
How to appeal a higher Medicare Part B premium?
Mar 02, 2022 · If you disagree with a Medicare decision regarding your Part B coverage, you can appeal. If you decide to appeal Medicares decision, first ask your healthcare provider or insurance carrier for any information that can help your case. Look at your Medicare Summary Notice . It will list all of your billed services and supplies for a 90-day period.
How to avoid the Medicare Part B late penalty?
If you were without Part B or job-based insurance for more than 12 months while eligible for Medicare, you may face a Part B late enrollment penalty (LEP). The penalty is 10% of the Part B premium ($170.10 in 2022) for every 12-month period you did not have Part B or job-based insurance that allowed you to delay enrollment.
How much is the late enrollment penalty for Part B?
You waited to sign up for Part B until March 2019 during the General Enrollment Period. Your coverage starts July 1, 2019. Your Part B premium penalty is 20% of the standard premium, and you’ll have to pay this penalty for as long as you have Part B. (Even though you weren't covered a total of 27 months, this included only 2 full 12-month ...
Who is eligible for Medicare Part B premium reimbursement?
Apr 27, 2020 · How do I appeal a Medicare Part B penalty? You’ll want to document as much information as possible about when someone from the government told you not to take Part B. This can include the date and time of your conversation or phone call, the name of the person you spoke with, and what you did as a result of the information you were given.
How do I get rid of Medicare Part B penalty?
You may qualify to have your penalty waived if you were advised by an employee or agent of the federal government – for example by Social Security or 1-800-MEDICARE – to delay Part B. Asking for the correction is known as requesting equitable relief.Apr 27, 2020
How do I appeal a Medicare Part B premium?
First, you must request a reconsideration of the initial determination from the Social Security Administration. A request for reconsideration can be done orally by calling the SSA 1-800 number (800.772. 1213) as well as by writing to SSA.
Is there a cap on Medicare Part B penalty?
Is There a Cap on the Medicare Part B Penalty? As of now, there is no cap on the Part B late enrollment penalty. However, if passed, the Medicare Part B Fairness Act or H.R. 1788 would cap the penalty amount at 15% of the current premium, regardless of how many 12-month periods the beneficiary goes without coverage.
Can LEP be removed?
Eliminating the Part D LEP For most people, you have to pay the LEP as long as you are enrolled in the Medicare prescription drug benefit. There are some exceptions: If you receive Extra Help, your penalty will be permanently erased. If you are under 65 and have Medicare, your LEP will end when you turn 65.
How do I dispute a Medicare charge?
Fill out a "Redetermination Request Form [PDF, 100 KB]" and send it to the company that handles claims for Medicare. Their address is listed in the "Appeals Information" section of the MSN. Or, send a written request to company that handles claims for Medicare to the address on the MSN.
How do I appeal Part B Irmaa?
Even if you haven't experienced a life-changing event, you can still appeal an IRMAA. Request an appeal in writing by completing a request for reconsideration form. To get an appeal form, you can go into a nearby Social Security office, call 800-772-1213, or check the Social Security website.
How is the Part B penalty calculated?
Part B late penalties are calculated as an extra 10 percent for each full 12-month period when you should have had Part B but didn't. If you should have signed up at age 65, the penalty calculation is made on the time that elapsed between the end of your IEP and the end of the GEP in which you finally sign up.
Are you automatically enrolled in Medicare if you are on Social Security?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
Can you drop Medicare Part B anytime?
You can voluntarily terminate your Medicare Part B (medical insurance). However, since this is a serious decision, you may need to have a personal interview. A Social Security representative will help you complete Form CMS 1763.Nov 24, 2021
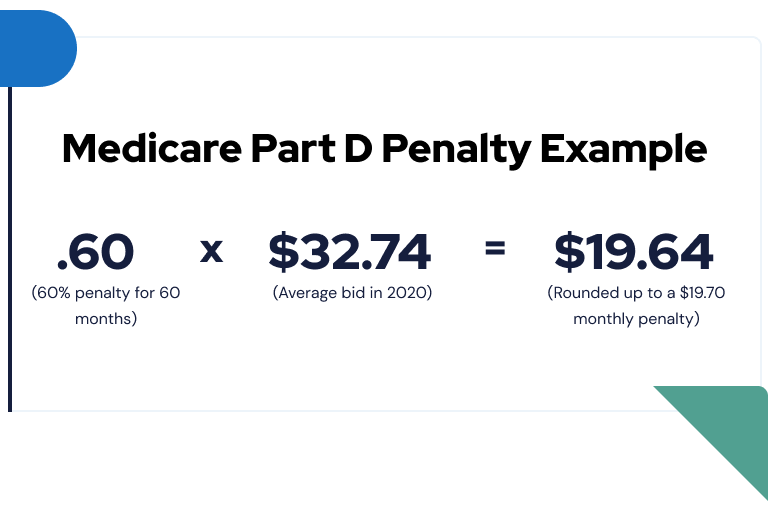
What is the Part D penalty?
