis treatments if you or a loved one live with kidney failure. Dialysis treatments are often time...
What Supplies Do You Need for Home Dialysis?
There are different kinds of home dialysis, and each uses different equipment to remove toxins from your bloodstream. While there are differences b...
What are the different kinds of home dialysis?
There are two main types of home dialysis: Peritoneal Dialysis and Home Hemodialysis. Medicare will typically cover whichever form your doctor pres...
Who performs at-home dialysis treatments?
Medicare dialysis coverage does not pay for nurses or doctors to administer your treatments. Instead, it will pay to train someone to aid in your c...
How Much Does Dialysis at Home Cost With Medicare?
As a starting point, Medicare Part B covers home dialysis supplies. This is the portion of Original Medicare that helps pay for medical services an...
How long does Medicare pay for dialysis?
If you’re a Medicare beneficiary that’s 65 or older, Medicare will pay for your home dialysis and supplies as long as your doctor deems them medica...
What is the average cost of a dialysis treatment?
According to the Centers for Disease Control (CDC), Medicare pays an average of $80,000 each year for beneficiaries with kidney failure. After acco...
How Much Does Dialysis Cost Out of Pocket?
Still asking, “How much does Medicare pay for dialysis?” It’s best to know how Medicare calculates your costs because it will help you make sense o...
Is End Stage Renal Disease Covered by Medicare?
End Stage Renal Disease occurs when your kidneys can no longer function enough to meet your body’s needs. With ESRD, toxins and fluids can build up...
How much does Medicare pay for dialysis?
Once you pay your Part B deductible ( $203 per year in 2021), Medicare pays 80 percent of the monthly amount of your inpatient dialysis treatments, and you pay the remaining 20 percent coinsurance. If you get services for less than one month, your doctor may be paid per day.
What is covered by Medicare for self-dialysis?
Certain drugs for self-dialysis. Medicare Part B covers some drugs used in self-dialysis, including heparin and topical anesthetics (when medically necessary). ESRD-related drugs that only have an oral form of administration are only covered by Medicare Part D and Medicare SNPs. Medicare Part D plans (also known as Medicare Prescription Drug Plans) ...
How old do you have to be to get Medicare for ESRD?
To qualify for Medicare coverage of ESRD, you must: Be under the age of 65 and diagnosed with ESRD by a doctor. Have enough work history to qualify for Social Security Disability Insurance or Social Security Retirement Benefits or enough work history to qualify for benefits through the Railroad Retirement Board.
Does Medicare cover dialysis?
All Medicare Advantage plans include an annual out-of-pocket spending limit, and most plans include prescription drug coverage, both of which Original Medicare doesn’t cover.
Is end stage renal disease covered by Medicare?
Is End-Stage Renal Disease covered by Medicare Advantage? People with ESRD may qualify for Medicare, a Medicare Advantage plan or a Medicare Special Needs Plan (SNP). A Medicare SNP is a type of Medicare Advantage plans that helps cover people with specific characteristics or diseases, including ESRD. These plans tailor benefits, provider choices, ...
When does Medicare start covering kidney transplants?
Medicare coverage can begin the month you’re admitted to a Medicare-certified hospital for a kidney transplant (or for health care services that you need before your transplant) if your transplant takes place in that same month or within the next 2 months.
When does Medicare start ESRD?
When you enroll in Medicare based on ESRD and you’re on dialysis, Medicare coverage usually starts on the first day of the fourth month of your dialysis treatments. For example, if you start dialysis on July 1, your coverage will begin on October 1.
How much is Part B insurance?
Most people must pay a monthly premium for Part B. The standard Part B premium for 2020 is $144.60 per month, although it may be higher based on your income. Premium rates can change yearly.
What is assignment in Medicare?
Assignment—An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare cover home dialysis?
Medicare Part B covers training for home dialysis, but only by a facility certifed for dialysis training. You may qualify for training if you think you would benefit from home dialysis treatments, and your doctor approves. Training sessions occur at the same time you get dialysis treatment and are limited to a maximum number of sessions.
Does Medicare cover dialysis for children?
Your child can also be covered if you, your spouse, or your child gets Social Security or RRB benefits, or is eligible to get those benefits.Medicare can help cover your child’s medical costs if your child needs regular dialysis because their kidneys no longer work, or if they had a kidney transplant.Use the information in this booklet to help answer your questions, or visit Medicare.gov/manage-your-health/i-have-end-stage-renal-disease-esrd/children-end-stage-renal-disease-esrd. To enroll your child in Medicare, or to get more information about eligibility, call or visit your local Social Security oce. You can call Social Security at 1-800-772-1213 to make an appointment. TTY users can call 1-800-325-0778.
Does Medicare cover pancreas transplant?
If you have End-Stage Renal Disease (ESRD) and need a pancreas transplant, Medicare covers the transplant if it’s done at the same time you get a kidney transplant or it’s done after a kidney transplant.
How long does it take for Medicare to stop paying for dialysis?
Beneficiaries receiving Medicare only because of ESRD will stop receiving benefits either: 12 months after the month you end dialysis treatments.
How much does Medicare pay for kidney failure?
According to the Centers for Disease Control (CDC), Medicare pays an average of $80,000 each year for beneficiaries with kidney failure. After accounting for the portion paid by Medicare Part B, the remaining 20% averaged out to $16,000 per Medicare beneficiary needing dialysis treatments.
What is Medicare Part B?
