
- Some denials can be adjusted via telephone reopening
- You may submit your appeal request in writing or through our website using eServices
- Railroad Medicare also accepts redetermination requests via fax at (803) 462-2218
- First level of appeal: redetermination. ...
Full Answer
Where to submit railroad Medicare claims?
• Call Palmetto GBA Railroad Medicare toll-free at 1-800-833-4455. If you are hearing impaired, you can call (877) 566-3572. • Call the Railroad Retirement Board’s automated system at 1-800-808-0772. • Submit an Online Service Request on the RRB website www.RRB.gov.
How to file for Medicare Appeals?
You can file an appeal if you disagree with a coverage or payment decision made by one of these:
- Medicare
- Your Medicare health plan
- Your Medicare drug plan
How to bill Medicare Railroad claims?
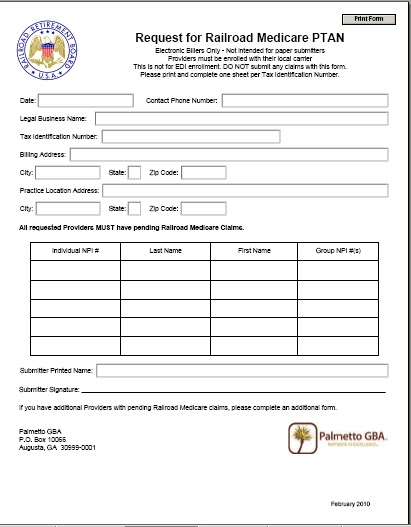
- Before filing claims electronically to Railroad Medicare, you must have an EDI enrollment packet on file with Palmetto GBA. ...
- View the Electronic Filing Instructions
- Palmetto GBA Interactive CMS-1500 Claim Form Instructions — This resource can also be helpful to providers who submit electronic claims. ...
What are Medicare appeals process?
There are five levels in the Medicare claims appeal process:
- Level 1: Your Health Plan. If you disagree with a Medicare coverage decision, you may request your health plan to redetermine your claim.
- Level 2: An Independent Organization. ...
- Level 3: Office of Medicare Hearings and Appeals (OMHA). ...
- Level 4: The Medicare Appeals Council. ...
- Level 5: Federal Court. ...
How do I appeal a railroad Medicare claim?
You may submit your appeal request in writing or through our website using eServices. Railroad Medicare also accepts redetermination requests via fax at (803) 462-2218. First level of appeal: redetermination. Timeframe: 120 days from the receipt of the initial determination.
What are the five levels for appealing a Medicare claim?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
How do I contact Railroad Medicare?
Contact Railroad MedicareProvider Contact Center: 888-355-9165.IVR: 877-288-7600.TTY: 877-715-6397.
How do I appeal a Medicare rejection?
Fill out a "Redetermination Request Form [PDF, 100 KB]" and send it to the company that handles claims for Medicare. Their address is listed in the "Appeals Information" section of the MSN. Or, send a written request to company that handles claims for Medicare to the address on the MSN.
How successful are Medicare appeals?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
Can providers appeal denied Medicare claims?
If you disagree with a Medicare coverage or payment decision, you can appeal the decision. Your MSN contains information about your appeal rights. If you decide to appeal, ask your doctor, other health care provider, or supplier for any information that may help your case.
Is there a difference between Medicare and railroad Medicare?
A: The only difference is that retired railroad beneficiaries have their Part B benefits administered by the Palmetto GBA Railroad Retirement Board Specialty Medicare Administrative Contractor (RRB SMAC) regardless of where they live. Members should be certain to advise providers of this when they receive treatment.
How do I find my railroad Medicare claims?
If you'd like to use the IVR, you can do so by calling 800–833–4455. From the main menu, press one (1) for claim status. You will need your Railroad Medicare number, date of birth, name, and date of service for the claim you are searching for. Claim status is available Monday thru Friday from 7 a.m. through 11 p.m. ET.
What is Federal railroad Medicare?
The Medicare program covers railroad workers just like workers under social security. Railroad retirement payroll taxes include a Medicare hospital insurance tax just like social security payroll taxes.
How do I write a Medicare appeal letter?
The Medicare appeal letter format should include the beneficiary's name, their Medicare health insurance number, the claim number and specific item or service that is associated with the appeal, dates of service, name and location of the facility where the service was performed and the patient's signature.
What happens if Medicare denies a claim?