Medicare calculates the penalty by multiplying 1% of the "national base beneficiary premium" ($33.37 in 2022) times the number of full, uncovered months you didn't have Part D or creditable coverage. The monthly premium is rounded to the nearest $. 10 and added to your monthly Part D premium.
What is the LEP penalty?
The late enrollment penalty (also called the “LEP” or “penalty”) is an amount that may be added to a person's monthly premium for Medicare drug coverage (Part D).
How to request reconsideration of Social Security?
A request for reconsideration can be done orally by calling the SSA 1-800 number (800.772.1213) as well as by writing to SSA .
What is a work stoppage?
Work stoppage. Loss of income from income producing property. Loss or reduction of certain kinds of pension income. Events that result in the loss of dividend income or affect a beneficiary's expenses, but do not affect the beneficiary's modified adjusted gross income are not considered qualifying life-changing events.
What are the life changing events?
There are 7 qualifying life-changing events: 1 Death of spouse 2 Marriage 3 Divorce or annulment 4 Work reduction 5 Work stoppage 6 Loss of income from income producing property 7 Loss or reduction of certain kinds of pension income
What happens if you don't get Part B?
If you didn't get Part B when you're first eligible, your monthly premium may go up 10% for each 12-month period you could've had Part B, but didn't sign up. In most cases, you'll have to pay this penalty each time you pay your premiums, for as long as you have Part B.
When does Part B start?
You waited to sign up for Part B until March 2019 during the General Enrollment Period. Your coverage starts July 1, 2019. Your Part B premium penalty is 20% of the standard premium, and you’ll have to pay this penalty for as long as you have Part B.
What is the late enrollment penalty for Medicare Part B?
Medicare Part B enrollment is complicated, and the wrong decision can leave you without health coverage for months – and lead to lifetime premium penalties. Part B premiums increase 10 percent for every 12-months you were eligible for Part B but not enrolled.
Can I get a Part B penalty waived?
People make Medicare enrollment errors for a variety of reasons, and equitable relief is not available for all of them.
How do I appeal a Medicare Part B penalty?
You’ll want to document as much information as possible about when someone from the government told you not to take Part B. This can include the date and time of your conversation or phone call, the name of the person you spoke with, and what you did as a result of the information you were given.
How long does Medicare late enrollment last?
Overview. Medicare beneficiaries may incur a late enrollment penalty (LEP) if there is a continuous period of 63 days or more at any time after the end of the individual's Part D initial enrollment period during which the individual was eligible to enroll, but was not enrolled in a Medicare Part D plan and was not covered under any creditable ...
How long does Medicare Part D last?
A Medicare Part D plan notifies an enrollee in writing if the plan determines the enrollee has had a continuous period of 63 days or more without creditable prescription drug coverage at any time following his or her initial enrollment period for the Medicare prescription drug benefit.
What happens if you disagree with an ALJ?
If you disagree with the ALJ or attorney adjudicator decision, or you wish to escalate your appeal because the OMHA adjudication time frame passed, you may request a Council review. The Council is part of the HHS Departmental Appeals Board (DAB).
What does "I" mean in CMS?
In a 2019 Final Rule, CMS ended the requirement that appellants sign their appeal requests.In this booklet, “I” or “you” refers to patients, parties, and appellants active in an appeal.
Can a patient transfer their appeal rights?
Patients may transfer their appeal rights to non-participating providers or suppliers who provide the items or services and don’t otherwise have appeal rights. To transfer appeal rights, the patient and non-participating provider or supplier must complete and sign the
How much will Medicare Part B cost in 2021?
In 2021, Medicare Part B costs $148.50 for new enrollees. This is the rate that most people pay. Those in the highest income bracket can pay more considerably more than that. Social Security determines what you will pay based on your modified adjusted gross income (MAGI) as reported to the IRS. If you owe a higher premium, Social Security calls ...
How much is Part B deductible in 2021?
In return for covering a small, once annual Part B deductible ($203 in 2021) you can sometimes find premiums as much as $250 lower than a Plan F. That keeps money in your pocket. Medigap plans L, M, N and High Deductible F are also great solutions for high income individuals.
What is MAGI on SSA-44?
Your MAGI amount is made up of your total adjusted gross income plus any tax-exempt interest income. (The Form SSA-44 has instructions which explain which line numbers from your IRS Tax return that you will use to calculate this number).
How much is IRMAA 2021?
Right now in 2021, Part D premiums range from around $7 to over $180/month, depending on where you live. (For more on finding the right Part D plan, visit our pages about Part D .)
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
What to do if you decide to appeal a health insurance plan?
If you decide to appeal, ask your doctor, health care provider, or supplier for any information that may help your case. See your plan materials, or contact your plan for details about your appeal rights.
How many levels of appeals are there?
The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal.