Medicare Part B#N#Medicare Part B is the portion of Medicare that covers your medical expenses. Sometimes called "medical insurance," Part B helps pay for the Medicare-approved services you receive.#N#helps cover home dialysis supplies, including dialysis machines, water purifiers, and some medical supplies.
What is the Medicare deductible for 2021?
In 2021, the Part B deductible is $203. Premium: This is the monthly cost of Part B. You must pay your monthly Part B premium to have active Part B coverage.
How long does dialysis training last?
For example, spouses and other loved ones can learn how to help administer your home dialysis treatments. The training periods can last 10 to 12 hours per day for several weeks.
Does Medicare cover kidney failure?
This typically includes a bundle of Original Medicare (Parts A and B) and Medicare Prescription Drug Plan (Part D). can now cover the treatments for ESRD, or kidney failure, and may have different costs than Original Medicare’s Part B. Medicare will also help pay for you and/or another person to receive the training needed to perform your at-home ...
Can you do dialysis at night?
You can administer either treatment during the day or night at your doctor’s recommendation. Each uses different equipment, and the length of your treatments depends on your specific health needs. Talk to your doctor to find out what kind of home dialysis is in your care plan.
When does Medicare start covering dialysis?
Medicare coverage will take effect depending on the route of treatment. If you’re a Hemodialysis patient, coverage will start in your 4th month of dialysis. When you’re a home dialysis patient, Medicare is active in the first month of treatment.
How many sessions does Medicare cover for peritoneal dialysis?
In further detail, Medicare will cover up to 15 dialysis training sessions for peritoneal dialysis and pay for up to 25 dialysis sessions for hemodialysis.
How much does hemodialysis cost?
Just one year of hemodialysis may cost you $72,000. And a single year of peritoneal dialysis can cost you around $53,000 each year. Keep in mind, Medicare will only cover 80%, you’ll be left with the remaining costs. Even with the majority of your treatment covered, you’ll still have costly bills.
Does Medicare cover medical equipment?
Medicare will cover a range of treatments, including tests, medications, and equipment. We know how important it is to understand your coverage. You need to know what isn’t covered just as much as you need to know what is covered. Below we’ll review how Medicare works with each treatment you may need. Then, you can make decisions ...
Can you get dialysis at home?
You can get dialysis in several different types of facilities. If you qualify, your dialysis can take place within the comforts of your own home. Or, you can also get dialysis at a certified dialysis center. For Medicare to cover your treatment, though, the center must be Medicare-certified.
Does Medicare cover ambulance transportation?
Your doctor will need to specify that transportation is medically necessary. Often, Medicare Advantage plans will cover transportation services too.
Does Medicare cover dialysis?
Yes, Medicare will cover you should you need dialysis treatments. Dialysis can come in many different forms. Below we’ll go over different types of dialysis treatments that have coverage.
There Is Reason For Policymakers To Act
Steering Medicare beneficiaries into the individual market would likely raise individual market premiums and increase the federal cost of subsidizing individual market coverage more than it reduced costs to the Medicare program, write the authors.
Medicare Advantage Plans Esrd And Dialysis Coverage
Generally, you cannot enroll in a Medicare Advantage plan if you have already been diagnosed with end-stage renal disease. But there are two prominent exceptions.
Does Medicare Pay For Dialysis Patients Who Receive Home Dialysis Treatment
Yes. Medicare will typically cover your home dialysis treatments if you or a loved one live with kidney failure. Dialysis treatments are often time-consuming and can leave a patient exhausted. Receiving this treatment at home can ease the physical burden on the patient while eliminating the need to travel to regular appointments for care.
Health Services Covered Under Esrd Medicare
If a Medicare beneficiary requires dialysis, the federal Medicare program covers various dialysis services, including:
Medicare And Chronic Kidney Disease
Medicare is a federally funded health insurance program for Americans over age 65 and people who have been deemed disabled. In 1972, people requiring dialysis became newly entitled to this health benefit. The law was amended in order to provide coverage to people who may have forgone treatment due to the high costs of dialysis treatment.
Find Help With Dialysis Costs Today
There is no question that dialysis treatment is expensive, but that doesnt mean it should put a financial barrier between you and the care you need. Through crowdfunding, its possible to afford dialysis so you can focus your time and energy on your health. Tell your story and share your fundraiser to your close network and beyond.
Is Dialysis Covered Under Medicare Part A Or B
Medicare Part A covers the costs of dialysis if you have the treatment at an inpatient facility. You are responsible for paying the Part A deductible, which is $1,484 as of 2021.
What does Azar say about dialysis?
It is the epitome of a system that pays for sickness rather than health, and [the Trump] administration is intent on shifting these priorities.". In addition, Azar said, "In many ways, today's policies bias providers toward center-based dialysis" over kidney care alternatives, such as home-based dialysis. Further, Azar said dialysis centers ...
Who is the CEO of the National Kidney Foundation?
National Kidney Foundation CEO Kevin Longino praised Azar's focus on improving kidney care. He said HHS is "clearly charting a path towards making progress in prevention, early detection, treatment, research, and access to transplantation; all critical issues for kidney patients, and they are doing this in a strategic, thoughtful, ...
Do dialysis centers have incentives?
Further, Azar said dialysis centers currently have no incentive to help patients find or prepare for transplants, as such procedures could eliminate patients' need for dialysis care, and therefore mean dialysis centers could see fewer patients.