If Medicare denies payment of the claim, it must be in writing and state the reason for the denial. This notice is called the Medicare Summary Notice (MSN) and is usually issued quarterly. Look for the reason for denial. coverage rule), it must be stated on the notice.
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
Call 888-355-9165, select Option 5 for Customer Service
Representatives are available Monday through Friday from 8:30 a.m. to 4:30 p.m. for all time zones with the exception of PT, which receives service from 8 a.m. to 4 p.m.
Telephone Reopenings
Some denials can be adjusted via telephone reopening (restrictions apply.) To request a claim reopening by telephone:
Submit Documentation
If you are unable to submit your appeals via our eServices portal , please submit your completed appeals forms and documentation using one of the methods noted below:
Contact a Different Department
View our main Contact Us page for information on how to submit a general inquiry or to contact a different department.
Your Opinion Matters
Please take a moment to complete our Redetermination – 1st level appeal survey. These questions are only related to your 1st level of appeals, the Redetermination.
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
What to do if you didn't get your prescription yet?
If you didn't get the prescription yet, you or your prescriber can ask for an expedited (fast) request. Your request will be expedited if your plan determines, or your prescriber tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function.
How long does Medicare take to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 calendar days. Payment request—60 calendar days. Learn more about appeals in a Medicare health plan.
How to ask for a prescription drug coverage determination?
To ask for a coverage determination or exception, you can do one of these: Send a completed "Model Coverage Determination Request" form. Write your plan a letter.
How long does it take for a Medicare plan to make a decision?
The plan must give you its decision within 72 hours if it determines, or your doctor tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function. Learn more about appeals in a Medicare health plan.
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
What is Medicare Part A?
Hospital Insurance ( Medicare Part A ), which helps pay for inpatient care in hospitals and skilled nursing facilities (following a hospital stay), some home health care services, and hospice care.
What is the enrollment period for Medicare?
Special Enrollment Period for People Covered Under a Group Health Plan#N#If you are age 65 or older and covered under a group health plan, either from your own or your spouse’s current employment, you have a special enrollment period in which to sign up for Medicare Part B. This means that you may delay enrolling in Medicare Part B without having to wait for a general enrollment period and paying the 10 percent premium surcharge for late enrollment. The special enrollment period rules allow you to: 1 enroll in Medicare Part B anytime while you are covered under the group health plan based on current employment; or 2 enroll in Medicare Part B during the 8-month period that begins the month after your group health coverage ends or employment ends, whichever comes first.
What is the RRB?
The Railroad Retirement Board (RRB) enrolls railroad retirement beneficiaries in the program, deducts Medicare premiums from monthly benefit payments, and assists in certain other ways.
What is the deductible for hospital care in 2021?
In 2021, the hospital insurance deductible amount is $1,484. If you receive medical services from a doctor, you pay a yearly deductible amount as well as a coinsurance amount for each visit. In 2021, the medical insurance deductible is $203.
What age does Medicare cover?
Medicare is our country’s health insurance program for people age 65 or older, certain people with disabilities who are under age 65, and people of any age who have permanent kidney failure.
How long does it take to enroll in medical insurance?
Initial Enrollment Period for Medical Insurance. When you first become eligible for hospital insurance (Part A), you have a 7-month period to sign up for medical insurance (Part B). This is called your initial enrollment period. A delay on your part may cause a delay in coverage and result in higher premiums.
Does Medicare cover railroad workers?
The Medicare program covers railroad workers just like workers under social security. Railroad retirement payroll taxes include a Medicare hospital insurance tax just like social security payroll taxes. Though you’re paying into the Medicare program during your working years, and will probably rely on its services in the future, ...
Provider Contact Center: 1-888-355-9165
Call the Provider Contact Center (PCC) to speak with representatives in Customer Service, Provider Enrollment, Electronic Data Interchange, eServices and Telephone Reopenings.
Interactive Voice Response (IVR): 1-877-288-7600
Use the IVR to request routine claim status, beneficiary eligibility, and payment information and to request a duplicate remittance advice.
Email Us
Use our contact form to submit general inquiries or to provide feedback on our website. For security reasons please do not submit requests involving PHI/PII with this form.
Contact Palmetto GBA Departments
For information on contacting a specific department by phone, email, fax, or for instructions on submitting documentation by mail, please select a department:
Feedback to the Railroad Retirement Board (RRB)
If you would like to send any feedback to the RRB regarding your experience with Palmetto GBA, please direct your comments to: [email protected] .
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
